What is already known on this subject?
- VILI originates from the interchange of energy, or mechanical power between the ventilator and the lung parenchyma, among other factors.
- Mechanical power is also associated with ICU mortality, 30-day mortality, and with days free of mechanical ventilation, even with a low tidal volume; high mechanical power (MP) was also associated with in-hospital mortality.
- A mechanical power greater than 17 Jules/min results in a constantly increasing risk as reported in the literature.
What does this study contribute?
- This study evaluates the clinical outcomes related to mechanical power in patients ventilated for different causes, including patients with SARS-CoV-2 infection in the context of the pandemic.
- Notwithstanding some knowledge gaps, there is evidence that mechanical power variables should be managed with caution to provide safe mechanical ventilation and deliver less energy or mechanical power transmission to the already injured lung parenchyma during each breath, thus avoiding the exponential increase in VILI.
INTRODUCTION
Acute respiratory failure is one of the main reasons for admission to the intensive care unit (ICU), and mechanical ventilation is the approach to maintain respiratory function and until the patient's clinical condition resolves.1 The principles of mechanical ventilation are to improve gas exchange, decrease the patient's respiratory work, and buy time while re-establishing respiratory and systemic physiology. The decision to ventilate a patient will depend on multiple factors1 and has precise indications. Mechanical ventilation is prescribed to achieve therapeutic goals and it requires monitoring and control to limit any potential deleterious effects, which are included in the concept of ventilator-induced lung injury (VILI).2,3
In addition to the mechanism responsible for the injury, the heterogeneity of the sick lung must be considered, which determines the presence of regional variations with collapsed or occupied alveolar units and distended alveolar regions, subjecting certain pulmonary areas to greater stress and cyclical collapse.
The determinants of VILI include delivered pressures, volume, and flow, as well as the times these variables are administered per unit of time.4 It has been argued that VILI depends on the amount of energy per minute delivered to the lung by the ventilator measured in Joules, which is called mechanical power.2)(5)(6 The energy is used mainly to overcome airway resistance and to expand the chest wall; such energy may also lead to cell damage.7-9
Our objective was to describe the value of mechanical power in patients with SARS-CoV-2 infection and ventilated for other causes and its relationship with days of mechanical ventilation, ICU length of stay and mortality, in patients receiving mechanical ventilation in a volume-controlled mode for more than 24 hours in three ICU in the city of Pereira, between July and August 2020. As a secondary objective, the demographic, clinical and ventilatory parameters used in the study subgroups are described.
METHODS
Multicenter, analytical cohort observational study. The protocol of this study was approved by the Ethics Committee of Universidad Tecnológica de Pereira under number 04-010620 dated June 4, 2020. This study includes patients admitted to the ICU of three institutions: Hospital Universitario San Jorge, Clínica Los Rosales, and Clínica Comfamiliar in Pereira - Colombia, between July 1 and August 31, 2020; the patients required invasive ventilatory support in a volume-controlled mode for more than 24 hours. Convenience sampling was used including all hospitalized patients in the study centers that met the inclusion criteria.
We included patients older than 18 years, with mechanical ventilation in a volume-controlled mode for more than 24 hours. Patients were excluded if they had a history of exposure to mechanical ventilation in the previous 30 days, pregnant women, patients with mechanical ventilation in modes other than volume controlled, and duplicate or incomplete medical records.
The data were collected by the study authors and collaborators between July and August 2020 using a written information collection form (Complementary material 1) and obtaining data from the electronic medical record. The mechanical ventilation monitoring sheet of each institution was reviewed to obtain the ventilatory parameters. For the calculation of mechanical power, two measurements were taken to produce the data and as input for the equation. Measurements were taken at the time of intubation and at the start of mechanical ventilation in the patients; the second measurement was recorded 24 hours after the first measurement. The measurements were taken by a respiratory therapist or a physiotherapist experienced in adult respiratory critical care, in accordance with the protocol described under Complementary material 2.
The following variables were recorded: demographics (age, sex, previous diseases), need for inotropic support and renaltherapy, diagnoses, vital signs, ICU severity scores (APACHE II and SOFA) measured during ICU admission. Ventilatory parameters including tidal or tidal volume (Vt), Positive end-expiratory pressure (PEEP), maximum or peak pressure (Ppeak), respiratory rate (Rr), inspiration: expiration ratio (I: E), inspiratory time (It), and during a pause at the end of inspiration, and plateau airway pressure (Pplat), were also recorded.
Secondary variables were calculated as follows:
Compliance (C) = Vt / (Pplat - PEEP) (5), the dynamic and static Compliance measurements were taken, though the latter only if the patient was under neuromuscular relaxation for medical indi-cation. The dynamic compliance calculation was based on a <10% asynchronous index to ensure the reliability of the measurement.(5)
Elastance (E) = 1 / C, as the inverse of compliance.
Airway conduction pressure (APaw)
ΔPaw: Pplat - PEEP => Vt / C => E x Vt(5)
For the calculation of mechanical power (MP), the simplified formula proposed by Gattinoni at al.5 was used. Mechanical power (Joule / min) = 0.098 x (respiratory rate) x (tidal volume) x [peak pressure - (AP /2).5
The primary outcomes of the study were the number of days in the ICU, and the number of days under invasive mechanical ventilation. Patients were followed-up until death or ICU discharge. Potential selection biases were controlled with strict compliance with the inclusion and exclusion criteria; information biases were controlled with the requirement to clearly and fully complete the data collection instrument and rejecting any duplicate or incomplete records. Additionally, a subgroup analysis was conducted when the requirement for mechanical ventilatory support was due to the presence of SARS-CoV-2. Observer-related errors were controlled based on the homogeneity of the concepts used for the inclusion, exclusion, and definition of terms by the respiratory therapists and physiotherapists.
Statistical analysis
The data were analyzed using the R studio 1.2.5 software for Windows. Descriptive statistics were used to summarize the clinical characteristics of the study population according to the type of variable, for nominal variables, tables of frequency distribution, percentages, and ratios. For quantitative variables, in addition to the above, measures of central tendency (mean, median) and dispersion (variance, standard deviation, interquartile range) were used. The patients' characteristics with and without SARS-CoV-2 infection were compared using the Student's t-test for numerical variables and Pearson's chi-square for categorical variables at baseline. The correlation between ventilatory parameters and clinical outcomes (days of ICU stay and days of invasive mechanical ventilation) was reported using Spearman's Rho.
For primary outcomes, dependency relationships were established through the chi-square test to compare nominal or ordinal variables. The type of distribution was established to compare the quantitative variables; when the normal distribution assumptions were met, parametric tests were used (Student's t, anova); if these assumptions were not met, non-parametric tests were used (Mann-Whitney U, Kruskal Wallis). The number of days on mechanical ventilation were compared between the subgroups according to the value of the mechanical power discriminated in terciles, and survival analysis was performed using Cox regression. Death was considered the final outcome. Adjusted analyzes were controlled for sex, age, renal replacement therapy, inotropic support, neuromuscular relaxation, SARS-CoV-2 infection, and ventilatory parameters. Multivariate model 1 was adjusted for respiratory rate, tidal volume, and conduction pressure, while model 2 was adjusted for mechanical power. Hazard ratios were obtained and reported, and significance was determined based on a 95% confidence interval (95% CI).
RESULTS
The cohort included a total of 91 patients, who were admitted to 3 ICUs in the city of Pereira between June and October 2020. 72.5% (n = 66) of the patients were males and the average age was 59.6 ± 14.9 years. The average APACHE II score was 14.5 ± 7.9 and SOFA 8.6 ± 3.4. SARS-CoV-2 infection was diagnosed in 51.6% (n = 47) patients and 62.6% (n = 57) died. Twelve percent (n = 11) of the patients required renal replacement therapy, 41.8% (n = 38) received inotropic and / or vasopressor support and 64.8% (n = 59) were under neuromuscular relaxation.
Table 1 shows the characteristics of the patients included, as well as the comparison between patients with SARS-CoV-2 infection and patients without the infection. Regarding the clinical outcomes, no differences were found between the groups of patients.
Table 1 Characteristics of patients with mechanical ventilation.
| Total | SARS-CoV-2 infection | ||
|---|---|---|---|
| (n=91) | Negative (n=44) | Positive (n=47) | |
| Female | 25 (27.5) | 14 (31.8) | 11 (23.4) |
| Male | 66 (72.5) | 30 (68.2) | 36 (76.6) |
| Age | 59.6±14.9 | 61.3±17.0 | 58.1±12.5 |
| <45 years | 15 (16.5) | 9 (20.5) | 6 (12.8) |
| 45-64 | 38 (41.8) | 24 (54.5) | 14 (29.8) |
| >65 years | 38 (41.8) | 11 (25) | 27 (57.4) |
| Previous respiratory disease | 21 (23.1) | 12 (27.3) | 9 (19.1) |
| Severe ARDS | 34 (37.4) | 13 (29.5) | 21 (44.7) |
| APACHE II | 14.5±7.9 | 15.6±4.7 | 13.9±9.5 |
| SOFA | 8.6±3.4 | 9.0±4.0 | 8.2±2.7 |
| Renal replacement therapy | 11 (12.1) | 6 (13.6) | 5 (10.6) |
| Inotropic / vasopressor support | 38 (41.8) | 23 (52.3) | 15 (31.9) |
| Neuromuscular relaxation | 59 (64.8) | 13 (29.5) | 46 (97.9) |
| Outcomes | |||
| ICU days | 12.3±6.2 | 11.5±7.1 | 13.2±5.1 |
| IMV support days | 9.2±5.6 | 9.1±5.1 | 11.1±4.7 |
| Ventilation-free days | 2.3±3.1 | 2.2±3.5 | 2.0±2.7 |
| Death | 57 (62.6) | 26 (59.1) | 31 (66) |
Source: Authors.
Ventilatory parameters
Table 2 shows the ventilatory parameters at the beginning and 24 hours after the initiation of invasive mechanical ventilation. There was a reduction in FiO2 between the first and second measurement (from 56 ± 21 to 41 ± 15, p <0.001) and in the I:E ratio (from 2.7 ± 0.8 to 2.4 ± 0.7, p = 0.016, which was similar according to the SARS-CoV-2 infection status. Respiratory rate (p <0.001), I: E ratio (p = 0.025), FiO2 (p = 0.003), PEEP (p <0.001), peak pressure (p = 0.001), plateau pressure (p <0.001), pressure conduction and mechanical power (p <0.001) were higher in patients with SARS-CoV-2 infection, while dynamic compliance (p = 0.003) and static compliance (p = 0.001) were higher in patients without SARS-CoV-2 infection.
Table 2 Initial ventilatory parameters and 24 hours after IMV support in three hospitais in Pereira, Colombia.
| Ventilatory parameters | Total (n=91) | SARS-CoV-2 infection Negative (n=44) | SARS-CoV-2 infection Positive (n=47) | Valor p | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| To | T24 | p value | To | T24 | p value | To | T24 | pvalue | ||
| Breathing frequency | 21±5 | 20±6 | 0.100 | 18±4 | 17±6 | 0.811 | 23±5 | 24±4 | 0.049 | <0.001 |
| I:E ratio | 2.7±0.8 | 2.4±0.7 | 0.016 | 2.8±0.9 | 2.6±0.8 | 0.050 | 2.5±0.6 | 2.3±0.4 | 0.066 | 0.025 |
| Tidal volume | 434±50 | 431±50 | 0.857 | 433±54 | 427±54 | 0.312 | 435±46 | 435±45 | 0.299 | 0.82 |
| Volume (mL/Kg) | 6.95±0.84 | 6.91±0.87 | 0.954 | 7.04±0.97 | 6.95±1.01 | 0.362 | 6.87±0.68 | 6.87±0.73 | 0.329 | 0.328 |
| FiO2 | 56±21 | 41±15 | <0.001 | 50±19 | 38±13 | <0.001 | 63±22 | 43±17 | <0.001 | 0.003 |
| PaFi | 135±65 | 164±74 | 107±39 | <0.001 | ||||||
| PEEP (cm H2O) | 9±2 | 9±2 | 0.146 | 8±2 | 9±3 | 0.845 | 10±2 | 10±1 | 0.225 | <0.001 |
| Peak pressure | 31±8.7 | 30±8 | 0.091 | 27.8±9.6 | 28±10 | 0.282 | 34±6.6 | 32±6 | 0.900 | 0.001 |
| Plateau pressure | 21±6 | 20±4 | 0.034 | 18±5 | 19±4 | 0.226 | 23±5 | 22±4 | 0.510 | <0.001 |
| Driving pressure | 11±5 | 11±3 | 0.075 | 10±4 | 10±3 | 0.221 | 13±5 | 12±3 | 0.849 | 0.002 |
| Dynamic compliance | 23.7±11.1 | 23.34±9.21 | 0.479 | 27.3±13.1 | 25.9±10.8 | 0.732 | 20.2±7.4 | 20.9±6.7 | 0.381 | 0.003 |
| Static compliance | 44.6±20.0 | 43.8±15.8 | 0.157 | 52.1±24.5 | 48.4±19.0 | 0.684 | 37.6±10.9 | 39.6±10.5 | 0.273 | 0.001 |
| Power or mechanical power | 22.7±11.0 | 22.4±11.3 | 0.767 | 18.2±11.2 | 17.2±11.0 | 0.741 | 26.8±9.2 | 27.2±9.4 | 0.351 | <0.001 |
* p-value for the difference between patients with and without SARS-CoV-2 infection.
Source: Authors.
Mechanical power
The average mechanical power value was 22.7 ± 1 Joules/min. In the subgroup of patients with SARS-CoV-2 infection, the mechanical power was higher (26.8 ± 9 Joules/min) than in the subgroup of patients without a diagnosis of SARS-CoV-2 infection (18.2 ± 1 Joules/min) (p <0.001).
Clinical outcomes
The clinical outcomes of the patients is shown in Table 1. On average, the patients spent 12.3 ± 6.2 days in the ICU and 9.2 ± 5.6 days with invasive mechanical ventilatory support. ICU mortality was 62.6% (n = 57 patients). The occurrence of outcomes was similar between the groups with and without SARS-CoV-2 infection.
Table 3 shows the survival analysis using Cox regression for the risk of death, controlled by sex, age, static compliance, renal replacement therapy, inotropic support, neuromuscular relaxation, SARS-CoV-2 infection, and ventilatory parameters. A protective association was found between neuromuscular relaxation and time to death in model 1 (HR = 0.175, 95%CI 0.043-0.712) but not in model 2.
Table 3 Analysis using Cox regression for the risk of death in patients with ventilatory support with and without SARS-CoV-2 infection in three hospitals in Pereira, Colombia.
| Variables | Raw model | Adjusted Model 1* | Adjusted Model 2* | ||||||
|---|---|---|---|---|---|---|---|---|---|
| HR | CI95% | HR | CI95% | HR | CI95% | ||||
| Renal replacement therapy | 1.456 | 0.65 | 3.24 | 1.369 | 0.525 | 3.571 | 1.423 | 0.56 | 3.615 |
| Inotropic / vasopressor support | 0.88 | 0.51 | 1.51 | 0.556 | 0.243 | 1.271 | 0.764 | 0.398 | 1.468 |
| Neuromuscular relaxation | 0.77 | 0.44 | 1.34 | 0.175 | 0.043 | 0.712 | 0.358 | 0.121 | 1.057 |
| SARS-CoV-2 infection | 1.03 | 0.6 | 1.75 | 1.116 | 0.418 | 2.976 | 1.496 | 0.613 | 3.651 |
| Ventilatory parameters | |||||||||
| Breathing Frequency | |||||||||
| 12 to 17 | 1 | 1 | |||||||
| 18 to 21 | 0.906 | 0.462 | 1.775 | 3.033 | 0.791 | 11.629 | |||
| 26 to 35 | 1.306 | 0.697 | 2.445 | 4.178 | 0.983 | 17.761 | |||
| Tidal volume | |||||||||
| 330 to 399 | 1 | 1 | |||||||
| 400 to 459 | 0.94 | 0.52 | 1.7 | 1.015 | 0.501 | 2.058 | |||
| 460 to 562 | 0.603 | 0.28 | 1.301 | 0.381 | 0.132 | 1.100 | |||
| Driving pressure | |||||||||
| 3 to 9 | 1 | 1 | |||||||
| 10 to 11 | 1.453 | 0.742 | 2.845 | 2.219 | 0.782 | 6.301 | |||
| 12 to 26 | 1.39 | 0.753 | 2.566 | 3.119 | 0.737 | 13.200 | |||
| Mechanical power | |||||||||
| 4 to 16 | 1 | ||||||||
| 17 to 25 | 0.89 | 0.466 | 1.698 | 1.141 | 0.503 | 2.589 | |||
| 26 to 63 | 1.095 | 0.572 | 2.096 | 1.52 | 0.664 | 3.479 | |||
*Adjusted by sex, age, and static compliance.
Source: Authors.
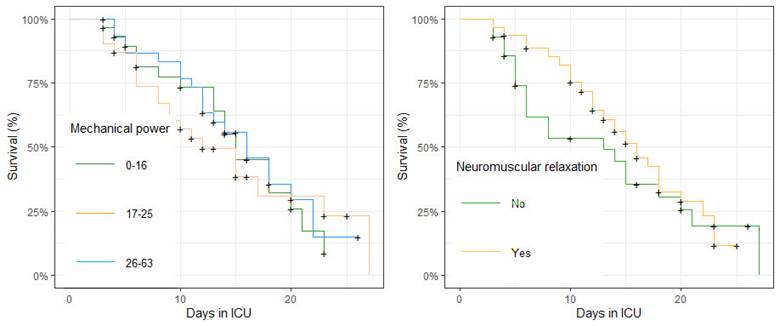
Figure 1 shows the average days in an ICU and days of invasive mechanical ventilation (IMV) according to the terciles of ventilatory parameters. Figure 2 shows the survival of patients with invasive mechanical ventilation. Panel A shows survival according to the terciles of mechanical power with no group differences identified. Panel B shows survival according to the use of neuromuscular relaxation, observing a higher percentage of survival and fewer days of ICU stay in the group of patients with neuromuscular relaxation.

Source: Authors.
Figure 1 Average days in an ICU and days of IMV according to the terciles of ventilatory parameters in patients with invasive mechanical ventilation in 3 ICUs in Pereira, Colombia.
DISCUSSION
VILI is the result of the relationship between the energy delivered by the ventilator to the lung parenchyma and how the lung responds. On one hand, there are the causes of ventilator generated VILI, including pressures, volume, flow, and respiratory rate. On the other hand, there are the conditions favoring lung injury; i.e. the amount of pulmonary edema, lung volume reduction, lung heterogeneity, cyclical collapse and loss of compliance, in addition to extrapulmonary factors such as perfusion, pH, and temperature during mechanical ventilatory support. All of these factors interact.10-11
Most studies on VILI focus on the static components of ventilation. However, another important factor is the respiratory rate which determines the number of times potential barotrauma or volutrauma is induced per minute.12,13 The inspiratory flow is another variable related to the development of VILI and the assumption could be made that the flow velocity plays a more significant role in a mechanically heterogeneous lung.14 The dynamic and static predictors are available, but traditionally lung-protective ventilation strategies have focused on measures and static characteristics of the tidal cycle such as tidal volume (Tv), plateau pressure (Pplat), PEEP, and recently driving pressure (AP); the importance of these measures is based on animal experiments and clinical data supporting their relevance.14-25
Gattinoni's group states that all the mechanical factors involved in ventilation, i.e: tidal volume, conduction pressure, flow, resistance, respiratory rate, and PEEP, are but different components of one single physical variable, which is the energy supply over time, that is, mechanical power.5 The mechanical power equation is derived from the equation of respiratory movement in which the pressure in the respiratory system has an elastic component necessary to distend the lung parenchyma, a resistive component necessary to advance the flow of air against the resistance of the airway and an inertial component due to changes in the lung parenchyma caused by volume acceleration.3,4 With the addition of PEEP at any given time, the pressure in the entire respiratory system equals:
P = ELrs • ΔV + Raw -F+ PEEP
(P: pressure in the respiratory system at any given time. ELrs: total elastance of the respiratory system. AV: tidal volume. Raw: resistance of the respiratory tract. F: flow. PEEP: positive pressure at the end of expiration.)
Therefore, VILI is the result of energy interchange, or mechanical power between the ventilator and the lung parenchyma, among other factors. In our study, the main reason for using mechanical ventilation in patients without a diagnosis of SARS-CoV-2 infection was hypoxemic respiratory failure secondary to acute respiratory tract infection; pressure conduction and mechanical power were higher in patients with SARS-CoV-2 infection, while both dynamic and static compliance were higher in patients without SARS-CoV-2 infection.
The mechanical power values found are consistent with those reported by cohort studies in international databases; a higher mechanical power value was documented in patients with SARS-CoV-2 infection and in the tercile analysis no significant differences were observed between groups, and no significant differences were found in the survival analysis using Cox regression for the risk of death. However, there is no conclusive scientific evidence to date that indicates which is the limit value of mechanical power in the population with SARS-CoV-2 infection under invasive mechanical ventilation, and even in the population with ARDS due to other causes; the mechanical power values have been heterogeneous in the different studies published so far.
The results of this study should be interpreted in the light of some potential limitations: population differences in terms of the reasons for administering mechanical ventilation; and, in the context of the COVID-19 pandemic, heterogeneity of the pulmonary and ventilatory characteristics of the patients. Therefore, we conducted some subgroup analyses as described. One of the limitations of the study are the differences in recording the ventilatory mechanics by different personnel in a multicenter study, although the respiratory therapist was monitored for the correct implementation of the protocol. Concerning the position of the patients, the prone ventilation variable was not considered in the initial design, and due to physiological factors inherent to the position, these factors may alter the results of ventilatory mechanics.
In our study, both an improved survival rate and shorter ICU stay were observed in the group of patients in which neuromuscular relaxants were used; however, a specifically designed study would be required to verify this association. Further prospective studies should be conducted to assess the value of mechanical power both at admission and over a 24 to 48 hour follow-up, in addition to an assessment after 8 days of pursuing a mechanical ventilation strategy.
This study paves the way to future research in the field of mechanical power in patients with ARDS due to SARS-CoV-2 infection and raises the need for permanent monitoring of this group of patients undergoing mechanical ventilation.
In conclusion, continuous monitoring of mechanical ventilation favors a safe therapeutic approach. 26 High mechanical power is a variable that has been described as a predictor of unfavorable outcomes in patients undergoing mechanical ventilation, considering the physiological substrate of the equation of motion. However, the specific value of mechanical limit power to ensure protective ventilation in all groups of patients managed with mechanical ventilation is not yet clear. Our results open the door to future research in the field of mechanical power as a variable to be evaluated in routine monitoring of mechanical ventilation.
ETHICAL DISCLOSURES
Ethical approval
The protocol of this study was approved by the Ethics Committee of Universidad Tecnológica de Pereira under number 04010620 dated June 4, 2020.
Protection of human and animal subjects
The authors declare that no experiments were performed on humans or animals for this study. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics commit-tee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
ACKNOWLEDGMENTS
Author Contributions
• ARP and JAE: Study concept and design, acquisition, analysis, and interpretation of data, drafting of the manuscript; critical revision of the manuscript for important intellectual content, original material and construction of images and tables. Administrative, technical, and material support; study supervision
• GS: Study concept and design; drafting of the manuscript, critical revision of the manuscript for important intellectual content, original material and construction of images and tables; study supervision.
• JFGG: Study concept and design, drafting of the manuscript, critical revision of the manuscript for important intellectual content, original material and construction of images and tables. Administrative, technical, and material study supervision.
• DAR: Critical revision of the manuscript for important intellectual content, study supervision. Interpretation of data, drafting of the manuscript. Administrative, technical, and material support.
• PM: Study concept and design, analysis, and interpretation of data, drafting of the manuscript, original material and construction of images and tables.
Administrative, technical, and material support. Statistical analysis.
• AVL: Acquisition, analysis, and interpretation of data, construction of tables, administrative, technical, and material support. Drafting of the manuscript.
• MAF and AGD: Revision of the manuscript. English translation. Administrative, technical, and material support.
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.











 text in
text in