INTRODUCTION
Hip surgery is currently one of the most frequent procedures; chronic pain associated with this intervention is reported in 7-28 % of patients. 1 Despite this reality, and the fact that it is classified as severe pain, there is no consensus available with regards to its therapeutic approach. This may be due to the complex sensory and nociceptive innervation of the hip, which hinders the prescription of an ideal analgesic plan. 2,3 Short et al. 4, showed that the femoral nerve has branches of the sensory cranial nerves to the inguinal ligament which are difficult to block with regional infra-inguinal techniques such as iliac fascia or femoral nerve block. Furthermore, these techniques fail to block the obturator and the accessory obturator nerve, which are key for the innervation of the anterior hip capsule.
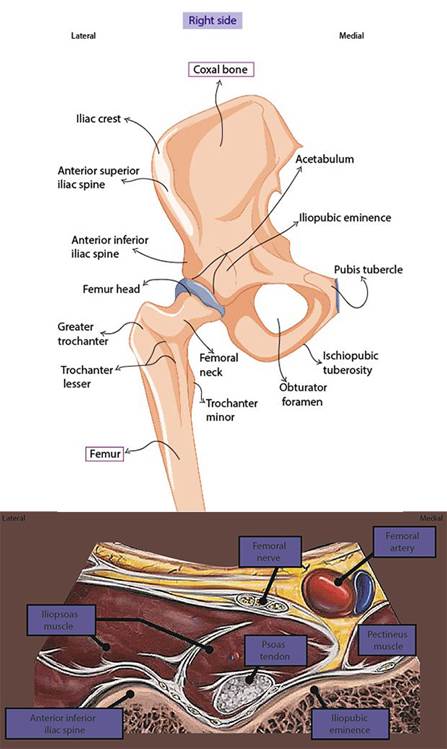
The PENG block was described by Girón Arango et al., in 2018, and enables the block of the joint branches that are not reached by other types of blocks. 5,6 It is considered a safer, opioid-sparing nerve block that favors early ambulation. 7-13 The advantages include the option to do it in supine decubitus avoiding weakness or motor block of the quadriceps muscle, which is essential for postoperative recovery and ambulation. 5 One drawback is that it cannot be used as a single analgesia strategy, but it must be combined with other peripheral nerve blocks 8 (Figures 1 y 2).
There is meager scientific evidence in terms of its efficacy and safety, and most of it has only recently been published. The objective of this narrative review is to analyze and ponder the current evidence with regards to efficacy and safety of the PENG block and its role in the postoperative pain management in hip surgery
To this end, a narrative review was conducted using the PubMed database and the Cochrane library. Two bibliography searches were performed. In the first, the key terms used included "total hip replacement" AND "PENG block". In the second, the key term used was "PENG block", with the following filters: review, systematic review, not older than one year. All papers discussing the PENG Block as an analgesia technique for hip surgery were included. Any studies conducted on anatomic cadaveric models, or involving specific anesthesia techniques (epidural, spinal, unilateral, caudal) were excluded.
All articles that could be accessed in full text, according to the relevance of the title and the summary, pursuant to the objective of the study, were analyzed. The first search generated 27 results, and 8 articles were selected for analysis. The second search generated 28 results, and 4 articles were analyzed. In total, 12 studies were included for review. Table 1 lists the most important characteristics of the studies analyzed and the selection process is depicted in Figure 3.
Table 1 Key characteristics of the studies analyzed.
| Study | Type of study | Primary variable | Principal results |
|---|---|---|---|
| Wang et al. (2022) 13 | Meta-analysis | Opioid use in the first 24 h. | Opioid use 4. in the PENG group vs. iliac fascia block 95 % CI (1.08 a -0.11) p < 0.05. |
| Huda et al. (2022) 14 | Systematic review and meta-analysis | Pain control and opioid use in the first 24 h. | No differences in the results of the pain scale. Time until the first rescue dose with opioids: 3.82 h difference (p=0,05). |
| Farag et al. (2022) 15 | Systematic review and meta-analysis | Pain scale results with PENG Block. | Better pain control with PENG block during the first hours. 95 % CI (-0.87 a -0.12); p = 0.01 |
| Morrison et al. (2020) 16 | Narrative review | Analyze the literature on PENG block as an analgesic and anesthetic technique. | Reduced need of systemic opioids. |
| Hua et al. (2021) 17 | Clinical controlled trial | VAS based pain at rest and during movement, before the block and at three different times after the block (t1, t2 and t3) vs. Iliac fascia block. | Statistically significant reduction in the pain scale at rest and during movement (t1-t4) in the PENG group vs. iliac fascia block (p < 0.05). |
| Lin et al. (2021) 18 | Clinical controlled trial | VAS pain scale difference during the preoperative period and 4 h PO. | The PENG group experienced less pain than the iliac fascia group (p=0.04). |
| Zheng et al. (2022) 19 | Non-inferiority clinical controlled trial | Pain scale result a12h PO. | No differences |
| Allard et al. (2021) 20 | Prospective | Accumulated dose of morphine 48 h PO. | No differences |
| Remily et al. (2022) 21 | Retrospective | Changes in VAS pain scale and use of opioids during the PO. | The changes in VAS at 48 h were significantly lower in the PENG group vs. Control (p < 0.001). Longer time until the first dose of systemic opioid in the PENG group vs. controls (8 h vs. 2.45 h p<0.002). Less doses of systemic opioids as compared to the control (p<0.022). |
| Mysore et al. (2020) 22 | Retrospective | Use of hydromorphone during the first 24 h PO. | The mean use of hydromorphone was lower in the PENG group vs. the control group (p=0.002). |
| Da Acosta et al. (2022) 23 | Case report | Analgesia delivered via continuous PENG block + femoral cutaneous block | VAS at 6 and 12 h postoperative was 0, and at 30 h = 2. No systemic opioids or motor block required. |
| Kukreja et al. (2020) + | Case series | VAS results with PENG block at 6.12 and 24 h. | Improved pain control in patients undergoing hip surgery for the first time. Most patients had VAS 0 at 24 hours. |
Source: Authors.

Source:Authors.
Figure 3 Flowchart depicting the selection process of the articles included in the review.
The results of this search are listed based on their level of evidence in terms of scientific quality, considering in the first place systematic and narrative reviews, then clinical controlled trials, observational and descriptive studies and case reports.
Available evidence
This paper includes three systematic reviews with meta-analyses. The first one by Wang et al. 13, in 2022, assessed the efficacy and safety of the PENG block for postoperative analgesia in hip surgery. The primary variable was the use of opioids during the first 24 hours after surgery. The intervention was PENG block vs. iliac fascia block. Five randomized CCTs were included with a total of 234 patients, 121 were randomized to the PENG group and 113 to the iliac fascia group. In most cases the local anesthetic used was ropivacaine (n=3), and levobupivacaine in the rest, at a concentration ranging from 0.2 to 0.5 %. The use of opioids at 24 h PO was lower in the PENG group vs. the iliac fascia block, with a 95 % Cl (-1.08 to -0.11) p< 0.05. Patient controlled analgesia was the most frequently used approach during the postoperative period.
The second systematic review by Huda et al. 14, in 2022, studied the efficacy of the PENG block in hip surgery vs. iliac fascia and its association with: 1) use of opioids, 2) motor block, and 3) patient satisfaction. The primary variable was pain control during the first 24 h and opioid use. Six RCTs were included (n=346), 2 of which were also included in the previous review. There were no statistically significant differences in the pain scales between the PENG block vs. iliac fascia at 6,12 and 24 h after surgery ([p=0.59, 95% CI: -0.38, 0.22], [p=0.10, 95% CI: -2.13, 0.17], [p=0.18, 95% CI: -2.98, 0.55]), respectively. With regards to time until the first rescue dose with opioids, a statistically significant difference was observed in the PENG group, with a mean difference of 3.82 h (p=0.05), and less use of opioids in the first 24 h post-surgery: mean decline 0.54 mg, which is statistically significant (p=0.05). The level of satisfaction among patients who received the PENG block and those who didn't (p=0.02) was also significantly different. Statistically significant differences were also observed in the incidence of motor block during the postoperative period (p=0.0002).
In the third systematic review and meta-analysis studied in this paper, Farag et al. 15, focused on the efficacy and safety of the PENG block in hip surgery. It was compared against other analgesia techniques in terms of pain reduction based on pain assessment scales, the need for additional analgesia and the incidence of complications. The primary variable in this study was the result of the pain scales (numerical and visual analogue scale), using the PENG block. The secondary variables were: time elapsed until the first rescue dose with opioids, length of hospital stay, patient satisfaction and complications such as nausea, vomiting, pruritus and dizziness. A total of 15 RCTs were included (n=837). The results of the pain scales favored the PENG group; however, this difference was only significant during the early postoperative period. The use of opioids was less in the PENG group during the first 24 h, but this effect was not evidenced at 28 h. No statistically significant differences were observed in the time elapsed until the first dose of opioids administered and the hospital length of stay. The incidence of vomiting was lower with the PENG block and no statistically significant differences were identified in terms of the incidence of nausea, pruritus and dizziness.
In a narrative review conducted in 2020 by Morrison et al. 16, the efficacy of the PENG block for analgesia or anesthesia in hip surgery was analyzed, including studies conducted in different countries: Canada, Turkey, India, Costa Rica, Italy and Spain. With regards to the efficacy variables, the use of PENG block, not associated with other blocks was described in 11 studies with a total of 35 adults and 1 pediatric patient undergoing hip fracture surgery. An adequate pain control was seen in these patients, with a reduced need of systemic opioids, and in some of the patients these analgesic agents were not even needed. In 9 trials (n=32), the PENG block was supplemented with other regional techniques, such as femoral nerve flock or lateral femoral cutaneous block. An adequate level of analgesia was observed in these patients, with minimal opioid requirements in the first 72 hours after surgery. In these studies the PENG block was administered in one single dose, except for one study in which a continuous infusion catheter was inserted for continuous infusion of the local anesthetic, in an adult patient undergoing hip arthroplasty. After 72 hours this patient did not require any additional analgesia. In terms of safety, two patients in which the technique was challenging, reported quadriceps muscle weakness but the motor block was resolved 48 h after surgery.
This article also included 3 clinical trials. The first by Hua et al. 17, was a randomized, single blind clinical trial conducted in China in 2021; the trial assessed the efficacy and safety of the PENG block vs. iliac fascia block. A total of 48 patients were included (27 males and 21 females), aged 65-85 years, undergoing arthroplasty due to hip fracture. Patients with coagulopathies, unable to consent, severe cardiovascular disease, neuromuscular disorders of the lower extremities, a history of epilepsy or alcoholism were excluded. The patients were randomized into two groups: iliac fascia block (n=24) and PENG block (n=24). The blocks were administered under ultrasound guidance prior to administering the spinal anesthesia and performing the surgery, using 20 mL of 0.4% ropivacaine. After surgery the patients received a sufentanil 1000 mg + tropisetron 10 mg infusion in 100 mL of saline solution and IV analgesia rescue doses with oxycodone 1 mg. The primary variable was the VAS pain score at rest and in movement prior to the block (t0), at 10 minutes (t1), at 20 minutes (t2) and at 30 minutes after the block (t3). The adverse effects were assessed, including quadriceps muscle weakness. There was a statistically significant reduction in the pain scale at rest and in movement (t1-t4) in the PENG block vs. the iliac fascia block (p<0.05). The VAS reduction 10 minutes after administering the block was more significant in the PENG vs. iliac fascia group, which is an indication of a faster onset of action of the PENG block. The level of patient satisfaction was higher in the PENG group. Motor block was identified in 7 patients in the iliac fascia group versus the PENG group (p< 0.05).
The second clinical trial by Lin et al. 18, was a randomized 1:1, double blind trial conducted in Australia during 2020, assessing the efficacy of the PENG block vs. iliac fascia block in hip surgery. Sixty patients ≥ 45 years old undergoing hip fracture surgery were randomized. The blocks were administered 15-45 minutes preoperatively with 20 mL of 0.75 % ropivacaine. The primary variable was the VAS pain score, in the preoperative period and 4 hours after surgery. The PENG group experienced less pain as compared to the iliac fascia group: 63 % no pain, 27 % mild pain and 10 % moderate pain vs. 30 % no pain, 27 % mild pain and 36 % moderate to severe pain in the iliac fascia group (p=0.04). The pain scale results on day 1 were similar in both groups, with no statistically significant differences. In terms of the quadriceps muscle strength, it was better preserved in the PENG group vs. the iliac fascia group, assessed in accordance with the Oxford classification; 60 % was intact in the PENG group vs. 0 in the iliac fascia group (p<0.001); and on day 1, 90 % was intact in the Peng group vs. 50 % in the iliac fascia group (p=0.004).
The third clinical trial by Zheng et al. 19, analyzed the non-inferiority of the PENG block vs. periarticular infiltration of local anesthetic (PAI). Sixty patients were randomized 1:1, single blind, aged between 40 and 80 years (group PENG n=30 and PAI n=30), with an ASA I-III score, programmed for hip arthroplasty. All patients received spinal anesthesia with hyperbaric bupivacaine 10-12 mg+100 µg of morphine. In the PAI group, the surgical team injected 20 mL of 0.75 % ropivacaine, ketorolac 60 mg, epinephrine 1 gr and 100 mL of saline solution, divided into two 50mL syringes. The PENG block was administered during the preoperative period under ultrasound guidance, with 30 mL of 0.5% ropivacaine. The primary variable was changes in VAS 12 hours after surgery, and the pre-specified non-inferiority value was 1. A difference in the pain scale was observed 12 hours postoperatively, between the PENG and PAI groups = 0.6 95% CI (-0.8 - 2), with non-significant differences between the two groups in the pain scale measured 24 h after surgery.
Observational studies
Five observational studies were included in this paper. The first was a prospective, cohort study conducted at a university hospital in France in 2019; Allard et al. 20 reviewed electronic medical records and compared the efficacy and safety of the PENG vs. femoral block in patients with hip fracture. The primary variable was the accumulated postoperative dose of morphine, 48 hours after surgery. The secondary variables were the results in VAS after 2, 12, 24 and 48 h of surgery, postoperative mobility of the lower limb operated, measured using the Medical Research Council (MRC) scale, incidence of adverse effects associated with the use of morphine, and length of hospital stay. Forty-two patients were included, femoral block n= 21 and PENG n=21. The patients were at least 18 years old, admitted for hip fracture arthroplasty, who received a regional analgesia technique (PENG or femoral block). The patients included had chronic pain and were previously receiving systemic opioids; patients with multiple trauma, cognitive decline or unable to consent, and patients who had received spinal or epidural anesthesia were excluded. The majority of the patients in the study were females (61.9 %), with a mean age of 80 years old. The median accumulated dose of morphine was 10 (0-20) mg. in the femoral block group, and 20 (0-50 mg) for the PENG group. There were no statistically significant differences between the groups in terms of pain intensity, time to ambulation, incidence of opioid-associated adverse events, or hospital length of stay. The quadriceps muscle weakness was lower in the PENG group, with a statistically significant difference (p=0.001).
Remily et al. 21, in a retrospective, case controlled study conducted in the United States, between 2017 and 2019, reviewed the medical records of patients undergoing total hip replacement with PENG block for postoperative pain control. A total of 96 patients were included, in which spinal anesthesia and iliac fascia block were administered, with no opioids used during the preoperative period. A total of 48 patients additionally received the PENG block after the procedure and were compared against the controls (n=48). During the postoperative period both groups received paracetamol, ketorolac and gabapentin. If needed, oxycodone or morphine was administered for the management of moderate to severe pain. The postoperative pain was assed using VAS every 12 hours for 48 h. The hospital stay was significantly shorter in the PENG group (39.7 vs. 51.3 h p<0.001), and the initial postoperative walk distance was also longer in this group (36.1 vs. 16.2 meters, p=0.001). The accumulated VAS scores at 48 hours were significantly lower in the PENG group vs. the control group (p<0.001). Likewise, the time elapsed until requesting the first dose of systemic opioid was significantly longer in patients receiving the PENG block vs. controls (8 h vs. 2.45 h p<0.002), and required a smaller dose of opioids (p<0.022).
Another retrospective study conducted in Canada by Mysore et al. 22, analyzed the PENG block plus intraarticular infiltration with local anesthetic for postoperative pain control in patients undergoing hip arthroplasty between 2018 and 2019. Patients who received intrathecal morphine, iliac fascia block and with opioid tolerance were excluded. A total of 47 patients were included in the PENG group and 76 in the control group. The mean consumption of morphine was lower in the PENG group vs. the controls (p=0.002).
Da Costa et al. 23, described a case report for analgesia delivered through a continuous infusion via a catheter inserted in the iliopsoas muscle and the iliopubic eminence, for total hip arthroplasty. The study showed that the continuous PENG block via a catheter with an elastomeric pump for 48 hours, plus the femoral cutaneous single dose block, provides an adequate level of analgesia. The VAS scores at 6 and 12 h after surgery were 0, and a VAS score of 2 at 30 h, which then dropped after 48 hours. Postoperative analgesia was complemented with coxib-type NSAIDs such as parecoxib and dipyrone. No opioids were required. The catheter remained in place for 48 h, and no quadriceps motor block was observed.
Kukreja et al. 24, in a series of cases of patients undergoing hip surgery at a tertiary care center in the United States, studied the results of the PENG block in 2020. The block was administered preoperatively for hip arthroplasty (n=6) and revision hip replacement surgery (n=6). The VAS was administered 6, 12 and 24 h after surgery. The total accumulated dose of morphine was measured at 6-12 h and 12-24 h postop. Patients undergoing hip arthroplasty for the first time showed lower pain scores and required less systemic opioids. Five patients undergoing primary hip arthroplasty had a VAS 0 score from 0 to 24 h after surgery. Patients undergoing revision hip replacement had an average VAS of 5.2 which dropped after 24 h.
DISCUSSION
The recently described PENG block provides an adequate level of analgesia for hip surgery. The use of this technique has been growing since 2018, with an exponential increase in research. This translates into increased use of this block, more research, and the need to systematize the information, standardize the technique, and identify its pain management role in this type of surgeries.
This narrative review included studies with different methodological approaches to assess the PENG block, from different countries. This is indicative of the fact that the technique is used worldwide and is reproducible.
Overall, favorable results were seen using the PENG block, with significant changes in different pain scales for hip surgery, whether used alone or in combination with other peripheral nerve blocks. It should be highlighted that there is no consensus in terms of the best efficacy comparator for this block. The comparators include iliac fascia, femoral nerve and obturator nerve. There is also variability with regards to the choice of the primary efficacy variable which was not standardized, since some studies used pain assessment scales (mostly VAS), while in other the variable measured was the use of opiates during the first postoperative hours. In terms of the technique per se, the dose and the type of local anesthetic agent are standardized. This hinders the actual evaluation of this analgesia technique.
Among the studies analyzed, hip surgery is not only emergency hip fractures - which should be differentiated from elective hip surgery 25, - but also elective procedures such as hip arthroplasty, with favorable outcomes for both clinical situations.
With regards to safety, no serious adverse effects were identified, in addition to the fact that there were less motor blocks when compared against other peripheral nerve blocks, which translates into improved patient satisfaction, early ambulation and less delays in hospital discharge.
This review ranks the PENG block as an effective and safe block in hip surgery with relevant evidence and methodological quality; it covers meta-analyses, systematic reviews, and case reports. It should be noted however, that this review failed to assess the risk with regards to bias of the publications included. Some of the limitations that need to be highlighted are: most of the studies were based on a small sample size; lack of standardized conditions with regards to the efficacy variable, use of the technique, dosing of the local anesthetic agent, and supplementation with other peripheral nerve blocks. Additionally, there was a discrepancy in the appropriate timing for administering the blocks: preoperative or postoperative.
It would be interesting to pursue further research standardizing the various aspects previously discussed, establishing protocols regarding the type of local anesthetic, the doses, the use of the technique, the timing of the intervention, the use of complementary approaches and techniques 26, and the management of postoperative pain in the framework of multimodal analgesia. All of these factors may contribute to standardize the technique and to conduct comparative studies with other peripheral nerve blocks with a view to generating quality scientific evidence.
CONCLUSIONS
In conclusion, the therapeutic approach of postoperative pain in hip surgery continuous to be challenging. Certainly the multimodal strategy is useful, effective and safe. The PENG block exhibits multiple advantages and seems to be an effective and safe technique with few documented adverse events. It is imperative to continue characterizing this block, alone or in combination with other regional blocks, to develop institutional analgesia protocols for orthopedic surgery, to adopt and standardize its use, and then to study the results under controlled conditions.
ACKNOWLEDGEMENTS
AD. Conceptualized the idea, searched the literature, collected the results, analyzed and interpreted those results and drafted the manuscript.
BS. Supervised the work and participated in the drafting and editing of the manuscript.
GI. Supervised the work and participated in the drafting and editing of the manuscript.
AD, BS, GI participated in the discussion, reviewed and approved the final version of the manuscript and accept the responsibility for the contents of the article.











 text in
text in