Introduction
Endoscopic retrograde cholangiopancreatography (ERCP) is a valuable procedure in managing biliopancreatic disease and is successfully performed in 85% to 95% of patients with normal gastrointestinal anatomy. In patients with gastrectomy and Roux-en-Y reconstruction, endoscopic instrumentation of the bile duct has lower success rates than ERCP in patients with preserved anatomy, increasing the need for more invasive and costly interventions1. ERCP in patients with anatomic abnormalities of the gastrointestinal tract, such as gastrectomy and Roux-en-Y reconstruction, is technically challenging for several reasons: the length of the biliopancreatic limb, the acute angle of the jejunojejunostomy, tortuosity due to adhesions, the difficulty in biliary cannulation, and the design (length) of the endoscopes2.
Double-balloon enteroscopy (DBE) allows for diagnosing and treating various small intestine diseases, including therapeutic interventions in the bile duct in patients with altered gastrointestinal anatomy3,4.
The first ERCP by DBE was reported in 2005, and since then, this procedure has been performed successfully in other countries5. The case we present below is the first of its kind published in Colombia in a patient with choledocholithiasis and altered anatomy due to a history of total gastrectomy with Roux-en-Y reconstruction due to gastric cancer.
Case report
We present the case of an 84-year-old female patient with a history of total radical gastrectomy and Roux-en-Y reconstruction for moderately differentiated gastric adenocarcinoma in 2012. She reported cramping pain in the right hypochondrium of nine hours of evolution, nausea, jaundice, and choluria. On physical examination, we found a jaundiced patient with normal vital signs, a tender abdomen in the right hypochondrium, and a negative Murphy’s sign. The paraclinical tests identified a cholestatic profile (Table 1), a hepatobiliary ultrasound with cholelithiasis and normal bile duct, an MRCP with multiple gallstones, signs of acute cholecystitis in the initial phase, and dilatation of the extrahepatic bile duct (11-mm common bile duct) with microcalculi in its distal portion (Figure 1). After discussing the case, the general surgery and gastroenterology services decided to perform a laparoscopic cholecystectomy with intraoperative enteroscopy to manage choledocholithiasis.
Table 1 Initial paraclinical test results
| Paraclinical test | Result | Reference value |
|---|---|---|
| Leukocytes | 3000 | |
| Neutrophils | 2400 | |
| Lymphocytes | 400 | |
| Hemoglobin | 11.7 g/dL | |
| Hematocrit | 37.5% | |
| Platelets | 128.000 | |
| Erythrocyte sedimentation rate | 42 mm/hour | |
| Creatinine | 1.15 mg/dL | |
| BUN | 28 mg/dL | |
| Aspartate aminotransferase | 282 U/L | 0-35 |
| Alanine aminotransferase | 129 U/L | 0-35 |
| Alkaline phosphatase | 159 U/L | 30-120 |
| Total bilirubin | 4.62 mg/dL | 0,3-1,0 |
| Direct bilirubin | 2.03 mg/dL |
Source: The authors.

Figure 1 MRCP showing multiple gallstones, extrahepatic bile duct dilation, and choledocholithiasis. Source: Authors’ archive.
Technique description
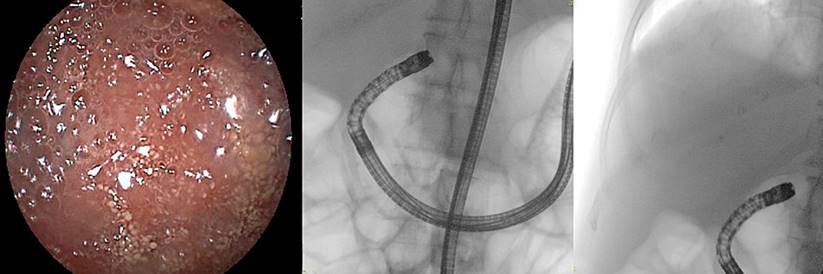
The patient was under general anesthesia, in the supine position. A short Fujifilm EI-580BT DBE was inserted orally (155 cm working length, 9.4 mm distal diameter, and 9.3 mm flexible portion diameter with a 3.2 mm working channel and overtube of 95 centimeters). We observed a normal esophageal-jejunal anastomosis and then advanced through the jejunum toward the jejuno-jejunal anastomosis (located 50 centimeters from the esophageal-jejunal anastomosis) (Figure 2).
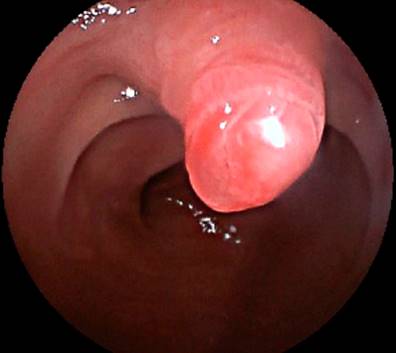
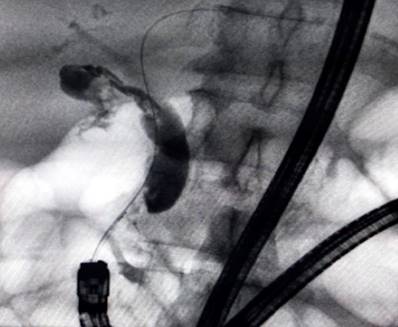
We entered through the biliopancreatic loop (with the help of fluoroscopy) up to the duodenal stump (approximately 150 centimeters in length) (Figure 3). A normal-looking duodenal papilla was identified (in the upper quadrant) (Figure 4). Cannulation was attempted with a conical tip catheter, an arc papillotome, and a needle papillotome, but we could not advance the guidewire toward the bile duct. So, an inverted papillotome was used, advancing the hydrophilic guidewire toward the bile duct (Figure 5).

Figure 5 Cannulation with an inverted papillotome and advancement of the guidewire into the bile duct. Source: Authors’ archive.
Cholangiography was conducted; we observed a normal intrahepatic bile duct and a dilated common bile duct measuring 12 millimeters in diameter, with a stone of 5 millimeters in its distal third and multiple gallstones (Figure 6). A papillotomy (Figure 7) and instrumentation of the bile duct with a 9-12 mm extractor balloon (Figure 8) were performed. We removed the calculus and biliary sludge (Figure 9) with no immediate complications.
During the extraction of the endoscope, we tattoed the mucosa of the biliopancreatic loop adjacent to the jejunojejunostomy for later identification in case of a new therapeutic procedure in the bile duct (Figure 10). The final x-ray showed the evacuation of most of the contrast medium from the bile duct (Figure 11). At this time, the surgery department performed the laparoscopic cholecystectomy.
The patient evolved satisfactorily, and the oral route was started the next day. Her liver biochemical profile was normal on the third postoperative day. She was discharged on the fifth postoperative day, ordering an outpatient follow-up in three weeks. Her liver biochemical profile was normal.
Discussion
In patients with altered gastrointestinal anatomy, ERCP has lower success rates than patients with normal anatomy; therefore, achieving access to the bile duct endoscopically is challenging in these cases. In patients with a history of gastrectomy with Roux-en-Y reconstruction and biliopancreatic diseases amenable to endoscopic management, ERCP by DBE is a viable option6.
Studies on this technique have reported that ERCP by DBE was successful in up to 87% of cases. It is deemed a safe intervention with low rates of significant complications, reporting adverse events in 0%-12%7.
The procedure is less invasive, with less morbidity than the percutaneous route or the surgical approach. Once the duodenal papilla or the biliary-enteric anastomosis is reached, it is possible to perform the rest of the endoscopic interventions usually performed by conventional ERCP, such as sphincterotomy, stone removal, stent insertion, or dilation of the stricture or duodenal ampulla5.
This laborious procedure requires a highly qualified team and takes longer than a conventional ERCP, with an average duration of 40 to 111 minutes4. In our case, the procedure was carried out successfully since biliary cannulation, papillotomy, and removal of the stone and biliary sludge from the common bile duct were achieved in a single intervention with no complications and excellent clinical evolution.
A short endoscope must be used for the ERCP accessories (cannula, papillotome, extraction balloons). Conventional DBEs have a length of 220 centimeters and are not suitable for ERCP accessories. Particularly difficult was the cannulation of the bile duct, which was only possible with an inverted papillotome because the DBE faces the papilla in a manner opposite to that of a conventional ERCP. Another difficulty is the absence of an elevator claw in the endoscope, which limits the mobility and direction of ERCP accessories.
For patients with cholecystocholedocholithiasis, there are several therapeutic options: pre-surgical ERCP8 and laparoscopic common bile duct exploration (LCBDE, either transcystic or by choledochotomy)9. Both techniques have similar efficacy in resolving choledocholithiasis without significant differences in morbidity and mortality10. ERCP resolves choledocholithiasis in 88% of cases11 and may result in major complications in 6%-15% such as acute pancreatitis (3%-10%), bleeding (0.3%-2%), cholangitis (0.5%-3%), and duodenal perforation (0.08%-0.6%)12. The LCBDE success rate is close to 90%, requires a surgeon expert in the technique, and can be associated with complications in 5%-15% of cases: retained stones (0%-5%), bile leak (2 3%-16.7%), pancreatitis (0%-3%), among others, such as basket impaction and bile duct narrowing9. Despite the efficacy and safety of LCBDE, one study found that only 7% of patients with choledocholithiasis were treated surgically, and 93% were managed with ERCP13. The cause of this discrepancy is multifactorial. The possible explanations are insufficient training in the technique, using instruments not routinely handled by the surgeon (dilating balloons, baskets, choledochoscope), and being a technique rarely performed9.











 text in
text in