Introduction
Acute pancreatitis is an inflammatory process with various etiologies; typically, it presents mildly, and recovery does not involve sequelae. However, mortality can reach 40% in severe cases1.
When parenchymal necrosis occurs and collections form, approximately 40% to 63% of patients require different interventions for drainage2.
In recent years, multiple endoscopic and surgical management approaches have been described. The decision to perform these procedures follows a step-up approach, beginning with less invasive methods such as percutaneous or transluminal drains, with surgical necrosectomy as the last option. This strategy aims to minimize surgical trauma, tissue damage, and inflammatory response1-3. Surgical management is associated with high complication rates, longer hospital stays, and higher mortality compared to minimally invasive endoscopic management1. Direct endoscopic pancreatic necrosectomy has been described as a minimally invasive procedure for managing walled-off necrosis located near the stomach and duodenum. For collections located laterally, a novel percutaneous procedure has shown good clinical outcomes1.
We present the case of a patient with severe necrotizing acute pancreatitis with extensive collections, in whom percutaneous and surgical drainage management failed, but who achieved a favorable clinical response with percutaneous endoscopic necrosectomy.
Case report
A 33-year-old male patient with a history of obesity was admitted to a secondary-level healthcare institution due to abdominal pain and recurrent vomiting. He was diagnosed with mild biliary-origin pancreatitis and started on medical management. Due to persistent pain, a contrast-enhanced abdominal CT scan was performed, revealing signs of pancreatic necrosis with a collection extending from the pancreas along the left paracolic gutter to the ipsilateral iliac fossa. Multiple percutaneous drainage procedures were performed by interventional radiology. The patient continued to experience abdominal pain, oral intolerance, and signs of systemic inflammatory response; after 20 days, he was transferred to a high-complexity institution.
A new abdominal CT scan (Figure 1) showed pancreatic necrotic collections dependent on the tail, with central and left-sided abdominopelvic distribution, and these collections were in contact with the gastric wall.

Author’s file.
Figure 1 Contrast-enhanced abdominal CT scan. Coronal section. Percutaneous drains are visible.
It was decided to perform laparoscopy for drainage of the collection and pancreatic necrosectomy. During surgery, an inflammatory phlegmon was observed in the upper abdomen with the omentum adhered to the liver and inflammatory thickening between the stomach and transverse colon, a retrogastric peripancreatic collection in the middle and distal thirds of the pancreas, and a frozen abdomen in the left flank. The procedure was suspended, a drain was placed in the cavity, and pancreatic tissue samples were taken. Cultures reported the growth of KPC-producing XDR Enterobacter cloacae, so targeted antibiotic therapy with ceftazidime/avibactam and metronidazole was administered concurrently for four weeks.
A follow-up abdominal CT scan revealed the persistence of collections extending into the abdominopelvic cavity with multiple septa and the presence of air inside, which had not decreased in size, with multipurpose catheters located within. Based on the imaging report, it was decided to manage the condition with percutaneous endoscopic necrosectomy.
Percutaneous endoscopic procedure
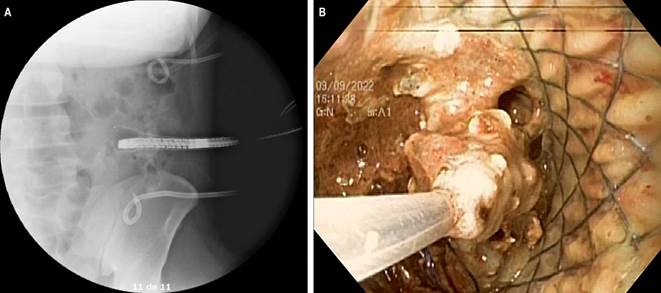
The procedure began with the medial pig-tail drain. Contrast medium was advanced, and under fluoroscopy, the drain was confirmed to be in the correct position. A Jagwire metal guidewire was then advanced through the drain, and the catheter was removed. The entry orifice was enlarged with a small 5 mm incision, and a 9 mm Savary bougie was advanced over the guidewire. A fully covered 16 cm esophageal stent was then advanced over the guidewire and deployed (Figure 2). A 12-15 mm dilation balloon was used to dilate the stent to 15 mm. An endoscope was then advanced through the stent, revealing a large cavity with necrosis and several drains inside. Using a loop, an endoscopic necrosectomy was performed to remove the abundant necrotic tissue, and the cavity was washed with saline solution. The stent was connected to a collection bag, and the drains were left in place for tidal irrigation (Figure 3).
Author’s file.
Figure 2 Percutaneous endoscopic necrosectomy. A. Placement of the esophageal stent under fluoroscopic guidance. B. Percutaneous endoscopic necrosectomy.

Author’s file.
Figure 3 Two pig-tail drains in the left flank, a Foley catheter in the anterior abdominal region, and a working port for percutaneous endoscopic necrosectomy are visible.
In the third necrosectomy session, a significant reduction in necrotic and purulent content was observed. Consequently, the pancreatic drainage device was removed and a Blake drain was inserted.
The patient showed appropriate clinical progression, with no fever spikes, controlled abdominal pain, and tolerance to oral intake. The patient was discharged with antibiotic management. During the follow-up appointment, it was decided to remove the drains.
Discussion
Pancreatic necrosis develops in approximately 20% to 30% of patients with acute pancreatitis, and in 20% to 40% of these cases, the necrosis becomes infected, significantly increasing mortality to up to 35%4. A multidisciplinary approach involving gastroenterologists, surgeons, interventional radiologists, and other specialists is recommended for comprehensive management.
Timely and effective drainage of infected necrotic tissue is essential for improving outcomes5. When there is clinical deterioration or a need for multiple interventions, a follow-up CT scan should be considered for further decision-making4. In the presented case, multiple ineffective interventions, undrained collections, and exposure to various antibiotic regimens led to the development of multidrug-resistant bacterial strains, underscoring the importance of effective drainage.
Historically, open surgery with abdominal cavity packing, scheduled laparotomies, and continuous lavage were the standard management approaches, but they carried high mortality rates2,5. Over the past two decades, advances in tools and non-invasive techniques have shifted the preference towards minimally invasive approaches for acute necrotizing pancreatitis. The step-up approach has demonstrated better clinical success rates, lower morbidity and mortality, shorter hospital stays, and reduced costs1,6. A hybrid approach combining different minimally invasive techniques is also worth considering7.
The choice of therapeutic modality depends on several factors, including the patient’s clinical status, local expertise and resources, anatomical position, content and extent of the collection, timing of presentation, and maturation of the collection wall. Thus, a single treatment protocol cannot be universally applied8,9, as each therapeutic modality suits a specific patient group.
In the present case, the transabdominal laparoscopic approach was unsuccessful due to significant inflammatory involvement. As described by De França and colleagues, an alternative is to use laparoscopy as a guide to identify and approach the collection, leaving a working port for the endoscope, and subsequently performing necrosectomy10.
In the case reported by Lee and colleagues, the patient experienced prolonged hospitalization following initial management with percutaneous drains, without complete resolution of the collections. This led to the decision to perform percutaneous endoscopic necrosectomy, establishing the percutaneous tract under fluoroscopic guidance11. In this instance, the fistulous tract was established using a covered esophageal stent.
Conclusions
A multidisciplinary approach with a step-up strategy, beginning with minimally invasive techniques, is preferred over conventional surgical interventions. Percutaneous endoscopic necrosectomy is a safe and effective procedure, offering lower morbidity and mortality, shorter hospital stays, and reduced costs. It should be considered a viable option in cases of extensive peripancreatic necrosis.











 text in
text in 



