Introduction
By 2021, in Colombia, 170 000 People were Living With HIV (PLWH), of whom 8600 were new cases, and 7600 (88 %) were men1. Current HIV incidence trends are difficult to estimate because the COVID-19 pandemic interfered with HIV testing and delivery of treatment and prevention interventions worldwide2. In Colombia, the HIV epidemic is concentrated in Men who have Sex with Men (MSM) and Transgender Women (TGW), with a high prevalence of 17 % and 21.4 %, respectively3,4. The increased annual age-adjusted HIV incidence in Colombia between 2008 (12.35 per 100 000 habitants) and 2016 (23,1 per 100 000 habitants)5 is concerning and justifies a renewed effort to cut down on new HIV infections.
In 2020, the World Health Organization (WHO) and the United Nations Program on HIV/AIDS UNAIDS proposed intensified HIV goals, namely 95 % HIV detection, 95 % treatment initiation, and 95 % treatment engagement plus the adoption of combined prevention interventions, including HIV Pre-Exposure Prophylaxis (PrEP), in the global strategy to eliminate HIV by 20306. PrEP involves the administration of antiretroviral medications to HIV-negative individuals to prevent the acquisition of HIV. PrEP can reduce the risk of HIV acquisition by more than 90 % while offering an excellent safety profile, as demonstrated in multiple clinical trials7,8. The combination of Tenofovir Disoproxil Fumarate and emtricitabine (TDF/FTC) has been used as a preferred backbone of HIV infection treatment for two decades. Additionally, TDF/FTC has demonstrated efficacy/effectiveness and safety in multiple clinical and demonstration PrEP trials and has become the mainstay of HIV PrEP worldwide8-10. HIV PrEP has also resulted in unprecedented reductions in HIV incidence in population studies around the world11,12. Consequently, many countries have adopted PrEP as part of a set of interventions to stop the HIV epidemic13. Furthermore, PrEP has demonstrated effectiveness at reducing new HIV infections in a variety of settings14, including some where high HIV detection and treatment had not previously resulted in a reduction of HIV incidence12. This evidence strongly suggests that HIV PrEP is necessary to meet the targets required for Ending the HIV Epidemic (EHE).
Despite the demonstrated effectiveness of PrEP, uptake has been slow. Latin America (LA), Peru, Mexico, and Colombia have conducted demonstration projects, but PrEP still needs to be utilized more needs to be widely utilized15. For instance, in Brazil16, at the forefront of PrEP implementation in LA, PrEP uptake across the country ranges from 0.6 % to 24 %. Notably, in Colombia, PrEP was provided for free to participants in a demonstration project, but its provision was halted at the end of the project (study participant verbal communication). In contrast, Brazil and Chile made tenofovir disoproxil fumarate and emtricitabine (TDF/FTC) available for PrEP under their public health system in 2017 and 2019, respectively16-18. TDF/FTC was approved for PrEP in Colombia by the regulatory agency INVIMA in early 2019. However, this approval was not widely advertised, and the medication was not initially publicly funded for PrEP. The Colombian government incorporated TDF/FTC in the publicly funded formulary at the end 202119. In the same year, the Colombian HIV national clinical guidelines endorsed PrEP20. Recently, in July 2023, national clinical and implementation guidelines were issued for PrEP, which included recommendations for TDF/FTC, Tenofovir Alafenamide/emtricitabine (TAF/FTC), dapivirine vaginal ring, oral maraviroc and parenteral cabotegravir for key populations21. At the current stage, evidence is required on the need and willingness of key populations to inform further PrEP implementation. Previous studies in Colombia have shown that social (HIV stigma, poverty), personal (lack of knowledge, lack of prescription skills), and health services barriers (funding for PrEP) may limit further adoption of PrEP22-24.
In the adoption process of PrEP, it is essential to estimate the size of the eligible population and their awareness of and willingness to use it. Likewise, the factors that determine these parameters must be well understood. Nevertheless, more evidence must be generated in the Colombian setting. Therefore, we decided to use the elements of the motivational PrEP cascade, as proposed by Parsons et al25, to track the progression of PrEP adoption in a sample of two key population groups, namely Men who have Sex with other Men and Trans Gender Women MSM and TGW. The study objectives were: 1) to estimate the proportion of individuals who are PrEP eligible, the proportion willing to take PrEP, the proportion of those who self-perceived as PrEP eligible, and the proportion who had any previous PrEP experience; and 2) to examine the social conditions related to each outcome of the motivational PrEP cascade.
Methods
Study design: This cross-sectional study conducted in Colombia aimed to collect data on PrEP-related adoption outcomes in MSM and TGW and their determinants. We recruited a non-probabilistic sample of MSM and TGW between April 2020 and February 2021.
Sampling and recruitment. Online recruitment, which was necessary during the early COVID-19 pandemic, was initiated in April 2020 and ended in December 2020. The study was advertised on social media such as Facebook, Twitter, and Grindr. For face-to-face recruitment, the assistance of leaders of MSM and TGW organizations who approached potential participants in person was required. A face-to-face survey was conducted between October 2020 and February 2021 in Medellin, Bogota, and Cali, the three major Colombian cities. There were six interviewers, all with experience working with the LGTBQ community. The interviewers visited the TGW social venues, where they obtained consent and conducted interviews. These venues included community organizations, sex work streets, parks, or neighborhoods often visited by transgender people TGW. In the case of MSM, the interviewers visited community organizations, social venues, and LGTBQ events or recruited participants from individuals referred by friends and LGTBQ networks.
Study population: In the online questionnaire, individuals who self-identified as MSM or TGW and self-reported an HIV-negative status in the screening questions were prompted to complete the survey. For the face-to-face survey, individuals were recruited if they self-identified as MSM or a TGW, reported to be HIV-negative, and older than 18 years old. Further in the analysis stage, participants who self-reported to be living with HIV and those who reported residing outside of Colombia were excluded.
Assessments and measures: the questionnaire developed was based on published questionnaires previously used for PrEP research26-27and validated exclusively in a sample of MSM in Colombia22. The questionnaire includes sociodemographic characteristics, PrEP perceptions, knowledge, self-efficacy, HIV related behaviors, among others. The survey had 167 questions and could be completed in approximately 30 minutes. For this report, we used sociodemographic data such as age, education, employment, living arrangements, socioeconomic status (defined as the socioeconomic strata of the neighborhood), and health insurance status. Before asking any question specific to PrEP, participants were provided with a statement on PrEP in Spanish: The English translation reads, "Pre-exposure prophylaxis (PrEP) is an HIV infection prevention strategy where HIV-negative individuals take anti-HIV medications before coming into contact with HIV to reduce their risk of becoming infected. These medications can prevent HIV from establishing an infection within the body. PrEP has been shown to reduce the risk of HIV infection through sexual contact in gay and bisexual men, transgender women, and heterosexual men and women, as well as in people who inject drugs. It does not protect against other sexually transmitted infections (STIs), nor does it prevent pregnancy. It is not a cure for HIV. Using tenofovir/emtricitabine-TDF/ FTC as PrEP provides a 96 % to 99 % reduction in the risk of infection in HIV-negative people who take the pills every day as directed. If you miss a daily dose, the level of protection against HIV may decrease. It only works if you take the medicine. People who use PrEP correctly and consistently have higher levels of protection against HIV."
Six PrEP outcomes were assessed using the Motivational PrEP cascade as a framework25. The PrEP cascade describes the stages of engagement with PrEP as an HIV prevention strategy. The stages of the PrEP cascade vary by studies but generally move from an awareness of PrEP for HIV prevention to deciding to use PrEP, accessing PrEP, and starting and being adherent to a PrEP regimen.
1) PrEP awareness refers to being aware of PrEP as a prevention tool. This differs from PrEP knowledge, which refers to knowing specific information about PrEP (i.e., efficacy, side effects, and others). Awareness was inquired with the question, "Have you ever heard of pre-exposure prophylaxis to prevent HIV or PrEP?" response options were dichotomic: "1=Yes" or "0=No".
2) PrEP eligibility, that is meeting objectively the criteria for PrEP prescription, was defined as meeting three criteria: 1) participants self-reported being HIV negative, had condomless anal sex in the last six months, AND 2) had either an HIV Incidence Risk Index (HIRI) >1028 or 3) a self-reported history of syphilis, gonorrhea, or chlamydia infection in the last six months. Items used to calculate HIRI scores are presented in Table 1.
3) PrEP willingness, that is, one's self-motivation to use PrEP, which was inquired with the question "If PrEP is effective in reducing the risk of HIV by 90 %, and if in the next 12 months, PrEP was offered for free in Colombia, would you like to use PrEP to prevent HIV?", measured on a 5-point Likert scale where 1 = "definitely yes," 2 = likely yes, 3 = neither yes nor not, 4 = likely not, 5 = "definitely not," those indicating "definitely yes" were coded as willing to take it.
Table 1 Items used to calculate HIRI scores28
| HIRI variable and response options | HIRI-Score |
|---|---|
| Age | |
| <18 years or ≥49 years | 0 |
| 18- 28 years | 8 |
| 29- 40 years | 5 |
| 41-48 years | 2 |
| Number of sex partners | |
| 0 to 5 | 0 |
| 6 to 9 | 4 |
| >10 | 7 |
| Number of episodes CRAI (condomless receptive anal intercourse-Number of episodes), with any partner | |
| 0 times | 0 |
| 1 or more times | 10 |
| Number of HIV-infected male partner | |
| None positive partner | 0 |
| 1 positive partner | 4 |
| >1 positive partner | 8 |
| Number of episodes of Condomless insertive anal sex, with HIV-infected partner | |
| 0 -4 times | 0 |
| 5 or more times | 6 |
| Methamphetamine use | |
| Yes | 5 |
| No | 0 |
| Popper use | |
| Yes | 3 |
| No | 0 |
Source: modified from reference 28
4) Perception of PrEP eligibility, one's perception of being eligible for PrEP, assessed with the question "Do you believe that you are a good candidate to take PrEP?" measured on a 5-point Likert scale where 1 = "I am a candidate" 2 = I am likely a candidate, 3 = neither yes nor not, 4 = likely not a candidate, and 5 = "I am not a candidate"; those indicating themselves as "definitely candidates" were coded as self-perceived as PrEP candidates.
5) Intention to take PrEP assesses the intention to use it if already available, and that was addressed with the question, "If your doctor or other health professional were available to prescribe PrEP for you in the next 12 months, would you start taking PrEP pills?" measured with a 5-point Likert scale where 1 = "I would definitely start taking them" 2 = "likely would start taking", 3 = neither yes nor not, 4 = likely would no start, and 5 = " I would no start taking them"; those indicating they "would begin taking PrEP" were coded as with intention to take PrEP, and
6) PrEP action, which is defined as having had a concrete action of searching or using PrEP, was assessed with two questions, "Have you asked a health professional about PrEP?" and "Have you taken an-tiretroviral (or HIV) medications to prevent HIV infection?", both response options were dichotomic "1 = Yes" or "0 = No"; experience was defined as a "yes" response to any of those items.
Statistical analyses: We used descriptive statistics to summarize the social characteristics of the sample as a whole and by sexual orientation/gender identity groups (MSM vs TGW). We then compared PrEP outcomes by sociodemographic characteristics using the chi2 test, Fisher's exact test in categorical variables, and the Kruskal-Wallis rank test in ordinal measures. The normal distribution of the variables was evaluated using the Shapiro-Wilk test. We follow two approaches to calculate the percentage of participants at each stage of the PrEP cascade. First, we calculate the percentage of participants who meet the criteria for each of the PrEP outcomes, independently of the distribution in the other outcome; we did this for the whole sample (and in each of the sexual orientation/gender identity groups). Then, we calculate the cascade using it as a starting point those eligible for PrEP, among those eligible, those who were aware, among those aware, those willing to start PrEP, and so on. To represent the motivational cascade in multivariate models, we considered that each of the PrEP outcomes represents a stage in the direction towards the decision of PrEP uptake: PrEP awareness precedes willingness, and the latter precedes intention, and so on. Thus, for each of the PrEP outcomes, the relationship with an outcome of the previous stage was examined. Analysis was conducted with the whole sample and in the sample of those eligible for PrEP. Poisson analysis for cross-sectional data has been used extensively even when the outcome is dichotomous, as in the case of our analysis29,30. All analyses were done with Stata/IC version 16. A significance level of less than 0.05 was used for all analyses.
Ethical aspects
This study is classified as "minimum risk research," according to the risk category established in Article 11 of Resolution 8430 of 1993 of the Colombian Ministry of Health. Ethical principles such as autonomy, beneficence, and justice were respected. This study was reviewed and approved by the Research Ethics Boards of Corporación de Lucha contra el SIDA (approval certificate no. 034 of May 16, 2018) and Queen's University (DMED-2326-20). Participants of the online sample were given access to an online consent form. Once consent was granted, a Qualtrics-based survey immediately followed, which could be completed online. Participants in the face-to-face survey were invited to participate in person, and written consent was obtained before starting the survey.
Conflicts of interest
The authors declared no potential conflicts of interest concerning this article's research, authorship, and/or publication of this article.
Results
A total of 301 online participants who resided in Colombia, most of whom were MSM and who self-reported as HIV negative, completed at least 80 % of the survey and composed the online sample. This corresponds to 51.5 % (301/584) of those who accessed the questionnaire. The face-to-face questionnaire was completed by 93 % of those invited to participate. Exclusions from the analysis were related to having reported living with HIV (n=84), being a Cis-woman (n=8), residing abroad (n=6), and answering less than 80 % of the questionnaire (n=53) (Figure 1).
The baseline demographic characteristics are shown in Table 2. A total of 552 participants were MSM (78 %), 301 (42 %) were recruited online, 251 (35 %) were recruited face-to-face, and 158 (22.2 %) were TGW, all of whom were recruited face-to-face. Participants had an average age of 30 years (range: 18-77 years); 31 % were less than 24 years old; had medium-high education levels, with 56 % having more than secondary education; 83 % reported being single, 56 % working, 21 % had incomes above two minimum monthly wages (minimum wage was approx. 255.66 USD per month), 87 % had health insurance, and 6 % resided in neighborhoods of high socioeconomic status. TGW were more likely to be of lower socioeconomic conditions compared to MSM, either because of education, income, or socioeconomic stratum (Table 2). Differences in socioeconomic conditions were also observed between the sample of MSM recruited online and face-to-face, with lower status observed in the face-to-face sample.
Table 2 Baseline demographic characteristics of the study participants.
| Groups | |||||
|---|---|---|---|---|---|
| All (n=710) | MSM interviewed face to face (n=251(35.3%)) | MSM completed online survey (n=301(42.4%)) | TGW** interviewed face to face (n=158(22.2%)) | p-value | |
| Age, years (means; standard deviation) | 30.3; 10.0 | 28.0; 9.9 | 31.2; 9.0 | 32.4; 11.3 | <0.001 |
| n (%) | n (%) | n (%) | |||
| Civil status | |||||
| Married - Free Union | 112 (15.7) | 38 (15.1) | 48 (15.9) | 26 (16.5) | 0.079 |
| Single | 589 (83.0) | 212 (84.5) | 245 (81.4) | 132(83.5) | |
| Separated-widowed | 9 (1.3) | 1 (0.4) | 8 (2.7) | 0 (0.0) | |
| Living arrangements | |||||
| Alone | 184(26.0) | 50 (20.0) | 64 (21.3) | 70 (44.3) | <0.001 |
| Family | 439(62.0) | 170 (68.0) | 202 (67.3) | 67 (42.4) | |
| Friends-others | 85(12.0) | 30 (12.0) | 34 (11.3) | 21 (13.3) | |
| Education level * | |||||
| Primary school | 44 (6.2) | 7 (2.8) | 1 (0.3) | 36 (22.8) | 0.0001 |
| Secondary school | 270 (38.0) | 132 (52.6) | 30 (9.9) | 108 (68.4) | |
| Technical-superior | 396 (55,8) | 112 (44,6) | 270 (89,7) | 14 (8,8) | |
| Socioeconomic stratum * | |||||
| One-two (very low-low) | 333 (46.0) | 131(52.4) | 85 (28.2) | 117 (74.0) | 0.0001 |
| Three-Fourth (Middle) | 330 (46.5) | 111 (44.4) | 178 (59.1) | 41 (26.0) | |
| Five-Six (High) | 46 (6.5) | 8 (3.2) | 38 (12.6) | 0(0.0) | |
| Occupation status (one or more options) | |||||
| Work * | 397 (55.9) | 129 (51.4) | 191 (63.5) | 77 (48.7) | 0.002 |
| Housekeepers* | 13 (1.8) | 1 (0.4) | 10 (3.3) | 2 (1.3) | 0.029 |
| Voluntary | 28 (3.9) | 9 (3.6) | 11 (3.6) | 8 (5.1) | 0.714 |
| Student* | 132 (18.6) | 64 (25.5) | 61 (20.3) | 7 (4.4) | <0.001 |
| Unemployed | 141 (19.8) | 49 (19.5) | 67 (22.3) | 25 (15.8) | 0.256 |
| Other* | 83 (11.7) | 21(8.4) | 18 (5.9) | 44 (27.8) | <0.001 |
| Current monthly income * | |||||
| No income | 132 (18.6) | 54 (21.5) | 49 (16.3) | 29 (18.4) | 0.0001 |
| <1 minimum salaries*** | 210 (29.6) | 90 (35.9) | 60 (19.9) | 60 (38.0) | |
| Between 1 to 2 | 219 (30.8) | 83 (33.1) | 73 (24.2) | 63 (39.9) | |
| >2 minimum salaries*** | 149 (21.0) | 24 (9.6) | 119 (39.5) | 6 (3.8) | |
| Health insurance/coverage (Yes) | 614 (86.6) | 223 (88.8) | 258 (86.0) | 113 (84.2) | 0.371 |
| PrEP awareness (yes) * | 361 (51.2) | 106 (42.2) | 213 (71.9) | 42(26.6) | <0.001 |
*Differences observed between the sample of MSM recruited online and face-to-face 0.001 < p-value < 0.014.
** Difference observed between the sample of TGW and MSM interviewed face to face (age, coexistence, education level, socioeconomic stratum, occupation status, and PrEP awareness; p s 0.001); difference observed between the sample of TGW and MSM online survey (age, coexistence, education level, socioeconomic stratum, income, occupation status, and PrEP awareness; p s 0.001).
***Current monthly income in dollars is approximately $ 256.
Source: own creation.
PrEP motivational cascade outcomes in the whole sample.
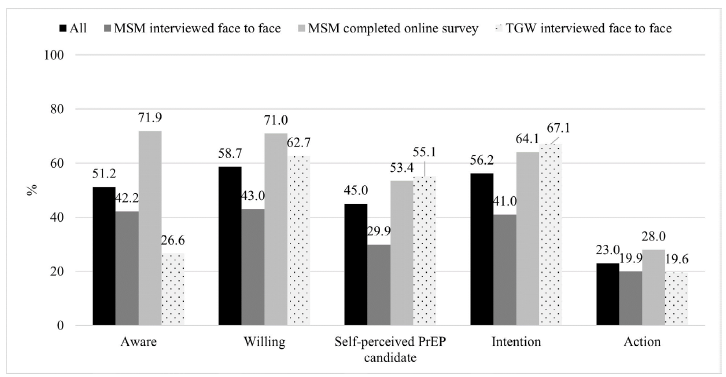
Fifty-one percent of the participants were aware of PrEP, 58.7 % were willing to use PrEP, 45 % were self-perceived as PrEP candidates, 56.2 % had the intention to take PrEP, and 23 % had acted around PrEP.
TGW reported the lowest level of awareness, while the MSM interviewed in person reported the lowest levels of willingness, perception of being PrEP eligible, and intention to use PrEP (Figure 2 and Table 3). There were differences in awareness (p < 0.001), willingness (p < 0.001), perception of being a PrEP candidate (p < 0.001), intention (p < 0.001), and action (p = 0.05) across the sex orientation/gender identity groups.
Source: own creation.
Figure 2 Distribution of PrEP outcomes in the whole sample. In evaluating PrEP motivational cascade outcomes categories, bars represent percentages of the total individuals sampled per study group for each outcome.
In bivariate analysis, PrEP eligibility was related to willingness, intention to take, and experience with PrEP (see Table 3). PrEP awareness was related to willingness and intention in that being aware of PrEP was related to a greater likelihood of both being willing and having the intention to take PrEP; in turn, willingness was associated with having an intention and experience with PrEP. Neither age nor having a stable relationship was related to any of the PrEP outcomes. The socioeconomic status of participants, irrespectively of the way it was measured (education, income, occupation, or neighborhood socioeconomic strata), was related to PrEP outcomes: those with lower socioeconomic status were more likely to be classified as eligible and were more likely to be aware, less willing to take, have less intention to take or have had an experience with PrEP (Table 3). Those without health insurance were likelier to be eligible and less likely to be aware of or have taken action around PrEP. Having health insurance coverage was not related to any other PrEP outcome. The multivariate analysis showed that the differences between sex orientation/gender identity groups and the negative effects of the low socioeconomic status variables on the PrEP outcomes remained (Table 4).
Table 3 Bivariate associations with PrEP outcomes using Generalized Linear Model-Poisson in all samples.
| Outcome (IRR*; IC95 %) | Eligibility, yes vs. no | Awareness, yes vs. no | Willing to take Prep, yes vs. no | Self-perceived as prep candidate, yes vs. no | Intention, yes vs. no | Action, yes vs. no |
|---|---|---|---|---|---|---|
| Group | ||||||
| MSM interviewed face to face | 1 | 1 | 1 | 1 | 1 | 1 |
| MSM completed online survey | 1.02 (0.87-1.19) | 1.70 (1.45-2.00) | 1.65 (1.40-1.94) | 1.79 (1.43-2,23) | 1.56 (1.31-1.86) | 1.41 (1.02-1.93) |
| TGW interviewed face to face | 1,06 (0,88-1,27) | 0.63 (0.47-0.85) | 1.46 (1.21-1.75) | 1.84 (1.45-2.33) | 1.63 (1.36-1.97) | 0.98 (0.66-1.47) |
| p-value | 0.8224 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | 0.0463 |
| Eligibility, yes vs. no | AA | 1.13 (0.98-1.31) | 1.18 (1.04-1.35) | 1.26 (1.06-1.50) | 1.18 (1.03-1.36) | 1.67 (1.23-2.26) |
| Awareness, yes vs. no | AA | AA | 1.37 (1.20-1.56) | 1.44 (1.22-1.71) | 1.26 (1.09-1.44) | 5.82 (3.84-8.83) |
| Willing, yes vs. no | ** | ** | ** | ** | ** | ** |
| Self-perceived as candidate, yes vs. no | ** | ** | ** | ** | ** | ** |
| Age, years(IRR ; IC95 %) | 0.98 (0.98-0.99) | 0.99 (0.99-1.00) | 0.99 (0.98-1.00) | 0.99 (0.98-1.00) | 0.99 (0.98-1.00) | 1.00 (0.99-1.02) |
| 18-30 | 1 | 1 | 1 | 1 | 1 | 1 |
| 31-45 | 0.79 (0.66-0.94) | 0.97 (0.82-1.14) | 0.87 (0.75-1.02) | 0.92 (0.76-1.13) | 0.87 (0.74-1.03) | 1.28 (0.95-1.72) |
| >45 | 0.65 (0.48-0.89) | 0.77 (0.57-1.03) | 0.90 (0.72-1.14) | 0.97 (0.73-1.30) | 0.92 (0.72-1.17) | 0.77 (0.43-1.35) |
| p-value | 0.0014 | 0.2189 | 0.2034 | 0.7493 | 0.2514 | 0.1253 |
| Civil status | ||||||
| Married - Free Union | 1 | 1 | 1 | 1 | 1 | 1 |
| Single | 0.88 (0.74-1.04) | 1.02 (0.83-1.24) | 0,90 (0,77-1.06) | 0.91 (0.73-1.13) | 0,98 (0.82-1.17) | 1.07 (0.72-1.58) |
| Separated-widowed | 0.74 (0.35-1.57) | 0.99 (0.48-2.03) | 1.12 (0.68-1.83) | 1.18 (0.60-2.30) | 1.25 (0.76-2.05) | 0.65 (0.10-4.15) |
| p-value | 0.2942 | 0.9824 | 0.3255 | 0.5392 | 0.5882 | 0.8304 |
| Education level | ||||||
| Primary school | 1 | 1 | 1 | 1 | 1 | 1 |
| Secondary school | 0.69 (0.56-0.86) | 0.95 (0.60-1.53) | 0.76 (0.58-1.00) | 0.75 (0.55-1.04) | 0.78 (0.61-1.01) | 0.68 (0.37-1.26) |
| High school | 0.74 (0.60-0.91) | 2.13 (1.37-3.30) | 1.09 (0.85-1.39) | 0.92 (0.68-1.25) | 0.94 (0.74-1.19) | 1.25 (0.71-2.21) |
| p-value | 0.0032 | < 0.0001 | <0.0001 | 0.0597 | 0.0344 | 0.0012 |
| Socioeconomic stratum | ||||||
| One-two (very low-low) | 1 | 1 | 1 | 1 | 1 | 1 |
| Three-Fourth (middle) | 0.97 (0.84-1.12) | 1.64 (1.39-1.93) | 1.07 (0.94-1.23) | 1.10 (0,92-1.31) | 0.99 (0,86-1,13) | 1.16 (0.85-1.56) |
| Five-Six (high) | 0.87 (0.63-1.19) | 2.20 (1.81-2.67) | 1.38 (1.14-1.67) | 1.32 (0.98-1.77) | 1.14 (0.89-1.46) | 2.67 (1.86-3.83) |
| p-value | 0.6721 | < 0.0001 | 0.004 | 0.1613 | 0.4919 | <0.0001 |
| Occupation status (one or more options) | ||||||
| Some kind of Any job vs. no work | 1.06 (0.93-1.22) | 0.78 (0.67-0.91) | 0.86 (0.76-0.98) | 0.82 (0.69-0.98) | 0.91 (0.79-1.04) | 0.91 (0.79-1.04) |
| Current monthly income | ||||||
| No income | 1 | 1 | 1 | 1 | 1 | 1 |
| <1 | 0.91 (0.76-1.10) | 1.05 (0.81-1.36) | 1.10 (0.89-135) | 0.99 (0.76-1.29) | 1.00(0.82-1.23) | 0.84 (0.53-1.33) |
| Between 1 to 2 | 0.85 (0.71-1.03) | 1.19 (0.93-1.53) | 1.13 (0.92-1.39) | 1.10 (0.85-1.42) | 1.03 (0.84-1.26) | 1.04 (0.68-1.61) |
| >2 | 0.84 (0.68-1.04) | 1.91 (1.52-2.39) | 1.31 (1.07-1.61) | 1.30 (1.01-1.69) | 1.15 (0.94-1.42) | 1.71 (1.13-2.57) |
| p-value | 0.3145 | < 0.0001 | 0.0355 | 0.0661 | 0.3902 | 0.0007 |
| Health insurance/coverage (Yes) | 1.19 (0.99-1.41) | 0.77 (0.60-1.00) | 0.98 (0.82-1.19) | 0.93 (0.71-1.20) | 1.01 (0.83-1.23) | 0.51 (0.28-0.89) |
*IRR: incidence rate ratio- calculated using GLM-Poisson Multivariate. **: not applicable.
Source: own creation.
Table 4 Multivariate associations with PrEP outcomes using Generalized Linear Model-Poisson in all samples.
| Outcome (IRR*; IC95 %) | Eligibility, yes vs. no | Awareness, yes vs. no | Willing to take Prep, yes vs. no | Self-perceived as prep candidate | Intention | Action |
|---|---|---|---|---|---|---|
| Group | ||||||
| MSM Survey face to face | 1 | 1 | 1 | 1 | ||
| MSM Survey Online | 1.35 (1.13-1.60)** | 1.38 (1.15-1.65)** | 1.50 (1.16-1.93)** | 1.37 (1.12-1.67)** | ||
| TGW | 0.78 (0.55-1.09) | 1.70 (1.37-2.10)** | 2.11 (1.61-2.75)** | 1.82 (1.48-2.24)** | ||
| Eligibility, yes vs. no | 1.18 (0.99-1.40)*** | 1.55 (1.17-2.04)** | ||||
| Awareness, yes vs. no | 0.22 (1.06-1.41)** | 1.37 (1.13-1.65)** | 1.20 (1.03-1.40)** | 5.67 (3.65-8.83)** | ||
| Age, years | ||||||
| 18-30 | 1 | 1 | 1 | 1 | 1 | |
| 31-45 | 0.77 (0.65-0.92)** | 0.88 (0.76-1.03) | 0.82 (0.71-0.96)** | 0.83 (0.70-0.98)** | 1.36 (1.03-1.80)** | |
| >45 | 0.63 (0.45-0.86)** | 0.78 (0.59-1.02)*** | 0.89 (0.69-1.13) | 0.89 (0.69-1.14) | 0.96 (0.62-1.48) | |
| Civil status | ||||||
| Married - Free Union | 1 | |||||
| Single | 0.86 (0.73-1.02)*** | |||||
| Separated-widowed | 0.89 (0.44-1.82) | |||||
| Education level | ||||||
| Primary school | 1 | |||||
| Secondary school | 0.65 (0.52-0.82)** | |||||
| High school | 0,73 (0,55-0,96)** | |||||
| Socioeconomic stratum | ||||||
| One-two (very low-low) | 1 | 1 | ||||
| Three-Fourth (Middle) | 1.26 (1.06-1.49)** | 0.87 (0.65-1.18) | ||||
| Five-Six (high) | 1.36 (1.09-1.68)** | 1.72 (1.12-2,62)** | ||||
| Current monthly income | ||||||
| No income | 1 | |||||
| <1 | 1.10 (0.85-1.43) | |||||
| Between 1 to 2 | 1.19 (0.89-1.58) | |||||
| >2 | 1.35 (0.99-1.84)*** |
*IRR: incidence rate ratio- calculated using GLM-Poisson Multivariate. ** p-value <0.05. *** 0.05 < p < 0.10.
Source: own creation.
PrEP motivational cascade outcomes in PrEP-eligible participants.
Table 5 presents the distribution of variables that determined eligibility for PrEP. Overall, 39.4 % of the MSM online, 49.4 % of the MSM face-to-face participants, and 51.5 % of TGW were eligible for PrEP. A total of 35.5 % of participants reported a high number of sexual partners, 43.3 % used poppers, 80.3 % reported condomless receptive anal intercourse, and 18.4 % reported a sexually transmitted infection in the previous six months. MSM and TGW eligibility criteria seem to differ in two aspects: having HIV-infected male partners and number of partners; nearly 90 % of the sample reported having no HIV-positive partners.
Table 5 Contribution of variables to individual scores of HIRI.
| HIRI variable and response options | HIRI-Score | All | MSM interviewed face to face | MSM completed online survey | TGW interviewed face to face |
|---|---|---|---|---|---|
| Age | n(%) | n(%) | n(%) | n(%) | |
| <18 years or ≥49 years | 0 | 53 (7.5) | 15 (5.9) | 18 (5.9) | 20 (12.7) |
| 18- 28 years | 8 | 56 (7.9) | 10 (3.9) | 30 (9.9) | 16 (10.1) |
| 29- 40 years | 5 | 221 (31.1) | 62 (24.7) | 111 (36.9) | 48 (30.4) |
| 41 -48 years | 2 | 380 (53.5) | 164 (65.3) | 142 (47.2) | 74 (46.8) |
| p-valueA | 0,0001 | ||||
| Number of sex partners | |||||
| 0-5 | 0 | 489 (68.9) | 195 (77.7) | 207(68.8) | 87 (55.1) |
| 6 to 9 | 4 | 89 (12.5) | 29 (11.5) | 43 (14.3) | 17 (10.8) |
| >10 | 7 | 132 (18.6) | 27 (10.8) | 51 (16.9) | 54 (34.1) |
| p-valueA | 0.0001 | ||||
| Number of episodes CRAI (condomless receptive anal intercourse-Number of episodes), with any partner | |||||
| 0 times | 0 | 404 (56.9) | 142 (56.6) | 175 (58.1) | 87 (55.1) |
| 1 or more times | 10 | 306 (43.1) | 109 (43.4) | 126 (41.9) | 71 (44.9) |
| p-valueA | 0.815 | ||||
| Number of HIV-infected male partner | |||||
| None positive partner | 0 | 657 (92.5) | 234 (93.2) | 269 (89.4) | 154 (97.5) |
| 1 positive partner | 4 | 44 (6.2) | 13 (5.2) | 27 (8.9) | 4 (2.5) |
| >1 positive partner | 8 | 9 (1.3) | 4 (1.6) | 5 (1.7) | 0 (0) |
| p-valueA | 0.021 | ||||
| Number of episodes of Condomless insertive anal sex, with HIV-infected partner | |||||
| 0 -4 times | 0 | 698 (98.3) | 244 (97.2) | 298 (99.0) | 156 (98.7) |
| 5 or more times | 6 | 12 (1.7) | 7 (2.8) | 3 (1.0) | 2 (1.3) |
| p-valueA | 0.289 | ||||
| Methamphetamine use | |||||
| Yes | 5 | 8 (1.1) | 5 (1.9) | 2 (0.7) | 1 (0.6) |
| No | 0 | 702 (98.9) | 246 (98.1) | 299 (99.3) | 157 (99.4) |
| p-valueA | 0.385 | ||||
| Popper use | |||||
| Yes | 3 | 230 (32.4) | 82 (32.7) | 86 (28.6) | 62 (39.2) |
| No | 0 | 480 (67.6) | 169 (67.3) | 215 (71.4) | 96 (60.8) |
| p-valueA | 0.068 | ||||
| Report condomless anal sex within the last 6 months | |||||
| Yes | na | 291 (41.0) | 150 (59.8) | 184 (61.1) | 85 (53.8) |
| No | na | 419 (59.0) | 101 (40.2) | 117 (39.9) | 73 (46.2) |
| p-valueA | 0.301 | ||||
| (Infectious syphilis or gonorrhea, chlamydia) STI, particularly if diagnosed in the preceding 6 months | |||||
| Yes | na | 70 (9.9) | 21 (8.4) | 33 (10.9) | 16 (10.1) |
| No | na | 640 (90.1) | 230 (91.6) | 268 (89.0) | 142 (89.9) |
| p-valueA | 0.61 | ||||
*p-value: comparing the three groups. *na: not applicable.
Source: own creation.
Assuming the PrEP-eligible participants were the starting point (100 %) of the motivational cascade, the outcomes were depicted in Figure 3. Most PrEPeligible individuals are lost in the awareness stage, which was more pronounced in TGW, in whom we observed that only 29.5 % were aware of PrEP from those eligible. The highest awareness among eligible people was observed in the MSM-online sample, 73 %, in which the experience with PrEP was the highest at 23 %.
Bivariate and multivariate results on the relations between sociodemographic conditions and PrEP outcomes are in the same direction as in the whole sample (tables 6 and 7): high levels of education, income, and socioeconomic status were related to greater awareness, willingness, intention, and action. In multivariate analysis, socioeconomic conditions remain important in terms of awareness and willingness. Having health insurance was not related to any outcome in the final models.
Table 6 Bivariate associations with prep outcomes using generalized linear model-Poisson in the sample eligible for PrEP.
| Outcome (IRR; IC95 %) | Awareness, yes vs. no | Willing to take Prep, yes vs. no | Self-perceived as prep candidate | Intention | Action |
|---|---|---|---|---|---|
| Group | |||||
| MSM interviewed face to face | 1 | 1 | 1 | 1 | 1 |
| MSM completed Online Survey | 1.56 (1.27-1.91) | 1.52 (1.25-1.85) | 1.70 (1.31-2.21) | 1.65 (1.32-2.05) | 1.40 (0.97-2.01) |
| TGW interviewed face to face | 0.63 (0.43-0.91) | 1.25 (0.98-1.58) | 1.40 (1.02-1.92) | 1.53 (1.19-1.95) | 0.77 (0.46-1.30) |
| p-value | <0.0001 | 0.0001 | 0.0003 | <0.0001 | 0.0239 |
| Eligibility, yes vs. no | ** | ** | ** | ** | ** |
| Awareness, yes vs. no | 1.37 (1.16-1.61) | 1.58 (1.26-1.97) | 1.29 (1.09-1.54) | 5.18 (3.11-8.61) | |
| Willing, yes vs. no | ** | ** | ** | ** | ** |
| Self-perceived as candidate, yes vs. no | ** | ** | ** | ** | ** |
| Age, years(IRR; IC 95 %) | 0.99 (0.99-1.01) | 0.99 (0.98-1.00) | 0.99 (0.98-1.01) | 0.99 (0.98-1.01) | 1.01 (0.99-1.02) |
| 18-30 | 1 | 1 | 1 | 1 | 1 |
| 31-45 | 0.97 (0.82-1.14) | 0.88 (0.72-1.08) | 0.96 (0.75-1.23) | 0.94 (0.76-1.15) | 1.41 (0.99-1.98) |
| >45 | 0.77 (0.57-1.03) | 0.91 (0.66-1.26) | 0.88 (0.57-0.137) | 0.97 (0.70-1.34) | 0.71 (0.31-1.60) |
| p-value | 0.1773 | 0.4331 | 0.8256 | 0.8152 | 0.0785 |
| Civil status | |||||
| Married - Free Union | 1 | 1 | 1 | 1 | 1 |
| Single | 0.97 (0.77-1.24) | 0.95 (0.78-1.15) | 0.97 (0.74-1.26) | 0.98 (0.79-1.21) | 1.05 (0.68-1.62) |
| Separated-widowed | 0.90 (0.33-2.47) | 1,14 (0.63-2.06) | 0.98 (0.36-2.70) | 1.23 (0.67-2.23) | 0.93 (0.16-5.33) |
| p-value | 0.9675 | 0.7116 | 0.9731 | 0.7354 | 0.9699 |
| Education level | |||||
| Primary school | 1 | 1 | 1 | 1 | 1 |
| Secondary school | 1,28 (0,70 - 2,33) | 0.78 (0.57-1.08) | 0.96 (0.62-1.50) | 0.83 (0.61-1.14) | 0,91 (0.40-2.05) |
| High school | 2.47 (1.41- 4.33) | 1.15 (0.87-1,52) | 1,26 (0,83-1,89 | 1,04 (0,78-1,39) | 1,93 (0,92-4,06) |
| p-value | <0.0001 | 0.0004 | 0.0641 | 0.0596 | 0.0007 |
| Socioeconomic stratum | |||||
| One-two (very low-low) | 1 | 1 | 1 | 1 | 1 |
| Three-Fourth (Middle) | 1.54 (1.25-1.89) | 1.06 (0.90-1.25) | 1.12 (0.90-1.39) | 0.91 (0.76-1.08) | 1.17 (0.82-1.67) |
| Five-Six (high) | 2.22 (1.78-2.76) | 1.45 (1.18-1.78) | 1.60 (1.18-2.17) | 1.32 (1.05-1.66) | 2.90 (1.97-4.27) |
| p-value | <0.0001 | 0.0013 | 0.0089 | 0.0071 | <0.0001 |
| Occupation status (one or more options) | |||||
| Some kind of job vs. no work | 0.77 (0.64-0.94) | 0.86 (0.73-1.00) | 0.77 (0.62-0.95) | 0.94 (0.80-1.11) | 0.71 (0.51-1.00) |
| p-value | 0.01 | 0.059 | 0.017 | 0.467 | 0.05 |
| Current monthly income | |||||
| No income | 1 | 1 | 1 | 1 | 1 |
| <1 | 1.14 (0.82-1.59) | 1.39 (1.06-1.82) | 1.21 (0.86-1.69) | 1.12(0.87-1.45) | 0.73 (0.42-1.25) |
| Between 1 to 2 | 1.34 (0.98-1.84) | 1.41 (1.08-1.85) | 1.30 (0.93-1.80) | 1.18 (0.91-1.51) | 1.02 (0.62-1.67) |
| >2 | 1.97 (1.48-2.64) | 1.54 (1.17-2.02) | 1.56 (1.12-2.17) | 1.23 (0.94-1.60) | 1.89 (1.21-2.96) |
| p-value | <0.0001 | 0.023 | 0.0441 | 0.4676 | 0.0001 |
| Health insurance/coverage (Yes) | 0.79 (0.58-1.07) | 0.99 (0.79-1.23) | 1.01 (0.77-1.34) | 1.00 (0.80-1.26) | 0.51 (0.27-0.96) |
| p-value | 0.129 | 0.902 | 0.913 | 0.975 | 0.036 |
*IRR: incidence rate ratio- calculated using GLM-Poisson Multivariate; **: not applicable.
Source: own creation.
Table 7 Multivariate association with PrEP outcomes using generalized linear model-Poisson in the eligible sample to PrEP.
| Outcome (IRR*; IC 95 %) | Awareness, yes vs. no | Willing to take Prep, yes vs. no | Self-perceived as prep candidate | Intention | Action |
|---|---|---|---|---|---|
| Group | |||||
| MSM Survey face to face | 1 | 1 | 1 | 1 | |
| MSM Survey Online | 1.30 (1.05-1.62)** | 1.33 (1.08-1.63)** | 1.48 (1.10-1.97)** | 1.51 (1.19-1.92)** | |
| TGW | 0.82 (0.54-1.26) | 1.38 (1.04-1.82)** | 1.56 (1.10-2.22)** | 1.68 (1.27-2.23)** | |
| Awareness, yes vs. no | 1.23 (1.02-1.47)** | 1.46 (1.14-1.86)** | 1.23 (1.02-1.48)** | 4.76 (2.80-8.07)** | |
| Age, years | |||||
| 18-30 | 1 | ||||
| 31-45 | 0.89 (0.73-1.09) | ||||
| > 45 | 0.57 (0.35-0.91)** | ||||
| Education level | |||||
| Primary school | 1 | 1 | |||
| Secondary school | 0.94 (0.48-1.86) | 1.19 (0.85-1.66) | |||
| High school | 1.33 (0.99-1.78)*** | 1.31 (1.02-1.69)** | |||
| Socioeconomic stratum | |||||
| One-two (very low-low) | 1 | ||||
| Three-Fourth (Middle) | 1.26 (1.03-1.56)** | ||||
| Five-Six (Hight) | 1.52 (1.18-1.96)** | ||||
| Current monthly income | |||||
| No income | 1 | ||||
| <1 | 1.36 (1.06-1.76)** | ||||
| Between 1 to 2 | 1.33 (1.02-1.74)** | ||||
| >2 | 1.21 (0.92-1.60) |
*IRR: incidence rate ratios- calculated using GLM-Poisson Multivariate; **p-value<0.05; *** 0.05 < p < 0.10
Source: own creation.
Discussion
This study is the first in Colombia to use the motivational PrEP cascade proposed by Parsons et al25, including PrEP eligibility, awareness, willingness, and intention in persons who self-identified as MSM or TGW. We found a high proportion, nearly 50 % of participants in this sample, of PrEP-eligible individuals, suggesting a high need to implement this intervention in Colombia, similar to what has been found in many other countries with similar HIV epidemics31,32. Other studies in Latin American populations reported identical figures in terms of PrEP eligibility in MSM and TGW: around 66 % of TGW in Brazil33, and between 51 % - 54 % of MSM at high risk of HIV acquisition in Brazil, Mexico, and Peru32. Other studies involving Latino populations also show that high proportions of TGW and MSM participants are PrEP eligible (eligibility adapted from the WHO criteria for pre-exposure prophylaxis or criteria from the CDC/Brazilian recommendations)26,33,34. Although the estimated HIV acquisition risk in MSM and TGW in our study is high, this may still be an underestimation given the lack of awareness from participants of their sexual partners' HIV serostatus and underreporting of asymptomatic STIs (e.g., latent stages of syphilis, health system limitations on extra-genital Chlamydia and Gonorrhea testing), which would have potentially increased eligibility if known. In addition, recall bias (e.g., not remembering how many partners they had sex with during the last six months) or the Hawthorne effect in participants interviewed face-to-face (e.g., minimizing the report on the number of sex partners while being observed) may also favor under-reporting risk.
Our results support the pertinence of the cascade concept to describe the status of PrEP uptake in MSM and TGW. In this regard, we found that PrEP awareness predicted willingness. In turn, willingness increased the likelihood of intention to take PrEP.
Participants with previous experience with PrEP reported more awareness of and willingness to take PrEP. This has been described in previous studies in Latin America26,35. The concept of a cascade to describe people at different stages of intervention uptake has been widely used for HIV treatment and to delineate population policy goals for HIV36,37. Similarly, the cascade provides a snapshot of how PrEP is perceived by a population sample expected to be a target for such an intervention. In this sample, 293 MSM and 88 TGW were eligible for PrEP, but most participants who completed the survey face-to-face needed to be made aware of its existence. Interestingly, more people were willing to take PrEP than those aware of the intervention. This is likely so because PrEP awareness was low in Colombia at the time of this survey (in the absence of a formal PrEP campaign), and the question about willingness in this survey was posed after an introductory paragraph that highlighted the expected PrEP benefit assuming no cost to the user. These observations suggest that, in Colombia, PrEP campaigns need to emphasize PrEP awareness with key messages such as the expected benefit, ease of use, and safety and make efforts towards eliminating or reducing costs to users.
While PrEP has demonstrated efficacy in a wide variety of populations with a high risk of HIV acquisition, including MSM, TGW, heterosexual individuals, and people who inject drugs8-10,38, MSM and TGW are expected to be a significant proportion of PrEP users in Colombia since these are two populations with the highest HIV prevalence in this country39. PrEP awareness in this study was 51.2 % overall, with a higher proportion of MSM being PrEP aware (completed online survey 71.9 % and interviewed face to face 42.2 %) than TGW (26.6 %). This level of awareness is comparable to that of other LA countries (Supplementary Table 1): An extensive multi-country Latin American survey in MSM found 10.4 % of PrEP awareness in 201240. This level increased over time in Brazil, with 51.5 % in 201741 and 64.9 % in 201826. PrEP awareness in MSM was 46.6 % in Peru and 64 % in Mexico in 201826. These figures are much lower than those reported in US samples in 2017 (95 %) and Canada in 2016 (80 %)42,43. Factors linked to the formal adoption of PrEP by the health systems in North America likely explain the much higher awareness of target populations in those settings. PrEP awareness in TGW in our sample was much lower than that of MSM. Lower PrEP awareness has been described consistently in TGW in Latin America and the United States33,44,45. TGW are consistently more socially vulnerable and marginalized across countries, with Colombia being no exception39,46. Despite this, TGW expressed a higher willingness to take PrEP, a finding that has also been demonstrated elsewhere33,47,48. These two observations suggest that this population group would significantly benefits from PrEP implementation. The qualitative results from PrEP-COL49 indicate that TGW perceived PrEP "as a need" and "as useful" along with condoms in cases of power imbalance in the context of sex work or with casual sex with men who do not want to use a condom50. Notably, online advertisement was ineffective at reaching TGW in our study, while strategies led by LGTBQ community leaders proved more suitable. This highlights that the socialization of PrEP campaigns requires adjustments suitable for the various population groups of interest.
Other social disparities in PrEP eligibility, awareness, and uptake have also been described. People with higher levels of stigma use less PrEP.
Racial disparities have been described in the US, where African Americans and Hispanics are less likely to use PrEP51. In Australia52, the UK53, and France54, MSM with social disadvantages were less likely to have the knowledge and to take PrEP. Similar results were found in MSM in Canada55. Our study has also demonstrated that PrEP eligibility, awareness, and willingness to use PrEP are highly inequitable in Colombia as the more educated, those with higher income, or those living in a higher SES neighborhood were more likely to have PrEP-positive cascade outcomes. Efforts to increase access to low SES MSM and TGW to PrEP information are a sensitive need in Colombia. Using social media to disseminate information about PrEP seems to reach individuals with higher SES but will likely miss reaching a large proportion of MSM and TGW.
This study is not free of limitations. This study collected information in two non-probabilistic sampling strategies. The study had to adapt to the COVID-19 epidemic, so it started with online surveys, which others have successfully used. However, the study population recruited online was mainly composed of MSM and no TGW, which required targeted advertisement via community organizations and face-to-face interviews during COVID-19 low-incidence periods. This study's sample of MSM and TGW seems similar to a sample previously recruited in three large cities in Colombia using respondent-driven sampling (Supplementary Table 2)3,4. To confirm the veracity of the information in the online survey, we asked various questions that allowed us to assess consistency, such as gender, sex, sex with women, sex with men, etc. We have used 6 to 12-month recall periods, which allows for the introduction of recall bias, but landmark studies have employed similar recall periods, which makes them comparable20.
Supplementary Table 1 Comparative studies of awareness, willingness, and intention to take PrEP in Latin American countries.
| Author | Country | Sample | Eligibility | Awareness | Willingness | Intention | Year of Data collection |
|---|---|---|---|---|---|---|---|
| MSM | |||||||
| Torres TS, Konda KA, Vega-Ramirez EH, Elorreaga O A, Diaz- Sosa D, Hoagland B, et al (2019)18. | Brazil, Mexico and Peru. | Participants accessing the questionnaire: N=43.687. | 67.50 % | 64.92 % | 64.23 % | No data: Willingness is understood as an intentional behavior based on 2 principles: recognition of the behavioral objective (ie, taking PrEP) and strategies implemented to achieve this objective. | 2018. |
| Individuals who completed the questionnaire and were included in the analysis: N=19,457 (44.54 %) | |||||||
| Hoagland B, De Boni RB, Moreira RI, Madruga JV, Kallas EG, Goulart SP, et al (2017)37. | Brazil. | The final study sample consisted of 1187 individuals, 95,3 % were male and 4,7 % were trans women. | Not reported. | 61.30 % | 82.10 % | No data: they have measured intention to use PrEP as a proxy of willingness. | 2014-2015. |
| Yi S, Tuot S, Mwai GW, Ngin C, Chhim K, Pal K, et al (2017)25. | Systematic review: studies related to Latin America | ||||||
| 145 countries in Africa, Asia, Europe and Latin America. | 2774 MSM. | Not reported. | 69.80 % | 80.80 % | Not reported. | 2012. | |
| Peru, India and South Africa. | 383 MSM. | Not reported. | Not reported. | 69 % | Not reported. | 2010-2011. | |
| Brazil. | 1131 MSM. | Not reported. | 61.3 % | 82.1 % | Not reported. | 2014-2015. | |
| Perú. | 532 MSM and TG. | Not reported. | Not reported. | 96.2 % | Not reported. | 2008. | |
| Edeza A, Galárraga O, Santamaria EK, Sosa-Rubí S, Operario D, Biello KB (2020). | Mexico. | A total of 23 participants completed in-depth semi-structured interviews. | Not reported. | Almost all participants stated that they were unfamiliar with PrEP prior to the interview. | Among the participants, most expressed interest in the medication after receiving information about it during the interview. | Not reported. | |
| Edeza A, Galarraga O, Novak D, Mayer K, Rosenberger J, Mimiaga M, et al (2019)28. | Latin America. | We carried out a multinational online survey of MSM in Latin America (n = 22698) in 2012. | Not reported. | 10.40% | Not reported. | Not reported. | 2012. |
| Torres TS, Luz PM, De Boni RB, de Vasconcellos MT, Hoagland B, Garner A, et al (2019)29. | Brazil. | Of 7242 individuals, 4 136 (57 %) completed the questionnaire. | Not reported. | 51.5 % | 56.3 % | Finally, they have measured intention to use PrEP, PEP, condoms, and HIVST as a proxy of willingness. | 2017. |
| TGW | |||||||
| Jalil EM, Grinsztejn B, Velasque L, Makkeda AR, Luz PM, Moreira RI, et al (2018)23. | Brazil. | A total of 374 individuals returned with a recruitment coupon, 370 consented with their participation and were screened (98,9 %) and 345 (93,2 %) eligible transwomen participated in the study. | 66.8 % | 38 % | 74.4 % | Not reported. | 2015-2016. |
| Poteat T, Wirtz A, Malik M, Cooney E, Cannon C, Hardy WD, et al (2019)44. | EEUU (Baltimore and Washington, DC). | Participant TGW, N=201. | Not reported. | 86.6 % | 75 % | No reported. | 2015-2017. |
| Zalazar V, Arístegui I, Kerr T, Marshall BD., Romero M, Sued O, et al (2016)45. | Argentina. | The original study included 452 transgender women. The final analytic sample included a total of 337 (74,6 %) transgender women (278 self-reported HIV negative and 59 with unknown HIV status). | Not reported. | Not reported. | 89.3 % | Not reported. | 2013. |
| Hoagland B, De Boni RB, Moreira RI, Madruga JV, Kallas EG, Goulart S, et al (2017)37. | Brazil. | The final study sample consisted of 1 187 individuals, 95,3 % were male and 4,7 % were trans women. | Not reported. | 61.3 % | 82.1 % | No data: they have measured intention to use PrEP as a proxy of willingness. | 2014-2015. |
*MSM: Men who have Sex with Men. *TG: Transgender. *PrEP: Pre-Exposure Prophylaxis. *PEP:(?), HIVST: Human Immunodeficiency Virus Self Testing. *TGW: Transgender Women. *HIV: Human Immunodeficiency Virus.
Source: own creation.
Supplementary Table 2 Comparative table with sample of MSM and TGW recruited by Berbesy et al.
| Transgender women | Transgender women | Men who have sex with men | Men who have sex with men | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Berbesy F, 20194. | Study PrEP Col. | Berbesy F, 20193. | Study PrEP Col. | |||||||||
| Sample | Medellín | Bogotá | Cali | Medellín | Bogotá | Cali | Medellín | Bogotá | Cali | Medellín | Bogotá | Cali |
| n=217 | n=248 | n=203 | n=49 | n=68 | n=41 | n=447 | n=439 | n=413 | n=186 | n=194 | n=133 | |
| Sociodemographic characteristics | ||||||||||||
| Age (years) | ||||||||||||
| 18-24 | 38.9 % | 21.9 % | 51.9 % | 44.9 % | 23.5 % | 14.6 % | 58.7 % | 52.5 % | 37 % | 39.5 % | 28.9 % | 40.5 % |
| 25-34 | 43.2 % | 36.8 % | 34.6 % | 38.8 % | 44.1 % | 41.5 % | 30.2 % | 31.4 % | 28.8 % | 42.2 % | 43.3 % | 45 % |
| 35-44 | 6.1 % | 13.3 % | 6.9 % | 8.2 % | 14.7 % | 14.6 % | 7.4 % | 6.2 % | 11.9 % | 10.3 % | 17 % | 8.4 % |
| >45 | 11.7 % | 28 % | 6.6 % | 8.2 % | 17.7 % | 29.3 % | 3.7 % | 9.9 % | 22.3 % | 8.1 % | 10.8 % | 6.1 % |
| Socioeconomic stratum | ||||||||||||
| 0 to 3 | 86 % | 97 % | 87.1 % | 95.9 % | 100 % | 95.1 % | 88.2 % | 87.9 % | 86 % | 79.6 % | 79.8 % | 72.2 % |
| 4 to 6 | 6.1 % | 2.8 % | 11.2 % | 4.1 % | 0 % | 4.9 % | 11.8 % | 12.1 % | 14 % | 20.4 % | 20.2 % | 27.8 % |
| Missing | 7.9 % | 0.2 % | 1.7 % | 0 % | 0 % | 0 % | ||||||
| Education level | ||||||||||||
| None or Primary school | 13.7 % | 14.7 % | 15 % | 24.5 % | 25 % | 17.1 % | 2.3 % | 3.9 % | 6 % | 8.1 % | 13.4 % | 8.3 % |
| Less than secondary school | 46.90% | 48.50% | 26.80 % | |||||||||
| Secondary school | 74.70% | 70.90 % | 67.60 % | 22.50% | 19.10% | 41.50 % | 30.10% | 23.00 % | 48.80 % | 25.80% | 20.10 % | 21.10 % |
| Technical | 10.10% | 6.60% | 11.60 % | 6.10 % | 5.90% | 12.20 % | 8.50 % | 17.80 % | 26.20 % | 19.40% | 18.60 % | 24.10 % |
| Some university studies | 0.00 % | 1.50% | 0.00% | 11.30% | 10.30 % | 8.30% | ||||||
| University - postgraduate | 1.60 % | 7.80% | 5.60% | 0.00 % | 0.00% | 2.40% | 49.10% | 55.20 % | 19.10 % | 29.00% | 24.70 % | 24.10 % |
| Civil status | ||||||||||||
| Single | 88.50% | 74 % | 76.40 % | 81.60% | 82.40% | 87.80 % | 88.10% | 85 % | 83.80 % | 89.30% | 81.40 % | 76.70 % |
| Married - Free Union | 11.60% | 20.20 % | 21.60 % | 18.40% | 17.70% | 12.20 % | 11.30% | 14.40 % | 15.10 % | 9.20 % | 18.00 % | 21.80 % |
| Separated/divorced | 4.10% | 0.00 % | 0.00% | 0.00% | 0.70 % | 0.60% | 11 % | 1.10 % | 0.00% | 0.80% | ||
| Widowed | 1.90% | 2 % | 0.00 % | 0.00 % | 0.00% | 0.50 % | 0.5 % | 0.8 % | ||||
| Coexistence | ||||||||||||
| Alone | 35.90% | 59.50 % | 26.50 % | 30.60% | 58.80% | 36.60 % | 10.70% | 20.40 % | 27.10 % | 30.60% | 58.80 % | 36.60 % |
| Family / non family | 76.70% | 44.60 % | 61.30 % | 55.10% | 23.50% | 61.00 % | 78.80% | 65.90 % | 61.70 % | 55.10% | 25.00 % | 61.00 % |
| Sons | 3.00 % | 9.70% | 0.00 % | 1.50% | 0.00% | |||||||
| Husband/Permanent Partner | 11.90% | 33.80 % | 20.60 % | 14.30% | 16.20% | 2.40% | 10.50% | 13.70 % | 11.30 % | 14.30% | 16.20 % | 2.40% |
| Occupancy in last seven days* | ||||||||||||
| Working as an employee or freelancer | 70.7 | 61.10 % | 77.4 | 0.00 % | 0.00% | 0.00% | 37.90% | 50.10 % | 57.20 % | 60.20% | 59.30 % | 54.10 % |
| Working | 73.50% | 35.40% | 46.30 % | |||||||||
| Not working but had a job | 0.7 | 0.60% | 0.2 | |||||||||
| Voluntary work | 10.20% | 2.90% | 2.40% | 4.80 % | 2.10% | 3.80% | ||||||
| Looking for work | 5.9 | 9.90% | 3.2 | 8.00 % | 11.50 % | 11.90 % | ||||||
| Not working, not looking for work | 6.7 | 8.10% | 0.3 | |||||||||
| Unemployed | 10.20% | 20.60% | 14.60 % | 17.20% | 23.20 % | 19.60 % | ||||||
| Studying | 7.20 % | 3 % | 4.30% | 6.10 % | 4.40% | 2.40% | ||||||
| Studying and working | 2.70 % | 1.10% | 5.70% | 38.20% | 27.90 % | 17 % | 26.90% | 15.50 % | 29.30 % | |||
| Not working because she is a pensioner, retiree or annuitant | 1.00% | 0.00 % | 0.00% | 0.00% | ||||||||
| Household activities | 5.70 % | 9.20% | 5 % | 2.00 % | 0.00% | 2.40% | ||||||
| Unable to work | 0.50 % | 0.60% | ||||||||||
| Other | 0.2 | 6.40% | 2.7 | 0.00 % | 45.60% | 31.70 % | 15.90% | 10.50 % | 14 % | 5.90 % | 11.30 % | 10.50 % |
| Ethnicity* | ||||||||||||
| Afro-Colombian, Afro-descendant, mulatto | 8.80 % | 6.20% | 30.40 % | 3.30 % | 6 % | 15.60 % | ||||||
| Other (Indigenous, Room-Gypsy, Raizal from San Andres, Palenquero from San Basilio) | 4 % | 6.40% | 8.00% | 1 % | 2.60% | 3.60% | ||||||
| None of the above | 86.80% | 87.30 % | 61.60 % | 95.70% | 91.30 % | 80.80 % | ||||||
| Monthly income (colombian money) | ||||||||||||
| No income | 16.60% | 14.30 % | 8.20% | 16.30% | 19.10% | 19.50 % | 35 % | 24.40 % | 14.30 % | 16.10% | 19.10 % | 20.30 % |
| Between $15,000 and $828,000 | 47.50% | 59.90 % | 53.40 % | 34.70% | 35.30% | 46.30 % | 24 % | 35.20 % | 42.30 % | 29.00% | 25.80 % | 28.60 % |
| Between $828,001 and 1,644,160 | 20 % | 16.00 % | 25.60 % | 46.90% | 39.70% | 31.70 % | 31.20% | 28.90 % | 35 % | 30.70% | 27.80 % | 26.30 % |
| Over $1,644,160 | 16 % | 9.80% | 12.80 % | 2.00 % | 5.90% | 2.40% | 9.80 % | 11.50 % | 8.40% | 24.20% | 27.30 % | 24.80 % |
| Main source of income | ||||||||||||
| Hairdresser, stylist, beautician | 19.80% | 23.80 % | 18.20 % | |||||||||
| Dressmaker, designer, seamstress | 1.90 % | 0.30% | 6.10% | |||||||||
| Employee | 4.60 % | 7.30% | 12,10 % | |||||||||
| Shows | 6.80 % | 1.50% | 13.30 % | |||||||||
| Sex work | 41,20% | 26.30 % | 1.10% | |||||||||
| Free-lance | 4.40 % | 17.00 % | 9.20% | |||||||||
| No income | 16.10% | 10.20 % | 4.60% | |||||||||
| Other | 5.10 % | 13.50 % | 35.50 % | |||||||||
| Health insurance | ||||||||||||
| Contributive- Subsidised-Special | 82.40% | 89.20 % | 82.80 % | 79.60% | 83.80% | 90.20 % | 96.50% | 95.00 % | 92.60 % | 90.90% | 87.10 % | 85.00 % |
| Not affiliated | 17.60% | 10.80 % | 17.30 % | 20.40% | 16.20% | 9.80% | 3.40 % | 5 % | 7.40% | 9.10 % | 13.00 % | 15.00 % |
| Risk behaviors | ||||||||||||
| Number of people with whom you have had penetrative, non commercial intercourse in the last 12 months* | ||||||||||||
| None | 6.70 % | 1.90% | 1.20% | 8.20 % | 47.10% | 14.60 % | 12.80% | 18.40 % | 12.70 % | |||
| 1 to 4 persons | 17.50% | 27.00 % | 36.30 % | 40.80% | 22.10% | 24.40 % | 55 % | 47.40 % | 58.90 % | 62.20% | 51.40 % | 55.60 % |
| 5 to 10 persons | 12.20% | 11.20 % | 23.70 % | 8.20 % | 10.30% | 14.60 % | 32.70% | 30.50 % | 27.30 % | 9.90 % | 13.90 % | 19.00 % |
| Over 10 persons | 63.60% | 59.90 % | 38.90 % | 42.90% | 20.60% | 46.30 % | 12.30% | 22.10 % | 13.80 % | 15.10% | 16.20 % | 12.70 % |
| Have you ever in your life received money in exchange for sex?* (Yes) | 87.10% | 70.50 % | 84.50 % | 11.60% | 11.10 % | 25.90 % | ||||||
| Condom | ||||||||||||
| Do you use condoms?* (Yes) | 90.40% | 84.20 % | 84.00 % | |||||||||
| Why have you used condom?* | ||||||||||||
| Comfort | 1.30 % | 31.70 % | 17.80 % | 12.50% | 52.10 % | 12.20 % | ||||||
| Custom | 1.20 % | 43.20 % | 20.10 % | |||||||||
| Preventing STIs/HIV | 94.30% | 97 % | 97.10 % | 88.30% | 95.20 % | 85.50 % | ||||||
| To prevent pregnancy | 0.40 % | 5.90% | 5.10% | 2.80 % | 4 % | 2.10% | ||||||
| Hygiene | 11.80% | 63.40 % | 35.60 % | |||||||||
| I live with HIV | 2 % | 15.20 % | 4.90% | |||||||||
| My partners demand it of me | 1.60 % | 13 % | 4.70% | |||||||||
| To care for my partner | 8 % | 27.60 % | 15.10 % | |||||||||
| For my care | 32.80% | 89.50 % | 44.10 % | |||||||||
| Other | 5.70 % | 5.20% | 7.30% | 6.80 % | 21.20 % | 17.60 % | ||||||
| PrEP knowledge | ||||||||||||
| Have you heard of pre-exposure prophylaxis or PrEP? (Yes) | 9.90 % | 5.60% | 4.80% | 14.30% | 32.40% | 31.70 % | 27.10% | 39.40 % | 15.30 % | 55.10% | 59.60 % | 59.10 % |
| Have you ever taken pre-exposure therapy? (Yes) | 4.10 % | 2.70% | 1.10% | 0.00 % | 10.60% | 12.20 % | 1.70 % | 5.70% | 4.50 % | 12.90% | 7.90% | |
| Would you take PrEP to help prevent HIV? (Yes) | 39.50% | 45.50 % | 68.90 % | 65.30% | 61.80% | 61.00 % | 63 % | 40.20 % | 73.10 % | 65.30% | 61.80 % | 61.00 % |
* Items asked differently or not requested in the PrEP-Col study: a. How many men (including gay, transgender, transsexual, transvestite, transsexual, transsexual) have you had anal sex within the last six months?
Source: own creation.
Conclusions
PrEP is an acceptable and feasible HIV prevention strategy for reducing HIV incidence in Colombia. PrEP awareness remains low in MSM and TGW in Colombia, yet a large proportion of PrEP-eligible individuals in this group would likely consider taking PrEP. Working on awareness and other early stages of the motivation cascade are needed to ensure that most people eligible for PrEP can initiate and adhere to it. PrEP implementation in Colombia will need a multilevel intervention to address structural factors that would otherwise hinder PrEP adoption and uptake: this includes a multimodal socialization and education campaign, publicly funded PrEP medication and care continuum, and monitoring of relevant outcomes.

















