Introduction
Ultrasound has shown its usefulness in the management of inflammatory joint disease, particularly of rheumatoid arthritis (RA),1-6 both in the early and late phases, not only in the diagnostic process, but also in the assessment of the damage, the progression and the evaluation of treatments.
It has demonstrated to be more sensitive than the physical examination when evaluating the presence of synovitis, (7-11) and for this reason the scientific societies such as the European League Against Rheumatism (EULAR) include it in their recommendations to improve diagnostic certainty. (9 In addition, in the established disease it detects subclinical activity, which is predictive of both structural damage and appearance of subsequent crises. (12-14
However, the evidence of its usefulness using patient-derived outcomes is scarce. (15,16 One study found that there was a relationship between the ultrasound activity status and anxiety, pain, and morning stiffness. (15 Regarding the assessment of the quality of care or the influence that may exist on patients satisfaction with the use of ultrasound, three studies were found that evaluated both patients and physicians. Of these studies, two evaluated the satisfaction of the patient without annotated diagnoses in relation to the use of ultrasound for joint aspiration or intra-articular injection, and found that it helps the vast majority of them to understand the procedure and improves the anxiety related thereof. Ultrasound was perceived to be more effective than non-ultrasound-guided therapy and patients were more likely to undergo similar new procedures. (17,18
The third study analyzed the opinion of a group of patients with RA, regarding ultrasound, to which they were subjected rigorously to assess the activity of their disease. The authors found that most patients (80-90%) consider a reasonable ultra-sound duration time to be 20-30 min. Likewise, they found greater satisfaction with the care and a perception of the treatment as safer. (19 An inconvenience found was the use of non-endorsed or standardized tools for the evaluation of satisfaction.
The quality of service has several definitions; however, the most widely accepted is that of Parasuranam et al., (20 which considers it a construct resulting from the comparison of the expectations or desires of the consumer vs. those of a provider and his/her perceptions of the service received. (21 Given its importance, several methods have been developed to measure the quality of service, such as Servperf, Servqual22-24 and Servqhos, (25,26 the latter for the specific measurement of the health sector. The Servqhos has been practiced in hospital, dialysis, surgical and outpatient areas, (27-33 without results in the areas of rheumatology or diagnostic imaging. This instrument is validated in Colombia, where it has been already applied. (34
In the Colombian model, governed by Law 100 of 1993, the quality of health care is part of the aspects that must be measured by health providers to achieve quality standards and compete with each other for users. (35 The data show that 67% of the people identified as ill who did not use health services had as the first reason the poor quality of the service. (36 In addition, the Bulletin 018 of the Office of the Attorney General of the Nation, 2007, considered that the main failings of health service provider companies were the inhumane treatment given to patients, the discrimination and the disproportionate demands to access the service.
The objectives of the study are to determine the degree of satisfaction with the health care of a group of patients with RA, who underwent an ultrasound during the consultation, as well as to evaluate whether it is superior compared to that of a group of patients who did not undergo this procedure, through the Servqhos questionnaire and with the hypothesis that ultrasound would have positive effects in the assessment of the quality of care and would improve the parameters of satisfaction.
Methods
An observational cross sectional descriptive study which included patients over 18 years of age with a diagnosis of RA by the ACR/EULAR classification criteria, who underwent a musculoskeletal ultrasound for the study of RA during the medical consultation in a Colombian institution in the period between March and August, 2019, was carried out. Patients with RA who did not undergo ultrasound during the consultation were included as a comparator group. Patients in whom ultrasound was performed as a guide to procedures or at a time other than the outpatient consultation were excluded, in addition to those who had difficulties or did not accept to answer the questionnaire.
At the discretion of the treating physician, during the consultation, it was considered to perform an ultrasound to determine clinical aspects related to RA or its musculoskeletal complications. The procedure was carried out by the treating physician himself, and there was no limit for the number of studies or time. A GE Logic S5 equipment, linear transducer of 7-13 MHz, gains of 50-70%, and Doppler with PRF 0.7, adjusted gain, was used. After the medical act and with the acceptance by the patient, the Servqhos questionnaire (Appendix B annex 1) was delivered, whether or not the ultrasound had been performed. In the event that the ultrasound had been carried out, the patient was also asked to answer the non-standardized questionnaire on the perception of ultrasound (Appendix B annex 2).
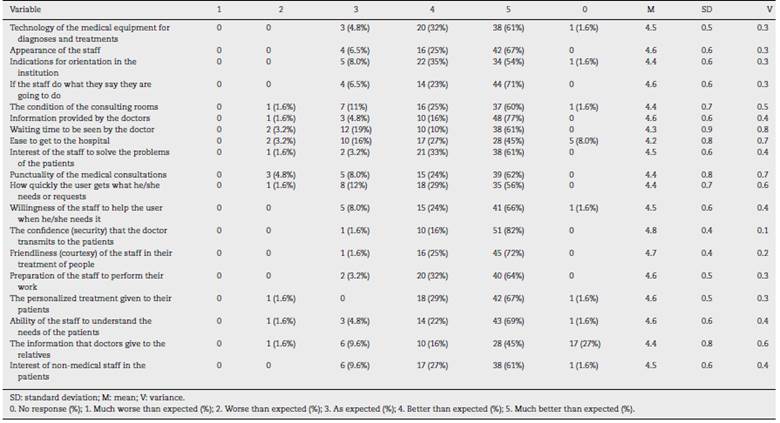
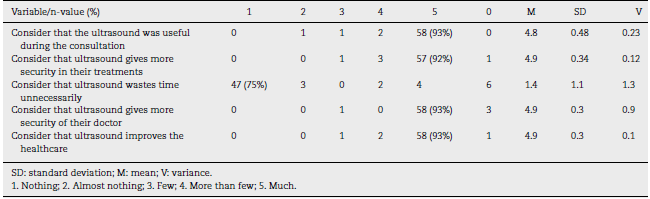
The Servqhos survey consists of 19 ordinal categorical variables that assess the quality of the healthcare service, each of which is scored on a Likert scale ranging from 1 (it has been much worse than I expected) to 5 (it has been much better than I expected). The ultrasound perception survey is conducted using five ordinal categorical variables, and each of these is scored on a Likert scale ranging from 1 (nothing) to 5 (much).
The information bias was controlled by training the interviewers. It was carried out a pilot test in which the procedures were standardized and changes were allowed in case that is required. Source biases were controlled by sensitizing all respondents on the need of answer the totality of the survey, in addition to provide assistance when necessary. A satisfied patient was defined as one who scored 70% or more on the questions of the Servqhos questionnaire with a score higher than or equal to 4. The maximum satisfaction was defined as a score of 5 in a question of this questionnaire. A sample size was calculated based on the a priori hypothesis of finding differences of 20% between the proportion of satisfied vs. dissatisfied patients, with an alpha error of 0.05 and a two-tailed power of 80%. Thus, a size of 62 research subjects in each group was estimated. In addition, a description of the general population was carried out.
Subsequently, a univariate analysis was made according to the distribution in the groups with or without performance of ultrasound, after which a bivariate analysis of the different questions was performed according to the distribution in the groups of satisfaction and very high satisfaction. The variables were described according to their nature assessed by the Shapiro Wilk test: the categorical ones in relative and absolute frequencies, the numerical ones according to their distribution, the normal ones with mean and standard deviation, and the non-normal ones with median and interquartile range. It was established if there was some grade of association with the chi-square tests for the categorical variables, while in the case of the numerical ones, parametric (Mann Whitnney U) and no parametric (Kruskal-Wallis) tests were performed according to the distribution.
The database was collected in Microsoft Excel and the data analysis was performed with the Stata 12.0 statistical software. The work follows the scientific, technical and administrative standards for health research, especially in human beings, set forth in Resolution 8430 of 1993 of the Colombian Ministry of Health, which are in relation to international regulations. It was considered a risk-free study and voluntary and anonymous participation was notified in the questionnaire.
Results
A total of 126 patients were obtained, of whom two were excluded from the analyzes given that they did not answer more than 50% of the questions. Of the remaining 124, 62 correspond to the group of patients to whom an ultrasound was performed during the consultation and 62 to the control group, in whom the procedure was not performed. The mean age of the ultrasound group was 57.4 years and that of the control group was 55.9, with no differences between the groups (p = 0.36). Regarding the gender, the majority of patients were women, 93.5% in the ultrasound group and 88% in the control group, with no differences among them (p = 0.89).
The reason why the physician considered to perform an ultrasound was for the study of joint pathology in 58 patients (93%), tendon pathology in 14 of them (22.5%) and study of bursae in 8 cases (12%). In 20 patients (32%) ultrasound was used to assess two or more of the described aspects.
In the completion of the Servqhos questionnaire, of a total of 1178 responses in each group, there was no response in 29 in the ultrasound group (2.4%) and in 29 in the control group (2.4%). Question number 18, which makes reference to information to the family, was the one that had the most missing data, with 19%, without being excluded from the analysis.
The results in the ultrasound group are presented in Table 1. The majority of responses were positive in almost all aspects of care. The questions featured with a high number of responses with the best value responses were: medical equipment, 61%; appearance of the personnel, 67%; information of the physician, 77%; confidence in the doctor, 82%, and kindness of the staff, 72%.
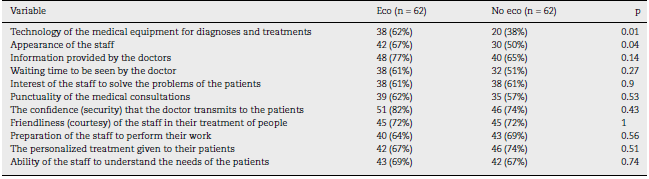
The results of the Servqhos in the control group are presented in Table 2. Most responses were positive, similarly than in the ultrasound group. Based on these results, it was found that in those to whom the ultrasound was performed, the number of satisfied patients was 56 (90%), while in the control group it was 48 (77%).
The difference in the proportion of satisfied patients between the groups was 13%, being statistically significant in favor of the patients to whom the ultrasound was performed (p = 0.05). The analysis of the relationship between the age and the state of satisfaction did not show that there was such asso-ciation (p = 0.99), as well as in the case of the gender variable (p = 0.12).
Table 3 summarizes the differences between the groups in specific questions of the Servqhos questionnaire that make reference to medical care, and that may be more related to the ultrasound procedure, taking into account the number of patients who rated them with the highest degree of satisfaction, defined as 5. Table 3 shows that in questions 1 and 2 of the questionnaire, which refer to the technology of the medical equipment and the appearance of the staff, there is a statistically significant difference (p < 0.05).
The non-standardized survey to assess the perception regarding ultrasound of the patients who underwent the procedure obtained the results that are summarized in Table 4. According to these results, there was a very good acceptance, considering that it was useful, with the highest qualification, in 93%; that greatly improves the safety of their treatments and of their physician, with 92%, and that improves care, with 93%.
Discussion
The level of satisfaction measured is high in both groups, but it is higher in the ultrasound group, being statistically significant, which may be due to the impact on people with the use of equipment during the medical act, the direct visualization of the pathology and the additional diagnostic and resolutive possibility that ultrasound allows. In general, this enables the physician to report in a more explicit and detailed manner the health status of each patient, which could be reflected in the analysis of the individual assessment of variables considered more related to the medical act and ultrasound, such as the use of medical equipment and the presentation of the staff, which were higher in the intervention group, in addition to a tendency to be higher in others, such as the medical information or the friendliness of the staff. Likewise, the vast majority of patients consider that it is useful, generates more confidence in the physician and the treatment, in addition to improving care. Similar results were obtained in studies such as the one of Ceponis et al. (19 in patients also with RA who underwent ultrasound at a time different from that of the medical consultation
This is the first study that shows that ultrasound improves the parameters related to the quality in the provision of medical service and their perception by the patient, which is essential for the individual well-being, favorable results also demonstrated in the use of ultrasound for patients who undergo arthrocentesis. (17,18
One of the strengths of the study is the use of the Servqhos tool, an instrument validated in various populations, including that of Colombia, (34 which will allow to make comparisons in future studies, in addition to the use of musculoskeletal ultrasound during consultation by the treating physician himself, which is important for the short-term medical decision making.
Regarding the limitations, there is a possible selection bias, since there is no control over whom the ultrasound is performed or the reasons for its use. Likewise, it cannot be generalized to other population groups, with diagnoses other than RA, a high degree of satisfaction with care in general, which may make the difference much smaller, and the use of the non-validated survey for the perception of ultrasound.
The conclusion of the study is that in patients with RA, musculoskeletal ultrasound at the time of medical consultation improves the perception of quality in health in general, as well as the perception specifically regarding the medical equipment and the presentation of the personnel. In addition, the perception of the ultrasound in those who undergo the procedure is good, it gives them more confidence in their doctor and improves the quality of care.











 text in
text in