Remark
| 1) Why was this study conducted? |
| This article aims to describe the experience earned by the Trauma and Emergency Surgery Group (CTE) of Cali, Colombia in the management of the severely injured trauma patient in the emergency department following the basic principles of damage control surgery. |
| 2) What were the most relevant results of the study? |
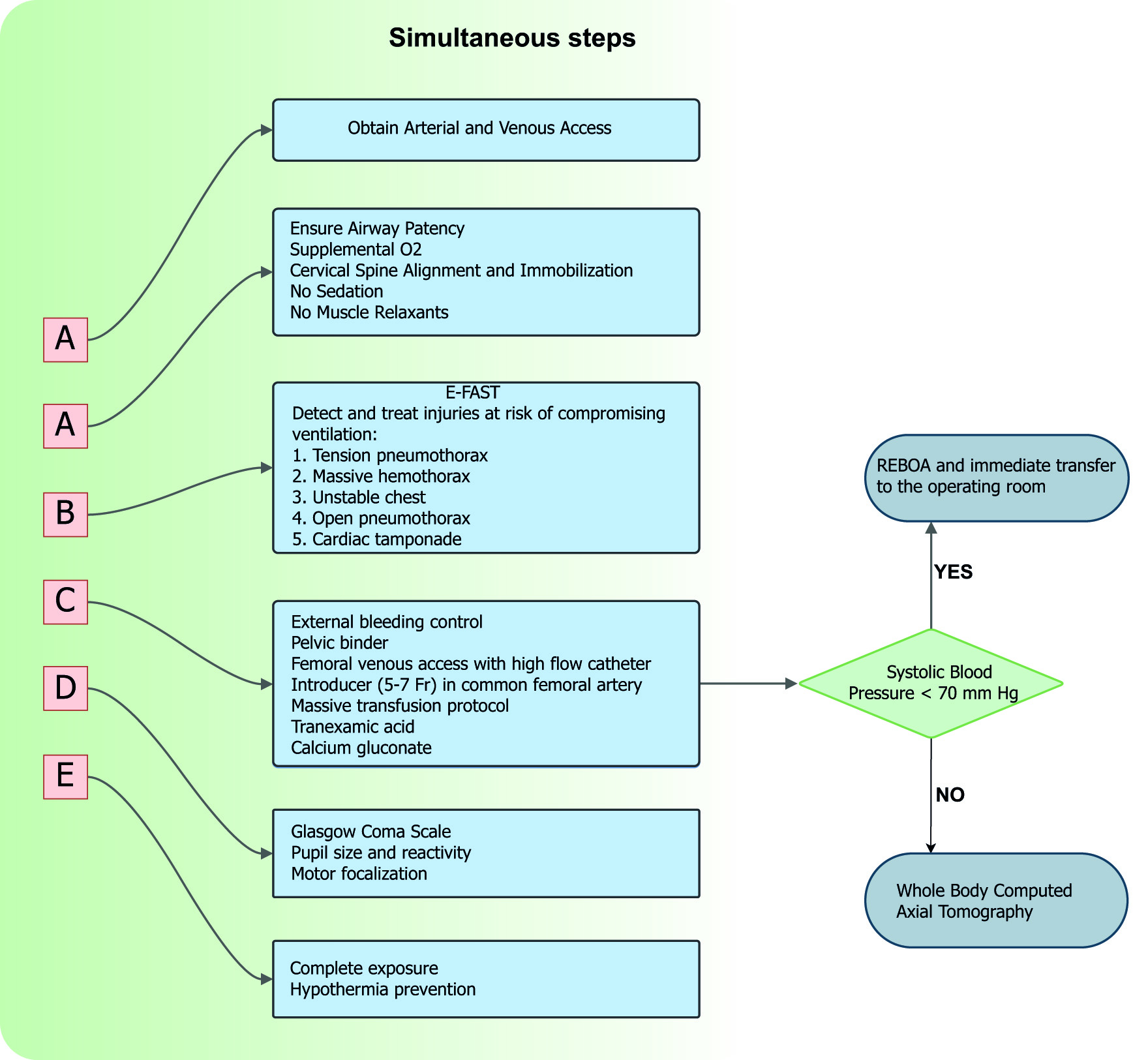
| The ATLS guidelines describe the A-B-C-D-E sequence, which consists of a clear and simple approach for severely injured trauma patients. Novel A-A-B-C-D-E sequence, where the initial "A-A" refers to achieving arterial and/or venous vascular access and airway control. Vascular access in common femoral artery and common femoral vein should be strategy to establish a way for massive transfusion protocol, invasive monitoring, and potential REBOA use. |
| 3) What do these results contribute? |
| The management of the severely injured trauma patient in the emergency department requires a multidisciplinary team that performs damage control maneuvers aimed at rapidly controlling bleeding, hemostatic resuscitation, and/or prompt transfer to the operating room, if required. |
Introduction
Patients with hemodynamic instability have a sustained systolic blood pressure less or equal to 90 mmHg, a heart rate greater or equal to 120 beats per minute and an acute compromise of the ventilation/oxygenation ratio and/or an altered state of consciousness upon admission. These patients have higher mortality rates due to massive hemorrhage, airway injury and/or impaired ventilation 1. Damage control resuscitation is a systematic approach that aims to limit physiologic deterioration through strategies that address the physiologic debt of trauma 2. The initial maneuvers implemented in the emergency department are: a primary survey by an experienced trauma team, diagnostic adjuncts such as chest X-ray, pelvic X-ray and Focused Assessment with Sonography for Trauma - FAST), temporary hemorrhage control maneuvers (tourniquet or pelvic binder/sheet), peripheral and central vascular accesses, massive transfusion protocol activation and endovascular aortic occlusion with the Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) 3,4.
This article describes the experience earned by the Trauma and Emergency Surgery Group (CTE) of Cali, Colombia, in managing severely injured trauma patients in the emergency department following the basic principles of damage control surgery. Therefore, a consensus was made to synthesize the experience earned during the past 30 years in trauma critical care management from the Trauma and Emergency Surgery Group (CTE) of Cali, Colombia, including experts from the the Universidad del Valle, University Hospital del Valle "Evaristo García", University Hospital Fundación Valle del Lili, Universidad Icesi and, the Asociación Colombiana de Cirugía, the Pan-American Trauma Society and the collaboration of international specialists of the United States of America and Latin America.
Epidemiology
Lozano et al.5, in a systematic analysis about the Global Burden of Disease between 1990 and 2010 found that 5.1 million people died as victims of trauma with an increase over the decades from 8.8% in the early 1990s to 9.6% by 2010. These trauma deaths affect predominantly young people with a large impact on economically useful life expectancy 5,6. According to the Global Burden of Diseases, Injuries, and Risk Factors Study in 2019 (GBD 2019) the deaths from traumatic injuries decreased by 1.11% from 2010 to 2019.
Concepts
The damage control strategy began around 1993 by Rotondo et al.2, who established three stages for the approach to severely injured trauma patients. Stage I consists of the control of bleeding and/or contamination, abdominal packing and temporary cavity closure; stage II in resuscitation and physiologic restoration in the intensive care unit and Stage III in surgical re-exploration, treatment and definitive closure. Subsequently, Johnson and collaborators included the prehospital scene as stage zero being crucial for adequate patient care 7. Another fundamental concept in trauma is the lethal triad which includes: hypothermia, coagulopathy and acidosis secondary to acute physiological deterioration 8. This concept was also expanded by Ditzel et al.9, proposed the lethal diamond of death with hypocalcemia as another fundamental concept.
During the last decades, the development and implementation of new diagnostic tools such as FAST and the whole body computed tomography provided important information that allows quick and organized decision-making with a highly detailed evaluation 10,11. On the other hand, bleeding control and hemostatic resuscitation with transfusion of red blood cells, plasma and platelets in a 1:1:1 ratio have shown better results in restoring intravascular volume and hemostatic balance 12. These maneuvers with the permissive hypotension avoid hypothermia, clotting factors dilution and blood loss from uncontrolled sources while maintaining sufficient blood pressure to ensure coronary and cerebral perfusion 13.
Also, REBOA has been consolidated as an additional endovascular tool that aids in the early control of hemorrhage and hemodynamic support 14,15. In the United States of America, REBOA has been used for infra diaphragmatic injuries; however, our experience has shown promising clinical results even in thoracic trauma 16,17. It is important to note that to carry out all the measures mentioned above. It is necessary to integrate a multidisciplinary trauma team, trained and organized and headed by a Trauma Surgeon who leads continuous and effective management.
Damage control in the emergency department
The ATLS guidelines describe the A-B-C-D-E sequence, which consists of a clear and simple approach for severely injured trauma patients. This organized management allows a simultaneous evaluation by different members of the team with a certain degree of overlap between the phases. Recently, some authors proposed a modification to the ATLS sequence due to the advent of endovascular therapies; they suggest a new A-A-B-C-D-E sequence, where the initial "A-A" refers to achieving arterial and/or venous vascular access and airway control (Figure 1).
A persistent systolic blood pressure of 70 mmHg or less despite hemostatic resuscitative maneuvers is an indication for aortic occlusion and transfer to the operating room 13,18.
ATLS assessment and resuscitation sequence: ABCDE
A: the airway should be protected and adequate ventilation should be secured. Supplemental oxygen must be administered to all severely injured trauma patients to achieve a 94-95% target saturation. Positive pressure ventilation, sedatives and muscle relaxants should be avoided due to its association with early circulatory collapse. In upper airway obstruction, an emergency cricothyroidotomy should be performed and in lower airway injuries, tracheal intubation guided by fiber bronchoscopy should be done. Also, the cervical spine must be protected from excessive mobility to prevent the development of or progression of a deficit.
B: Airway patency alone does not ensure adequate ventilation. Injuries that significantly impair ventilation in the short term include tension pneumothorax, massive hemothorax, unstable thorax, open pneumothorax and cardiac tamponade. The use of an extended FAST exam allows to identify and diagnosis all of these potential life-threatening injuries to treat them promptly and help to choose the optimal surgical management
C: During the primary survey, external hemorrhage should be identified and controlled by direct manual pressure on the wound or a tourniquet placement for an extremity. The internal source of hemorrhage should be managed with urgent surgical or endovascular interventions 19,20. In the hemodynamically unstable patient, both a common femoral vein and artery lines should be placed for intravenous access and blood pressure monitoring 21,22 (Figure 2). Additionally, the institution’s massive transfusion protocol should be activated, which includes four units of red blood cells, four units of plasma, 1 unit of apheresis platelets reserve, 1g of tranexamic acid and 20 ml of 10% calcium gluconate that should be administered according to the coagulation status of the patient 23. If during the initial resuscitation the systolic blood pressure of the patient reaches 80-90 mm Hg, a whole-body computed tomography (WBCT) should be done. This technology has emerged as a highly sensitive and specific diagnostic tool that will aid in the decision-making of the best surgical approach without incurring any delay in definitive management and/or increasing the radiation exposure significantly. On the contrary, if the patient is not responder and systolic blood pressure continues equal or lower to 70 mm Hg, it is indicated to deploy a REBOA and immediately transferred to the emergency room.

Figure 2 Vascular access in the common femoral artery and common femoral vein for a patient with severe trauma should be established vascular accesses. Arterial access with introducer lower 7 Fr, if it is possible, should be placed and a high flow catheter in the common femoral vein to continue the hemostatic resuscitation maneuvers and invasive monitoring. If the patient is a non-responder, REBOA can be placed through arterial access in the common femoral artery.
D: A rapid neurologic evaluation should establish the patient’s level of consciousness, pupillary size and reaction. Also, lateralizing and/or spinal cord injury signs should be identified.
E: full exposure and assessment of the anterior and posterior body space should be performed, followed by measures to prevent hypothermia.
Blood sampling for blood derivative crossmatching, arterial gas processing, fibrinogen, lactate and thromboelastogram will provide baseline values that predict and measure the severity of the trauma. However, resuscitation maneuvers should not be delayed while waiting for their results.
Conclusions
The management of the severely injured trauma patient is a dynamic, high-impact strategy that requires an experienced multidisciplinary team, which must evolve with new diagnostic tools and endovascular treatment reducing the hemodynamic repercussions as a lifesaving approach with higher survival rates.











 text in
text in