Remark
| 1) Why was this study conducted? |
| After beginning of COVID-19 pnademic early projections suggested an outpouring of cancer diagnoses with worse stages, survival, and excessive mortality compared with thpre-COVID-19 scenario, especially in low-and-middle-income countries where cancer care has limited access and might be more heavily affected by the pandemic. However, most studies have been conducted in high-income countries and fail to use observed rather than expected modeled data. |
| 2) What were the most relevant results of the study? |
| Despite a reduced demand following the lock-down, based on real-life data, our study shows that patients have learned from confinement experiences at an accelerated rate, mitigating the initial shock to nearly half the impact during the first COVID-19 peak and almost unnoticeable level for the second peak. We also found a differential impact depending upon type of cancer, type of service and sociodemographic conditions. |
| 3) What do these results contribute? |
| The rapid spread of an emerging and threatening disease led to stringent restrictions with a significant reduction in health services supply and attendance. Our results show the benefits of universal financial protection and the need for close surveillance based on real-life data in such situations, and a proper response to the emergency considering particularities of the impact by type of health service and population groups in order to reduce the negative effect of a general unselective response. |
Introduction
The COVID-19 pandemic has affected health systems worldwide. According to the WHO, up to August 2, 2021, 223 countries and regions reported 198.2 million confirmed cases and over 4.2 million deaths due to COVID-19 1. In Colombia, 4,785,320 COVID-19-positive cases had been confirmed, along with 120,723 deaths by the same date 1. Colombia’s first COVID-19 case was reported on March 6, 2020, followed by nationwide mandatory confinement from March 25 until August 31, 2020, making Colombia´s confinement one of the longest registered globally. In addition, circumstances such as COVID-19 detection and treatment prioritization, contagion fears among the general population and healthcare workers, bed space allotment to COVID-19 patients 2-4, strict lockdowns with travel restrictions, healthcare resources allotment 5 and secondary economic derangement, have led to reduced access to healthcare services.
Cancer patients are considered a high-risk group for COVID-19; hence, oncology centers have implemented measures to reduce their exposure to potential contagion in healthcare facilities (2). However, oncological diseases are time-sensitive regarding diagnosis and treatment 6, and some reports indicate that the pandemic has led to delayed treatment start dates 7, with projection models showing increased mortality secondary also to diagnostic delay 6. Furthermore, compared to 2019, reductions have been described in new patient registrations, follow-up visits, hospital admissions, outpatient chemotherapy, surgeries, pathological and radiological diagnosis, palliative care referrals, and almost halted cancer screening due to the COVID-19 pandemic 5.
The cancer service demand reduction has been described for different settings 7-10; however, most studies have been conducted in high-income countries, with no clear description of changes in health service supply and without real-life data based on early 2020 estimates. Thus, they do not necessarily reflect the long-term pandemic effects 5. Moreover, most studies fail to use observed rather than expected data on disease staging as the basis for prognosis and projections, especially in low-and-middle-income countries (LMIC), where cancer care access is limited and might be more heavily affected by the pandemic 5,11.
Colombia, a middle-income country, has a mandatory health insurance model with private and public insurers equivalent to USA’s HMOs. In 2017, insurance rates reached 94.4% for the two main insurance plans: the contributory (payroll) system for formal workers and their relatives and the subsidized system for low-income populations lacking payment capacity 12. Health insurance companies implement their health service networks using their health centers or agreements with independent healthcare providers. Both insurance plans deliver health care based on the national regulatory benefit package 13.
The Xaverian Oncology Center (CJO for its Spanish name) at the San Ignacio University Hospital (HUSI for its Spanish name) is a specialized center in Bogota providing multidisciplinary cancer care. Comprehensive care is ensured by offering medical and surgical oncology; radiation-oncology; pathology, molecular, and imaging oncology; and supportive care. A model based on specialized cancer units has been implemented for breast, gastrointestinal, thoracic, and urologic neoplasms. Between 2,500 and 3,000 new cancer cases access the CJO yearly 14. The CJO implemented measures to reduce the risk of SARS-Cov-2 contagion among patients without reducing the service supply. Therefore, this study utilizes real-life data to analyze the COVID-19 pandemic impact on oncology service demand in a middle-income setting without economic access restrictions (granted by universal insurance coverage), at a reference center with comprehensive cancer care supply.
Materials and Methods
We performed a time trend analysis based on data from the CJO-HUSI (Bogota-Colombia). Data were collected on new patient visits for cross-cutting services and specialized multidisciplinary units, follow-up visits for cross-cutting services, hospital discharges after in-hospital systemic therapy, ambulatory delivery of systemic therapy, radiotherapy, oncological surgery, and bone marrow transplant (BMT). Cross-cutting services correspond to outpatient visits for clinical oncology (solid tumors), hematology, radiation oncology, and palliative care, and specialized multidisciplinary services include the breast, stomach, prostate, and lung cancer clinics.
We collected data from January 1st-2017, to December 31th-2021 Aggregated monthly data asthe number of visits/procedures were retrieved from institutional databases, including the inpatient HUSI system (SAHI), outpatient HUSI system (Capacidades), and outpatient CJO system (SAHICO). Additionally, the clinical stage at diagnosis was obtained from databases of specialized multidisciplinary clinics. Only data linked to new cases in each time series were considered (2017, 2018, 2019, 2020, 2021). They were filtered by first-consultation date (cross-cutting services and multidisciplinary cancer units), histopathological diagnosis date (cancer staging), and treatment delivery date (systemic therapy, radiotherapy, surgery).
Data analysis
A temporal series analysis was performed as a sequence of the number of monthly observations (equidistant chronologically) and their percent variation for each service category separately 15.
To identify seasonal variations for cross-cutting services, multidisciplinary units, and treatment delivery, we report monthly trends in total numbers for the average between 2017-2019 and for the years 2020 and 2021. Additionally, for every service, we estimated percent change month-by-month during 2020 and 2021 compared to the annual average for the corresponding service during 2017-2019, exception made for oncology surgery, for which information was only available since 2019. In doing so, we can compare the magnitude of the impact for different service categories, regardless of the total number of observations in every service analyzed. The percent change was also estimated globally by sex and age groups for cross-cutting services.
We used the endemic channel quartiles method to provide information on the significance of monthly changes. Based on 2017-2019, we defined the alarm zone below quartile 2, the secure zone between quartiles 1 and 3, and the secure zone above quartile 3.
The clinical stage at diagnosis, defined per the AJCC-UICC 8th edition 16, was grouped for pre-confinement (January-March), confinement (April-August), and post-confinement (September-December) periods during 2020 and for the year 2021. Percentages of stages I through IV for breast, stomach, prostate, and lung cancer are reported, assuming, for comparative purposes, stages I-II as early disease and III-IV as advanced disease. Similarly, we retrieved data for multiple myeloma.
We analyzed trends in service demand in the post-confinement period up to June 2021 (10 months). First, we estimated monthly percent change (MPC) using a Log transformation option 17. Thus, percentages are assumed to change at a constant percentage of the values in the previous month, allowing a comparison of trends for services with different demand levels. The MPC was estimated for the entire post-confinement period (September 2020-June, 2021) and the first semester of 2021; this approach aimed to identify service demand variations likely related to administrative changes for the new fiscal year beyond the effect of the COVID-19 pandemic.
Finally, we report the daily COVID-19 diagnosis variations in Colombia as background information for the analysis of oncology service demand. Data on COVID-19 diagnosis are publicly available on the Colombian National Institute of Health website 18.
Results
In total, we registered 629, 1345, and 2006 new patients in hematology, clinical oncology, and radiation oncology, respectively; and we received 1278 new patients for palliative care.
By comparing total numbers for 2017-2019 and 2020 we observed a seasonal variation for outpatient consultations in palliative care, radiation-oncology, and radiotherapy treatment delivery, with decreased numbers in April-May, August-September, and November respectively (Supplementary Figure 1).
Coinciding with the beginning of the confinement, oncology service demand simultaneously decreased in April 2020 for new patients’ first consultations in cross-cutting services (R: -49.0% to -74.5%), in the specialized units (R: -64.9% to -90.0%), and for treatment delivery (R: -14.9% to -85.3%)(Figure 1). Apart from hematology, we again observed a simultaneous decrease in new patients’ first consultations in August 2020 (R: -18.9% to -55.6%), coinciding with a demand reduction in treatment delivery and the first wave of COVID-19 in Colombia (Supplementary Figure 2).

Figure 1 Time trends in percent change of service demand by service category. A: Cross-cutting services. B: Treatment delivery services. Percent variation month by month compared with the 2017-2019 average for each service category. The shadow area represents the period of confinement during 2020. * For surgery, the percent change is estimated based only on data from 2019, given the lack of information for previous years.
A rapid recovery was observed in new patients’ first consultations in cross-cutting services, except for clinical oncology (solid tumors), which remains in the alarm zone for the whole year (Figures 1 and 2). Contrastingly, the recovery was slower in the specialized multidisciplinary units, reaching baseline levels after confinement (Figure 3). However, the breast cancer clinic did not reach baseline levels by the end of 2020. The demand for ambulatory treatment delivery showed no significant impact (systemic therapy and radiotherapy); however, services requiring in-hospital care decreased to -58.4% (oncology surgery) without recovering from the alarm zone to the end of the year (Figures 1 and 2).

Figure 2 Endemic channels of oncology services demand during 2020. A: Cross-cutting services. B: Treatment delivery services. The alarm zone represents a reduction of service demand below quartile 1 of the historical behavior, the secure zone a stable trend in service demand between quartiles 1 and 3, and the success zone an unexpected increase in demand over quartile 3.
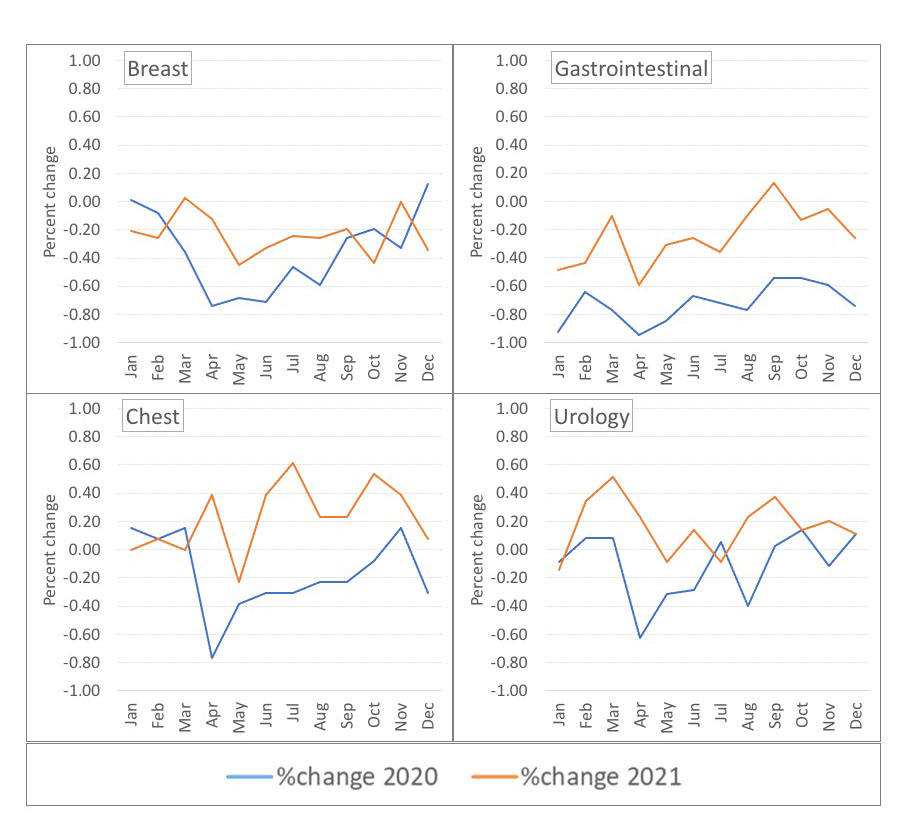
Figure 3 Time trends in percent change by specialized cancer unit. Percent variation month by month compared with the 2017-2019 average per unit
Follow-up visits for patients under treatment showed no pandemic impact on the hematology and clinical oncology (solid tumors); however, radiation-oncology showed a significant decline in April 2020 (-90.7%) and revealed a slow progressive recovery during confinement (Supplementary Figure 3).
Women showed a greater decrease in new consultation demand than men (from -11.7%, on average, down to -26.8% in August versus +7.5%, on average, down to -16.6% in August, respectively). Consistently, the demand for new patients’ first consultations in breast and urology multidisciplinary units showed a greater decrease for the former (average -53.2% vs. -20.7%, respectively). Furthermore, the most significant decrease was observed among patients 70 years and older and the lowest among patients 50 years and younger (Figure 4).

Figure 4 Time trends in percent change of service demand by sex and age. A: Time trends by sex. B: Time trends in specialized units for breast cancer (females) and prostate cancer (males). C: Time trends by age group. Percent variation month by month compared with the 2017-2019 average for demographic/service category
Regarding stage at diagnosis, we observed an early disease decline for breast cancer (66% pre-confinement and 55% post-confinement), with the greatest decrease in stage I (Figure 5). Similarly, early-stage stomach cancer declined from 35% pre-confinement to 13% post-confinement. Early-stage prostate cancer increased by 11% during confinement but returned to baseline post-confinement. Multiple myeloma ISS stage I increased from 7.7% pre-confinement to 28.6% post-confinement. Lung cancer showed a stable distribution of early and advanced disease throughout the year. None of the reported changes is statistically significant.
Except for radiotherapy, the data for 2021 showed a general increase of demand with different monthly patterns for palliative care and clinical oncology consultations. No statistically significant MPC was observed; however, we observed a reduced MPC for the first semester of 2021 compared with the estimated MPC for all ten months post-confinement in new patients’ consultations for the urology multidisciplinary unit and in-hospital systemic therapy (hospital discharges), with a change from a positive to a negative trend in the latter. The remaining services showed either variations below 0.5% between the two periods or a positive trend (Table 1).
Table 1 Monthly percent change after confinement by service category
| Service | Monthly percent change | Monthly percent change |
|---|---|---|
| Sep 2020-Jun 2021 | Jan 2021-Jun 2021 | |
| Cross-cutting services | ||
| Hematology | 1.2 (-2.4; 3.8) | 1.3 (-2.9; 4.3) |
| Clinical oncology | -1.3 (-2.9; 1.6) | -0.5 (-2.3; 1.8) |
| Radio-oncology | 0.0 (-2.3; 2.4) | -0.2 (-2.7; 2.5) |
| Palliative care | 0.8 (-1.6; 2.4) | 1.0 (-1.8; 2.8) |
| Multidisciplinary units | ||
| Breast | -0.7 (-4.0; 3.4) | -1.1 (-4.2; 3.2) |
| Gastrointestinal | 4.2 (-10.6; 16.9) | 8.5 (-10.8; 22.6) |
| Thorax | 0.3 (-0.7; 0.8) | 3.5 (-0.6; 10.4) |
| Urology | 1.7 (-0.4; 0.6) | 1.2 (-0.4; -0.5) |
| Treatment delivery | ||
| Systemic therapy | 0.2 (-0.1; 1.1) | 0.3 (-0.1; 1.2) |
| Hospital discharges | 0.3 (-1.6; 2.5) | -2.2 (-2.0; 2.0) |
| Radiotherapy | -0.8 (-2.5; 1.7) | -0.6 (-2.4; 1.8) |
| Surgery | 1.3 (-1.4; 2.9) | 0.9 (-1.6; 2.6) |
| Bone marrow transplant | 6.3 (-16.2; 27.6) | 9.9 (-14.6; 30.0) |
September 2020-June 2021 corresponds to the whole post-confinement period. Cross-cutting services and multidisciplinary units: new patients’ first consultations. Treatment delivery: patients who underwent the corresponding treatment. Hospital discharges: in-hospital systemic therapy. Systemic therapy: ambulatory delivery of systemic therapy. Green and orange cells indicate a 1.0% or more difference in 2021 (upward or downward, respectively) compared with the whole post-confinement period. BMT: Bone marrow transplant. Monthly percent change estimates based on 17
Discussion
Despite a continuous service supply, in our analysis, the demand for new patients’ first consultations and treatment delivery simultaneously decreased at the beginning of confinement and four months later during the first wave of the COVID-19 pandemic. However, the second decrease was of lesser magnitude without reaching the alarm zone in the endemic channels, except in-hospital care and clinical oncology. Without the latter, we observed a speedy demand recovery for the first consultations before the confinement ended. Regarding the remaining services, the recovery occurred after confinement but before the end of the year, with no consistent decrease during the second wave of the pandemic.
Our results suggest adaptability and learning as the pandemic progressed in cancer services and patients. To our knowledge, this situation has not been previously described; previous reports frequently predicted a sustained negative impact on oncology service demand and, consequently, on the clinical stage at diagnosis and cancer survival 19. However, most studies are based on modeling rather than observed data 6,7,11, and use data from the beginning of the pandemic, when the impact on service demand was greater 5,8) as in recent estimates for Latin America 11,20.
We did not observe a consistent increase in late-stage diagnosis during and after confinement across all cancer types analyzed but only for breast and stomach cancer (Figure 5), albeit not statistically significant. Generally, patients with advanced disease could be more willing to attend health services during confinement due to stronger symptom manifestation, whereas patients with the early-stage disease could delay consultations; however, this does not explain differences between cancer types. Reduced screening and greater impact due to women’s social role may be related to the greater, sustained negative impact for breast cancer 21, as observed for new patient’s first consultations in this specialized unit (sustained decreased but not significantly in 2021 - Table 1) and the stage at diagnosis (sustained early-stage decrease after confinement - Figure 5). Also, these factors are possibly related to the observed differences in sex (Figure 4). Since Colombia does not have mandatory screening for prostate cancer, oncology service demand for this type of cancer is not sensitive to this effect in addition to a different progression rate of the disease. In Colombia, most prostate cancer diagnoses are based on symptoms; thus, staying home during confinement with a different social role and free time compared to women 22, may have increased men’s willingness to seek medical advice. The different ways women and men experience outbreaks and respond to emergencies have been previously noted 23-25, and some COVID-19 studies in LMIC show that women have been less likely to seek health care 26; yet, data from high-income countries show no sex-related differences in pathological cancer diagnosis during the pandemic 27.

Figure 5 Stage of disease at diagnosis regarding the COVID-19 confinement. A: Breast cancer. B: Prostate cancer. C: Lung cancer. D: Stomach cancer. Percentage of the stage at diagnosis during the pre-confinement (January-March), confinement (April-August), and post-confinement (September-December) periods in 2020 and during 2021 (January-December)
Despite not having a screening program, the early-stage stomach cancer decrease could be related to reduced endoscopic examinations, particularly considering the high risk due to potential aerosolization and transmission of SARS-Cov-2 28. A reduction in endoscopic procedures was reported in the USA, where 98.6% of centers delayed elective endoscopies for a mean of 5.8 weeks 29, and in Northern Ireland, where diagnoses of gastroesophageal cancer declined by 26.6% 29. Interestingly, instead of a decrease, early-stage lung cancer showed a slight (not significant) increase throughout the year (Figure 5). This might be related to the increased imaging examinations as part of the COVID-19 diagnostic workup, even in mildly symptomatic patients, accidentally revealing early-stage disease that would otherwise not have been diagnosed. However, further research is anticipated.
The treatment delivery service demand did not impact ambulatory care (radiotherapy and systemic therapy - Figure 1). This finding suggests high adherence to ongoing treatment protocols and is coherent with the lack of impact on follow-up visits as opposed to new patient consultations. Notwithstanding, the lower availability of hospital beds and intensive care units due to the temporary shift of these resources to COVID-19 care negatively impacted treatment delivery requiring in-hospital care (i.e., surgery and hospital discharges) (Figures 1 and 2). These features and the speedy recovery in cross-cutting services demand indicate the positive effect of universal health insurance despite differences in income levels among cancer patients, an asset for cancer care in Colombia.
Nevertheless, the general increase in demand during 2021 might reflect a service backlog during the pandemic, with more cases requiring systemic treatment and palliative care at a later stage of the disease. Furthermore, the capability to adjust treatment protocols might have played a relevant role in response to the outbreak and could explain some differences in service demand, potentially impacting cancer survival. Specifically, we observed a rapid recovery over the previous year regarding first consultations for radiation oncology (Figures 1 and 2), a finding consistent with the increased early-stage diagnosis of prostate cancer, suggesting a shift from surgical to radiotherapy treatment and a possible increase in hypofractionated protocols during confinement 30. Moreover, expert recommendations indicate radiotherapy or chemoradiation during the pandemic for defined cancers (head-and-neck, lung, cervix, prostate, esophageal), leading to an increased radiotherapy demand 14. However, this is not an alternative for other cancer types requiring surgical management or in-hospital care. Hence, due to disease characteristics (incidence, prevalence, clinical course) and flexibility of clinical guidelines, the pandemic differentially affected cancer types, associated population groups, and oncology services (women vs men, elderly vs young, solid tumors vs hematology malignancies, cross-cutting vs specialized units).
Our study has several limitations. First, we analyzed seasonal trends by comparing absolute numbers, finding a coincident decrease during April-May (beginning of confinement) and August-September (first pandemic peak) for newpatients’ first consultations in palliative care and radiation oncology. Nevertheless, we did not make any adjustments based on seasonal effects. We think that comparing every month with the average of the previous year rather than month to month avoids, to some extent, the influence of seasonal variations in percent change estimates and the analysis by endemic channels gives information on significant monthly variations as described. Additionally, as we observed a consistent decrease of all services during these periods in 2020 but not in previous years, we consider the reduction in service demand during 2020 more likely related to the pandemic than to other institutional or contextual factors. However, we cannot prevent the potential effect of administrative changes for the different fiscal years. Indeed, modifications in contractual relationships with health insurance companies reduced the radiotherapy patient numbers (mainly prostate cancer patients) and in-hospital treatment during 2021 (Table 1); however, we declared a lack of statistical significance (around confinement or fiscal years), partially due to the small number of observations (monthly periods).
Finally, our analysis is not population-based but institutional-based; thus, the results should be cautiously interpreted regarding external validity. The CJO operates under the same contextual conditions as all cancer centers in the country, based on contractual relationships with health insurance companies, serving the insured population, and following the legally mandated benefit package. Despite common rules, a variation could exist by insurance type (contributory or subsidized) and efficiency of health insurance companies; consequently, our data could better represent patients in the contributory system (90% of patients at CJO-HUSI) and affiliates to the largest insurance companies possessing national representation.
Conclusions
It is still early to determine the COVID-19 precise impact on cancer diagnosis, treatment, and mortality. Some Latin American projections suggest an outpouring of cancer diagnoses with worse stages, survival, and excessive mortality compared with thpre-COVID-19 scenario 11,31. Based on real-life data, our study shows that patients have learned from confinement experiences at an accelerated rate, mitigating the initial shock to nearly half the impact during the first COVID-19 peak and almost unnoticeable level for the second peak. The rapid spread of an emerging and threatening disease led to stringent age-independent restrictions at the beginning of the pandemic. This, plus the lack of COVID-19 transmission knowledge, induced fears of mobilization and social exposure, with a significant reduction in health services attendance in all social groups. However, healthcare centers adapted as the pandemic progressed, optimizing services supply and biosecurity measures. Simultaneously, a patient learning curve is perceived regarding self-care and understanding the deleterious effects of interrupting cancer care.
The 2021 trends show an increased or stable demand for most oncology services (Table 1). These results and the observed trends during 2020 may imply that early projections tend to be overly negative due to failure to include post-confinement real-life data, an assertion supported by other studies with partially extended observational periods 9. However, the increase could also be related with a backlog of oncology services, as previously noted. Therefore, a proper response to the pandemic challenge would require a more accurate analysis of the differential impacts by cancer type, treatment type, and population groups. It is imperative for settings with limited resources to make a wake-up call for governments and stakeholders to act on the forthcoming changes in oncology service demand, ensuring economic protection and a suitable supply.











 text in
text in 



