Introduction
The health crisis caused by the COVID-19 pandemic has affected various countries, with more than 194 million confirmed cases and more than four million deaths at the beginning of July 2021. To date, Colombia is among the ten most affected countries, with more than 4 million confirmed cases and more than 119,000 deaths. Mental health disorders and problems negatively affect the quality of life, and alarming risks have been observed in Colombia, as evidenced by the National Mental Health Survey (MINSALUD, 2015), and at the present time, mental health care systems are deficient in the country (Rojas-Bernal et al., 2018). In this context, it is necessary to evaluate the impact of COVID-19 and design intervention strategies according to the population's needs (Qiu et al., 2020).
There is consensus on the negative impact of the COVID-19 pandemic on mental health. It has caused increase in depression, anxiety, post-traumatic stress, and a decline in sleep quality (Cao et al., 2020; Liu et al., 2020; Mazza et al., 2020; Wang et al., 2020). An increase in alcohol intake and tobacco uses and a decline in sports activities have also been reported (Stanton et al., 2020). Likewise, a reduced perception of happiness and satisfaction with life, which are positive indicators of mental health, has been observed (Li et al., 2020; Satici et al., 2021; Zhang et al., 2020).
Anxiety, depression, and stress in young people during the pandemic
Evidence suggests that anxiety, depression, and stress are common symptoms and reactions associated with the COVID-19 pandemic (Rajkumar, 2020). In general terms, a greater impact on anxiety, depression, and stress has been observed in women and people with chronic conditions (Mazza et al., 2020). Healthcare personnel, women, and young people have been identified as high-risk groups (Huang & Zhao, 2020; Lai et al., 2020). A high need for mental health care in the general population has been observed during the pandemic. In specific terms, a study in India on anxiety with adults indicated that about 80% of the participants required attention (Roy et al., 2020).
When evaluating the psychological impact of the pandemic during the COVID-19 outbreak in Chinese adolescents aged between 12 and 18, a high prevalence of symptoms of depression (43%), anxiety (37%), and comorbidity of depression and anxiety (31%) were observed (Zhou et al., 2020). The evaluation of the prevalence of emotional symptoms in adults (47.9% between 20 and 30 years old) during the COVID-19 outbreak in Wuhan (China) showed symptoms of depression in 48.3% and lower percentages of anxiety (22.6%) and comorbidity of depression and anxiety (19.4%) (Gao et al., 2020). In Spain, at the beginning of lockdown, university students (n = 2530) reported moderate to extremely severe symptoms of anxiety (21.34%), depression (34.19%), and stress (28.14%) (Odriozola-González et al., 2020).
Available evidence shows that during the pandemic, the women present more psychological and emotional problems; for example, they present more affectation in depression, anxiety, and stress (García-Fernández et al., 2021; Solomou & Constantinidou, 2020). A study assessing gender differences in mental health outcomes during quarantine in 59 countries found that women tended to develop more symptoms consistent with several mental disorders, such as depression, anxiety, and post-traumatic distress (Kolakowsky-Hayner et al., 2021). During the pandemic, women are also more affected by social factors such as job loss and additional concerns related to pregnancy and childbearing (Gausman & Langer, 2020).
In Italy, when the pandemic crisis began in March 2020, the population's mental health was evaluated in a study in which 2766 people participated. The results showed that female gender, negative affect, and detachment were associated with higher levels of depression, anxiety, and stress. The study also indicated that meeting someone who was ill was associated with higher levels of depression and stress, and medical problems were also associated with higher levels of depression and anxiety (Mazza et al., 2020).
An anxiety assessment carried out in Iranian population revealed that the level of anxiety was higher in women and in people who had sick relatives, as well as among people who followed news related to the pandemic and young people between 21 and 40 years of age (Moghanibashi-Mansourieh, 2020).
The impact of the pandemic on people with mental health problems
A longitudinal study conducted three measurements between April and May 2020 in the United States and analysed the effect of demographic, psychosocial, and behavioural factors on symptoms of depression, anxiety, and stress. The results showed that the pandemic had a moderate impact on the participants’ mental health. Those most affected were young adults and people with pre-existing health problems (Zhou et al., 2020).
A review of the literature (Guessoum et al., 2020), on the impact of the COVID-19 pandemic and lockdown in adolescents with psychiatric disorders, showed that the circumstances caused by the COVID-19 pandemic could cause an increase in depressive and anxiety disorders, increase symptoms related to grief and risk exacerbating emotional symptoms due to interruption or changes in care and management of disorders.
According to the study results by Czeisler et al. (2020) in which 5470 Americans participated, mental health conditions were disproportionately affecting specific populations such as young adults and people receiving treatment for pre-existing psychiatric conditions. Increased anxiety, depression, stress, higher levels of drug use, and serious considerations of committing suicide were observed. They found that 26% of the participants being treated for a previous diagnosis of anxiety disorders reported beginning or increasing drug use, and 23.6% stated that they had considered committing suicide in the previous 30 days. Furthermore, 25.2% of the participants being treated for a previous diagnosis of depressive disorders showed an onset or increase in drug use, and 22,1% reported considering committing suicide. A study conducted in France with university students (n = 69.054) evaluated the prevalence of self-reported mental health symptoms. Psychiatric follow-up history was identified as a risk factor for suicidal thoughts and symptoms of anxiety and stress (Wathelet et al., 2020).
The present study aimed to analyse the differences between young people with a history of mental health problems and a normative sample regarding their emotional symptoms, concerns, and satisfaction with life during lockdown for COVID-19. The objective was established considering that young people are a population at risk and that it is necessary to assess the pandemic's impact on emotional symptoms in people with pre-existing mental health problems. This information could be of interest for establishing differentiated care plans for young people with pre-existing mental health problems and justify the need to develop prevention programs when disaster events occur.
Method
Participants
The sample was obtained by convenience and availability, and 422 young people between 20 and 25 years of age participated (M = 21.89; SD = 1.67), of whom 77.3% (n = 326), were women. The community sample was made up of 298 participants (M = 22.13; SD = 1.65), of whom 73.4% (n = 212), were women. The clinical sample was made up of 133 participants (M = 21.38; SD = 1.59), of whom 85.7% (n = 114) were women. 87.2% (n = 116) of the participants in the clinical sample had diagnoses performed by health professionals, confirmed more than one year before the pandemic and lockdown onset. 8.3% (n = 11) were diagnosed between 6 months and one year before the pandemic, and 4.6% (n = 6) between three and six months beforehand. The most frequent diagnoses were anxiety disorders (8.7%; n = 42), depressive disorders (6%; n = 29), diagnosis of comorbidity of depression and anxiety (6%; n = 29), and other disorders and mental health problems (6.8%; n = 33).
Procedure
The procedures used for data collection were carried out following the guidelines of the Declaration of Helsinki (World Medical Association, 2013).
A unique web link to an online survey via the Lyme Survey platform was emailed to potential participants. The participants gave their consent before starting the self-report, which took between 25 and 30 minutes to complete. The questionnaires were applied between June 5 and August 3, 2020, during the period of lockdown in Colombia, which took place between March 25 and September 1, 2020.
Instruments
Sociodemographic conditions : The sociodemographic information included questions about age, gender, place of lockdown, education, and employment situation, and activities carried out.
Concerns: The researchers designed a 10-question scale on concerns about death, illness, financial situation, mental health, and interpersonal relationships. The answer options were never (1), rarely (2), sometimes (3), frequently (4), and almost always (5). The reliability analysis of all the items showed an adequate Cronbach's Alpha (α = .82).
Mental health status: A questionnaire of 26 questions was designed to inquire about the participants’ state of mental health. Questions included “Do you have, or have you had any psychological problems prior to lockdown? If so, indicate which one and since when.” Other questions inquired about the ability to concentrate, bodily sensations, and the ability to move, sleeping habits, and drug use. The answer options were never (0), much less than before (1), less than before (2), same as before (3), more than before (4), and much more than before (5).
Emotional symptoms: The Colombian adaptation of the Depression, Anxiety and Stress Scale (DASS-21) was used (Ruiz et al., 2017). This instrument is made up of 21 items, which in turn make up three subscales, and describe negative emotional states that are evaluated on a 4-point Likert-type scale (3 = "it has happened to me a lot or most of the time"; 0 = "It has not happened to me at all"). In this research, the instrument showed adequate reliability for depression (α = 90), anxiety (α = .81), stress (α = .86) and in the total scale (α =. 94).
Positive and negative emotion and feelings: An 11-item scale ad hoc was used to assess emotions and feelings with five response alternatives: much less than before (1), less than before (2), same as before (3), more than before (4), and much more than before (5). The positive emotions and feelings subscale comprise four items (4) and includes statements such as: "during the lockdown, I was satisfied with myself." The subscale for negative emotions and feelings (7 items) includes statements such as "during the lockdown, I felt angry" and "during the lockdown, I felt stressed". The positive emotions and feelings subscale showed high reliability (α = .82), and the negative emotions and feelings subscale also showed high reliability (α = 86).
Satisfaction with life: was assessed with the Colombian version of the SWLS Satisfaction with Life scale (Vinaccia Alpi et al., 2019), a five-element questionnaire with a Likert scale of 7 response alternatives, ranging from "strongly disagree (1)" to "strongly agree (7)", with scores between 5 and 35, and which enables evaluation of the individual's general satisfaction with their life. In this study, the reliability of the scale was high (α = .88).
Data analysis
Data were descriptively analysed using frequencies, means, and standard deviations. Comparisons were made for the concerns and general aspects of mental health in lockdown between the clinical and community samples using Mann-Whitney U tests for independent samples, because the Kolmogorov-Smirnov tests indicated a lack of normality in the variables.
Analysis of variance (ANOVA) was performed to establish the differences between young people without any pre-existing conditions and those who reported a diagnosis of depression, anxiety, comorbidity of depression and anxiety, and other diagnoses, in measurements of emotional symptoms, positive and negative emotions and satisfaction with life. Bonferroni post hoc analysis was used to identify the groups in which differences occurred.
Results
Descriptive results
Both the clinical and community samples were made up mostly of women, who accounted for 77.3% of the participants. 67.1% were aged between 20 and 22 years old. 98.1% were Colombian, 16.6% study and work, 24.4% experienced lockdown in closed places with no access to green areas (n = 103), and 89% (n = 376) were with their parents and other relatives.
The sociodemographic variables and some conditions associated with the lockdown experience are described in Table 1.
Table 1 Demographic characteristics of participants, for clinical and community samples.

Note: 3.5% (n = 10) of the community sample participants and 5.3% (n = 7) of those in the clinical sample experienced deaths of relatives due to coronavirus. 17.6% (n = 51) of the community sample and 35.5% (n = 47) of the clinical sample had physical illnesses, mostly allergies, and respiratory problems. 0.7% of the participants (n = 3) had coronavirus at the study time. 1.9% suspected they had it (n = 8)
Conditions associated with mental health before and during lockdown
To establish whether there were significant differences in general aspects of mental health status and during lockdown, a comparison of the mean of the responses was performed using Mann Whitney U tests. In the total sample it was observed that women, compared to men, presented more symptoms of depression (Z = -2.893, p =.004, d= .31), anxiety (Z = -2.717, p =.007, d= .34), stress (Z = -3.413, p =<.001, d= .39) and negative emotions and feelings (Z = -4.706, p =<.001, d= 1.16).
Participants with a history of mental health problems during lockdown perceived the passage of time as slower (Z = -2.074, p = .038, d = .10); they felt more inhibited (Z = -3.605, p =<.001, d= .30); experienced greater difficulty in retaining information (Z = -5.442, p =<.001, d = .50); had less restful sleep (Z = -4.058, p =<.001, d = .39), had more nightmares (Z = -1.955, p = .05, d = .21), and enjoyed less physical activity (Z = -2.381, p = .017, d = .27). No differences were observed in the two groups as regards alertness, eating habits, use of medications, consumption of alcohol, cigarettes, and drug use.
It was noted that 56.1% (n = 162) of the participants in the community sample and 66.9% (n = 89) of the clinical sample were less able to concentrate; 13.5% (n = 39) of the community sample presented fewer problems with retaining information than the clinical sample 58.9% (n = 78). 44.3% (n = 134) of the community sample and 66.2% (n = 88) of the clinical sample showed more difficulties sleeping during lockdown, and 30.8% (n = 89) of the participants in the community sample and 18% (n = 53) in the clinical sample had more nightmares.
As for sports, 38.1% (n = 110) and 48.1% (n = 64) of the community and clinical sample participants reduced their sports activities. On the other hand, the consumption of alcohol, cigarettes, and other substances increased in both groups, by 49.8% (n = 144) in the community sample and 55.6% (n = 74) in the clinical sample.
Differences in concerns associated with lockdown and the pandemic
When comparing the participants' concerns, no differences were observed for concern about one's own death and illness or that of a family member, access to health care and services, economic problems, or the supply of items to meet basic needs.
The factors that most affected the clinical sample included concern about being subject to lockdown (Z = -4.033, p =<.001, d= .41); not knowing how life will change because of COVID-19 (Z = -4.097, p =<.001, d = .41); psychological difficulties (states of anxiety, insomnia, irritability, sadness, etc.) (Z = 7.034, p =<.001, d = .79); an overload of school or work tasks (Z = 3.927, p =<.001, d = .40); concern about difficulties with cohabitation (Z = -3.962, p =<.001, d = .42); spending too much time on social networks, the internet or video games (Z = -2.670, p = .008, d = .28) and concern about academic and work performance (Z = -3.315, p =<.001, d = .36).
Differences between the two samples in emotional symptoms, emotions, and satisfaction with life
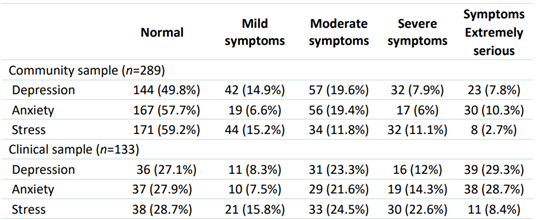
The participants were evaluated and categorized for depression, anxiety, and stress, according to the cut-off scores established for the population in the DASS-21 (Ruiz et al., 2017). The classification levels were normal, mild, moderate, severe, or extremely severe (Table 2). As can be seen, moderate to extremely severe symptoms occurred for depression in 35.3% of the community sample participants and in 64.3% of the clinical sample. For anxiety, moderate to extremely severe symptoms occurred in 35.5% of the community sample participants and 64.6% of the clinical sample. As for stress, moderate to extremely severe symptoms were observed in 25.6% of the community sample participants, while in the clinical sample, it reached 55.5%.
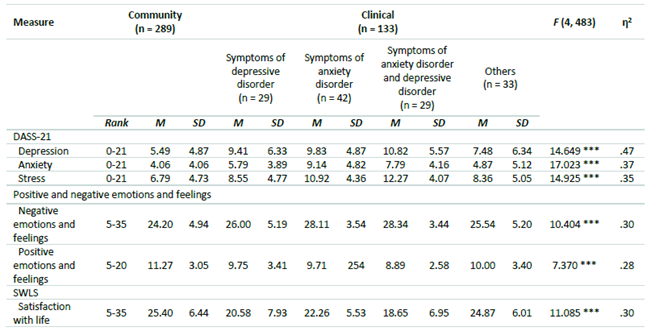
An analysis of variance (ANOVA) was performed comparing five groups: the community sample, the group with symptoms of anxiety disorders, depressive disorders, comorbidity of depression and anxiety disorders, and other mental health problems, and showed significant differences between the groups (Table 3).
The Bonferroni post hoc analysis were carried out taking the group from the community sample as a reference and indicated that the differences in symptoms of depression are more significant between the young people in the community sample and those with a diagnosis of comorbidity of anxiety and depression (μ1 - μ2= -5.33), p= <.001, 95% CI [-8.16, -.2.49]. Differences in symptoms of depression were also observed between the community group and the group with symptoms of depression (μ1 - μ2= -3.91), p=.001, 95% CI [-6.75, -.1.08], and with the group with anxiety symptoms (μ1 - μ2= -4.33), p= <.001, 95% CI [-6.74, -1.93].
Differences in anxiety symptoms were observed between the community group and the group with anxiety symptoms (μ1 - μ2 = -5.08), p =<.001, 95% CI [-7.05, -3.10] as well as with the anxiety and depression comorbidity group (μ1 - μ2 = -3.73), p = <.001, 95% CI [-6.05, -1.40].
The differences for stress are between in the same groups, i.e., the community group and the anxiety and depression comorbidity group (μ1 - μ2= -5.48), p=<.001, 95% CI [-8.05, -.2.90] and the anxiety group (μ1 - μ2= -4.13), p=<.001, 95% CI [-6.31, -1.94]. Negative emotions and feelings present a greater difference in the community sample and the clinical sample with anxiety and depression (μ1 - μ2= -4.14), p=<.001, 95% CI [-6.76, -1.51]. For positive emotions and feelings, the differences have a greater magnitude between the community sample and the group with comorbidity of anxiety and depression (μ1 - μ2= 2.37), p=<.001, 95% CI [0.71, 4.04].
In the satisfaction with life, the differences were observed between the community group and the group with anxiety (μ1 - μ2 = 3.14), p=. <05, 95% CI [0.12, 6.16], the depression group (μ1 - μ2= 4.81), p=<.001, 95% CI [1.25, 8.38], and the group with comorbidity of anxiety and depression (μ1 - μ2= 6.74), p=<.001, 95% CI [3.18, 10.31]. The post hoc results indicate that young people with diagnoses with comorbidity of anxiety and depression are those who experience the greatest discomfort during the period of lockdown.
Discussion
This study aimed to analyse the differences in emotional symptoms, concerns, and satisfaction with life during lockdown for COVID-19 between young people with a history of mental health problems and a community sample. The study hypothesis stated that there are statistically significant differences between young people with a history of mental health problems and young people without pre-existing conditions regarding their concerns about the pandemic, symptoms of depression, anxiety, stress, emotions, negative and positive feelings, and satisfaction with life. The results are in line with the hypothesis raised.
While the moderate and extreme symptoms for depression, anxiety, and stress showed percentages between 25% and 35% in young people without pre-existing conditions, the prevalence was between 55% and 65% for young people in the clinical sample. Statistically, significant differences were observed through comparative analysis of all factors, and primarily in symptoms of anxiety, depression, and stress. The differences had a greater magnitude between young people without pre-existing conditions and those presenting diagnoses of comorbidity with symptoms of stress and anxiety. Both the young people in the clinical sample and in the community, sample showed impairment in mental health, which shows the negative effect of the health crisis on the population (Rajkumar, 2020) and the need for care at all levels and social groups (Roy et al., 2020). However, young people with comorbid mental health symptoms are a population at higher risk. These observations on the risk status of people with pre-existing disorders and mental health problems were reported by Guessoum et al. (2020), who observed a greater risk of a poorer state of health and exacerbating symptoms interruptions or changes in care and management of disorders. These risks must be considered to mitigate the level of suffering and personal discomfort, and because of the risk of increased drug use, the impact of vital processes such as sleep, and the risk of suicidal ideations (Czeisler et al., 2020; Wathelet et al., 2020).
The concerns derived from the health crisis seem to affect all participants, and as such, we did not observe any differences in concern about their own death and illness or that of a family member, financial problems, and attention to basic needs. However, there were differences in concern about lockdown, coexistence problems, and psychological state (anxiety, insomnia, irritability, and sadness), work, and academic performance. This seems to indicate that the variables related to new situations generated by the health crisis affected young people with a history of mental health problems and those without pre-existing conditions in a similar way. Furthermore, we observed that having pre-existing conditions increases the likelihood of experiencing greater difficulties in daily situations, routines, and activities. As in other studies (Stanton et al., 2020), we observed increased alcohol intake and tobacco use and reduced sports activities in both cohorts. This shows that the pandemic and lockdown affect key factors for prevention in both physical and mental health. For this reason, prevention, and care programs to reverse the negative effects of alcohol intake, drug use, and physical inactivity must be encouraged.
Differences were also observed between the groups for satisfaction with life, negative and positive emotions, and feelings. One of the many negative effects on mental health caused by the pandemic is the reduced perception of happiness and satisfaction with life, which are positive indicators mental health indicators (Li et al., 2020; Satici et al., 2021). This study observed that young people with pre-existing antecedents and conditions are also the most affected. Previous studies indicate that the negative impact and greater dissatisfaction are in areas with the highest contagion rates and when individuals have existing chronic health problems (Zhang et al., 2020). We suggest strengthening socio-emotional competencies could contribute to reduce negative emotions and promote strategies that favour life satisfaction.
This study provides information that could be of interest for the prevention and intervention of young people with pre-existing mental health conditions and those without a previous condition. The results indicate the importance of designing intervention strategies according to the needs of the population, and of implementing programs that mitigate the negative effects on mental health associated with the pandemic, including drug use and the lack of physical activity. It also confirms the need to provide priority care for people with pre-existing mental health problems to prevent the exacerbation of symptoms and deterioration in health due to care problems and to reduce serious risks, including suicidal ideation (Czeisler et al., 2020).
Among the limitations of this study is its use of a cross-sectional study. Information on mental health status was self-reported and may be inaccurate. The reliability of the information would be greater with longitudinal data. The participants may not be representative of Colombian youth, the results may not be generalized to clinical samples with severe disorders, rural youth, and with less favourable socioeconomic conditions than those presented by the participants. Another limitation of this study is that women are overrepresented in the sample (77.3%), which may generate biases in the results. However, it is important to note that the results by gender observed are congruent with other studies showing that during the pandemic, women, compared to men, present more symptoms of depression, anxiety, and stress (García-Fernández et al., 2021; Kolakowsky-Hayner et al., 2021; Solomou & Constantinidou, 2020). The data obtained are relevant due to the novel nature of the problem and the need for prevention and intervention in risk groups. Future research with larger and more evenly distributed samples is required to understand the differential impacts of population subgroups from an inclusive, diverse, and equitable perspective.
Conclusion
Young people have been seriously affected by the COVID-19 pandemic in academic, occupational, social, and mental health spheres. Their prevention, care, and intervention need in Colombia are not appropriately satisfied, and differentiation, equity, and inclusion are required in health services. Those responsible for public policies and attention to the health crisis must design mechanisms that guarantee access to services according to the needs and
level of risk.
Some recommendations that researchers have provided to protect mental health include:
To identify vulnerable groups such as the young, the elderly, women, and medical staff.
To provide access to medical resources and the public health services system.
Establishing planning and coordination of strategies at the national level for psychological first aid during major disasters.
To create crisis prevention strategies and intervention systems that include epidemiological monitoring, detection, referral, and targeting (Qiu et al., 2020)