INTRODUCTION
Colonic lipomas are benign lesions that represent less than 4.4% of the tumors that affect this organ, being the location in transverse colon the least frequent. They can affect adults of any age, but they most often occur in people over age 50. 1
These lesions are usually asymptomatic, and colo-colonic intussusception is one of the rarest complications, which appears in direct relation to the size of the lipoma. 2-4 Establishing a diagnosis based on the symptomatology or on imaging findings is difficult, so colonoscopy is the golden standard to confirm the presence of this type of tumor. 5,4
Like other benign tumors, management depends not only on size, but also on symptoms. Most patients benefit from endoscopic resection, but surgery is required when that approach is not possible due to the morphological characteristics of the lipoma or because it is associated with complications such as bleeding, perforation or intestinal obstruction. 1-3,5
Nevertheless, the literature 6 does not have sufficient reports about the best surgical approach to this pathology. In this regard, this article contributes to the literature with the description of a clinical case of proximal intussusception of the transverse colon, secondary to a lipomatous lesion located in the hepatic flexure of the colon, which required surgical management by laparoscopy, without early or late post-operative complications. It also presents a brief review of the literature detailing the clinical features and management options of this unusual pathology; this part shows the contribution of the case to the reviewed literature. Finally, it is concluded that colonic intussusception is a preoperative complication that requires determining surgical management since it is diagnosed, regardless of mortality rates.
CASE PRESENTATION
A 43-year-old female patient, Caucasian, from Bogotá D.C. (Colombia), housewife, from a low-income household was admitted after 2 days of colicky pain mainly in the mesogastrium, associated with nausea, hyporexia and hematochezia. Two weeks prior to her consultation, the woman reported a change in stool caliber and occasional abdominal pain with characteristics similar to those already described that resolved spontaneously with the use of conventional analgesics. She had no pathological, surgical or family history and, according to the physical examination, she had vital signs within normal values and mild pain on palpation in the mesogastrium with a sensation of a mass at this level.
Diagnosis and identification of preoperative complications
Extension studies were requested, including a contrast-enhanced computed tomography (CT) scan of the abdomen. It showed a submucosal lesion that affected the transverse colon with fat density, suggesting a lipoma that probably led to a proximal intussusception of the transverse colon (Figure 1).
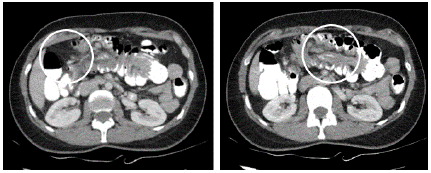
Source: Document obtained during the study.
Figure 1 CT scan of the abdomen performed on admission showing colo-colonic intussusception.
Bearing in mind that the findings of the CT scan suggested a rare pathology and the fact that the patient's clinical picture pointed to a diagnosis of right colon cancer, a colonoscopy under sedation was considered necessary. Based on the study, a rounded subepithelial mass was observed in the proximal transverse colon in what seemed to be a hepatic flexure, with smooth edges and no findings compatible with infiltration. The mass occupied 50% of the circumference, obstructed 70% of the lumen, and tilted producing intussusception (Figure 2).
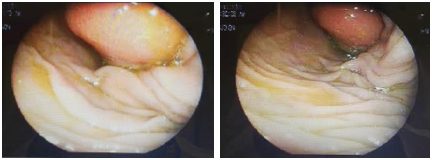
Source: Document obtained during the study.
Figure 2 Preoperative colonoscopy showing submucosal lesion in the proximal transverse colon.
Subsequently, because of the impossibility of endoscopic management due to the size of the lesion, the patient was taken to surgery, where a right hemicolectomy was performed by laparoscopy with side-to-side extracorporeal anastomosis with mechanical suture, without using drains. Mechanical bowel preparation was not considered necessary for this procedure; however, prior to surgery, prophylactic antibiotics (first-generation cephalosporin) were administered.
Intra-operative and post-operative findings
One of the intraoperative findings was a mobile pedunculated mass in the hepatic flexure of the colon, about 7x7cm, which protruded towards the lumen, without serosa involvement, causing colo-colonic intussusception (Figure 3).

Source: Document obtained during the study.
Figure 3 Lipomatous lesion observed in the surgical specimen obtained from enlarged right hemicolectomy.
In the post-operative period, the patient evolved without complications, so she was discharged on the third day with analgesic management and general recommendations.
The surgical pathology results concluded that the specimen was a submucosal lipoma with adjacent ulcerated mucosa and negative reactive changes for dysplasia and malignancy. Post-operative follow-up was carried out on the seventh day and the third week, and an adequate clinical evolution was observed, without complications related to the surgery. Consequently, coloproctology discharged the patient with nutritional recommendations and colonoscopic screening at age 50.
DISCUSSION
The case makes a significant contribution to the literature. The epidemiological, histological and clinical characterization of lipomas is presented below, including a description of colo-colonic intussusception with precise information on its incidence, clinical findings and types of intussusception. Additionally, details on what the literature has reported regarding the diagnostic approach to this type of lesions in the colon are provided, and the therapeutic approach is analyzed according to the literature.
Epidemiological, histological and clinical characterization
Lipomas of the gastrointestinal tract were first described by Bauer in 1757; later, a few other cases were reported in the literature, including the publications of Stetten (1909) and Hall (1985), who explained that these lesions could clinically resemble pathologies such as angiodysplasia and colon cancer. 7,8
Classic lipomas are histologically formed by mature adipose cells without pleomorphism, localized more frequently in the limbs and the trunk. 9 In the digestive tract, despite being somewhat rare with an overall incidence of 1.8% 1.3, mature adipose cells without pleomorphism are found in the colon for the most part, with an incidence of 0.03-4.4%, and located 65% of the time on the right side, often in the cecum. 2,6 Most of these lesions originate in the submucosal layer, but up to 10% may arise from the submucosal layer and extend to the muscle layer. 6,3
The systematic review by Crocetti et al.1, published in 2014, describes a female predilection in 55% of cases. Furthermore, the pathology is observed in an age range between 32 and 82 years (61±9), and only 15% of the total evaluated lipomas were located in the transverse colon, as in the clinical case reported in this article.
Most lipomas are asymptomatic; however, as the size of the lesion increases, the chances of developing symptoms are as high as 25%. One of the most unusual pictures that patients with lipomatous lesions >4cm may present is colo-colonic intussusception, of which only 32 cases have been reported in the literature. 1,3,6
Colo-colonic intussusception
Intussusception in adults originates 50-75% of the time in the small intestine, being usually secondary to a Meckel diverticulum or adhesions. Less than 20% of intussusception cases originate in the colon, with adenocarcinoma of the colon being the most common cause at this level. 10
In adults, this condition is generally secondary to an alteration in the normal peristaltic activity of the bowel wall, resulting from a pathological lesion that serves as the starting point for invagination from one bowel segment to another. 11
Intussusception is much more common in children, but may occur in up to 10% of adults. Studies describe a classic triad for diagnosis consisting of abdominal pain, palpable mass and hematochezia 12,13; however, publications such as Paskauskas et al.3 report that the most frequent symptoms, prior to emergency department consultation, are abdominal pain (100% of cases), followed by episodes of diarrhea and hematochezia (22-32% of cases). This pathology is usually limited to a single segment of the colon, and the least frequent is retrograde intussusception. 3
There are four main types of intussusception which are entero-enteric, ileocolic, ileocecal and colo-colic; the latter is the most common type in adults, which is consistent with the case report described here. 11
Diagnosis and findings of lipomatous lesions
The main diagnostic tools for lipomatous lesions are: 1) radiological studies, such as ultrasonography, which has many limitations inherent to the method and because it is an operator-dependent test 11; 2) computed tomography and abdominal nuclear magnetic resonance, which can determine fat density on many occasions by revealing infiltration of the colon wall, but can establish a less certain diagnosis as a malignant pathology 2; and 3) colonoscopy, which is the confirmatory method for this type of neoplasms due to their morphological characteristics. 5,4
The endoscopic findings of a lipoma include smooth, spherical, slightly yellowish and usually broad-based polyps of variable size (0.5-5cm). In addition, they show some characteristic endoscopic signs that are observed during manipulation with biopsy forceps, namely, tent sign (elevation of the mucosa over the lipoma), cushion sign (indentation of the lesion), and naked fat sign (extrusion of fat after biopsy). 4
Even so, some publications, such as Ghanem et al.8, report that biopsies taken during colonoscopies are not obtained adequately because ulcerated and necrotic tissues, distinctive of atypical lipomas, can cover adipose tissue. In such cases, the recommendation is to perform a biopsy by echoendoscopy in order to have a better diagnostic yield. 8
Therapeutic approach and association with the described case
The therapeutic options for colonic lipomas depend on the size of the mass: endoscopic resection is the first option for lesions <2cm, while surgical management is considered for larger symptomatic lesions or when they lead to complications such as intussusception. 1,2,3,6 Non-radical segmental colectomy via laparoscopy is generally the best therapeutic choice because there is less surgical trauma and a rapid post-operative recovery. 1,3,8,14
The case described here presented intussusception secondary to a pediculated lipomatous lesion of the hepatic flexure of the colon of about 7x7cm. This is a rare pathology with marked influence on both diagnosis and treatment selection. According to the reports, it can be said that determining the exact etiology of colon lesions based on clinical findings alone is difficult. Although the first differential diagnosis is colon cancer in the majority of cases, it is necessary to consider neoplasms of benign origin, despite their low incidence.
In this case, taking biopsy samples during the colonoscopy was not necessary because the size of the lesion and the symptomatology required priority surgery: laparoscopic right colectomy. Therefore, based on this report, it could be said that colonic intussusception is a preoperative complication for which surgery is the most recommendable option since it is diagnosed.
CONCLUSIONS
Colon lipomas are lesions that represent less than 4.4% of tumors affecting this organ and 1.8% of all tumors of the digestive tract. However, scientific discussion on this issue should not be disregarded only because of its low or high incidence, nor should it be forgotten that this pathology generally affects adults of any age, more often the population over 50 years of age. 1 With this in mind, knowing about cases that allow suggesting the best therapeutic approach is essential for medical practice.
The importance of this case also lies in the fact that colonic lipomas, as they are lesions considered incidental findings, can be clinically mistaken for other pathologies, mostly of malignant origin. Since both the size and macroscopic characteristics of these lesions can be determined from endoscopic imaging, colonoscopy is a diagnostic tool that avoids confusion with malignant pathologies and allows a better therapeutic approach.
In the case described here, the surgical approach was laparoscopic right colectomy, which is currently the most effective approach, the one that causes the least surgical trauma and the one that has the fastest post-operative recovery. The proper characterization and diagnostic approach of patients, as described above, avoids taking biopsies during colonoscopies and performing other procedures that are not always necessary.














