Introduction
Diabetes mellitus (DM) is currently a true epidemic. Those who suffer from it have a high risk of developing diabetic nephropathy and between 20 and 50% of them are at risk of suffering from terminal chronic renal failure (ESRD) and need dialysis or kidney transplantation1-3. It is known that about 40% of new cases of ESRD are due to this pathology. The number of diabetic patients who start dialysis is increasing all over the world and, in the province of Camagüey, it is not a different one, but it constitutes a real health problem. These patients present significant differences with respect to the rest of patients on dialysis, in terms of their demographic characteristics, complications, comorbidities and particularities in their treatment. They also need special management in most areas of hemodialysis, such as dialysis guidelines, vascular access (VA) or diabetes control; Likewise anemia, vasculopathy and retinopathy, which are usually associated with these patients4.
End-stage renal failure (ESRD), secondary to diabetic nephropathy (DN), is the most common cause of admission to renal replacement therapy (RRT) programs. The increase in affectation due to DM is related to a greater exposure to risk factors (inadequate dietary habits, sedentary lifestyle, obesity, among others) and to the increase in life expectancy. Thus, a greater number of people reach the ages in which this disease is more frequent5.
The decrease in infant mortality, communicable diseases and the general mortality rate has produced an increase in the life expectancy of the Cuban population (currently 77 years). An aging population has been created, which will produce a continuous increase in the prevalence of DM over the next 30 years, unless a greater efficacy is developed in the control of the most important risk factors (sedentary lifestyle, obesity) 6.
At the dawn of this century, the so-called "global diabetes epidemic" was unleashed, a phenomenon that is particularly related to type 2 DM and is taking place in both developed and developing countries6.
The ND rarely appears before the 10 years of evolution of DM. However, in some cases, it can occur before that time and even before the DM. Occasionally, microalbuminuria can be detected in patients with more than 12 years of evolution of the disease7. Consequently, it is estimated that the global prevalence of type 2 DM will increase, from 171 million in 2000, to a figure of at least 366 million for the year 2030. Therefore, a greater number of people will arrive to suffer from ESRD and require renal replacement therapy6,8. The so-called "micro-vascular complications" (retinopathy and nephropathy) are directly responsible for the morbidity most frequently associated with DM. In Spain, the percentage of diabetic patients with ESRD accounts for 36% of the total and the most important cause of terminal renal failure (26%) is ND9. In Germany and the USA in the US, more than 40% of people with ESRD have diabetes. At a global level, the number of patients with this pathology and who, in addition, needed dialysis was 1,000,000 in 2005, of which 260,000 resided in the USA. UU It is estimated that this population will grow at an annual rate of 8% 5,9.
Worldwide, the CTRI (Chronic Terminal Renal Insufficiency) is one of the pathologies of greatest impact, which has been located in the last 7 years within the first causes of morbidity and mortality. In Venezuela, these figures correspond to those registered in countries such as Chile, Argentina, Uruguay and Colombia10, where DM occupies the main cause, between 30 and 40%. In a study conducted in ten countries in Latin America, including Venezuela, it was determined that DN was the most frequent cause of ESRD (End Stage Renal Disease), with 24.6%11,12. According to this study, in Venezuela there are 9,408 patients on dialysis and 2,122 of them on hemodialysis (79%)10,13. "
In Cuba, there has also been a progressive increase in the number of patients with ESRD accepted in the dialysis and renal transplant (RT) programs. They have reached 10% of the total in recent years, with a propensity to increase5,13,14. In 2003, there were approximately 14,052 people with DM in the province of Santiago de Cuba. Of these, 1,054 were diagnosed as such in the same year and, in 2004, the number increased to 1,276 new patients15. According to statistics from the Nephrology Service of Camagüey, of the total number of patients included in the Chronic Program in 2012, 11% was constituted by diabetic patients, who increase the rate of deaths in the year.
If, in addition to the above, we consider that the life expectancy of the diabetic is, on average, eight years less than that of non-diabetic persons between the ages of 55 to 64 years and four years younger than those of 65 to 747, we can confirm that this condition constitutes, increasingly, an important health problem7,8. Due to the aging of the world's population, by 2025, 146 million people between 40 and 59 years old will suffer from diabetes and 147 million people aged 60 or older11. Globally, diabetes demands as many lives a year as HIV/ AIDS16-18.
In Cuba, the rate continues to be higher in women than in men (41.5% vs. 25%) and, for several years, it has been among the first ten causes of death19,20. In 2010, it caused 2,638 deaths, for a rate of 23.5 x 100,000 habs21. It is also observed a sustained growth of the prevalent patients in dialysis methods, with a rate of 119 per million population (pmp) in 2008, of 134 pmp in 2009 and 149 pmp in 2010, which means an annual increase of 10,3 %, 11,2% and 11,1% respectively22-24.
The Pan American Health Organization (PAHO) estimates that the cost of diabetes and ESRD in the region is at least 65 billion dollars per year, resulting in premature death, absenteeism, disability, medications, hospitalizations and medical consultations25-27.
The probability of developing an ESRD varies considerably based on racial and ethnic characteristics in patients with DM. It has been estimated that, in patients with type 2 diabetes of Caucasian race, it is in the range of 15 to 20%. However, the prevalence of type 2 diabetes is 10 to 15 times higher than that of type 1 DM. The result is that between 60 and 90% of diabetic patients who initiate diabetes dialysis programs have DM 2. Aging relative to the population, the increase in DM 2 and the improvement in the survival of these patients leads to a significant number of patients developing CRI, secondary to DN28.
The natural history of the DN is understood as a progressive path, from the renal functional alterations to the terminal renal failure. It goes through intermediate stages, marked by the appearance of microalbuminuria and proteinuria29. It can progress rapidly, after relatively long periods of stability, or end with early death of the patient, usually due to cardiovascular causes. The clinical course of nephropathy, in patients with type 2 DM, may present significant differences compared to that of patients with type 1 DM, in the phases prior to the development of established proteinuria. Due to a more advanced age, as well as the presence of arteriosclerosis, patients with type 2 DM may present other kidney diseases, added, more frequently than patients with type 1 DM, including diabetic nephropathy. The sum of the multisystemic damage of DM and chronic renal failure make it very difficult to treat these patients30.
The first alterations found in patients with ND are microalbuminuria and glomerular hyper-filtration, which implies a thickening of the glomerular basement membrane, tubular hypertrophy and expansion of the mesangial matrix. This is, possibly, a compensatory mechanism to prevent the urinary loss of water and electrolytes, an overload that generates glomerular damage33 and, in turn, decreases the glomerular filtration area (GFR), with progressive loss of renal function. Finally, glomerulosclerosis and terminal kidney disease are observed31,32.
The term ND is used exclusively to indicate renal lesions caused by microangiopathic or small vessel involvement33. The clinical picture is characterized by persistent proteinuria, arterial hypertension and progressive deterioration of renal function34,35. Hyperglycemia and arterial hypertension, combined, produce important clinical consequences4,12.
The ESRD is defined as the final entity to which chronic kidney diseases (CKD), primary or secondary, can arrive. Its main characteristic is the progressive and irreversible deterioration of global renal function, with a GFR level of less than 15 mL/ minute/1.73 m2 of body surface36.
Due to the failure of renal function, patients with DN are included in the Renal Replacement Therapy (RRT) program. In all patients with CKD, early remission to the nephrologist is important, as it is associated with lower mortality, better hemoglobin and albumin levels, as well as shorter hospital stay at the start of dialysis37. For diabetic patients, this fact is even more important, because it allows a better preparation and early measures can be applied to prevent the progression of renal failure. Among these, we can mention the intensification of glycemic control and blood pressure, especially if there is proteinuria, and the incidence of unhealthy lifestyle changes (excessive weight, tobacco consumption, etc.). It also facilitates the realization of an AV for a comfortable and safe dialysis start. The optimal time for the start of dialysis is still to be defined. However, at present, it is considered that the best time is when uremic manifestations or signs of malnutrition have not appeared28. In the case of diabetic patients, some authors advise that dialysis starts with higher creatinine clearances compared to non-diabetics, around 12-15 mL/min. This is due to the rapid progression of renal failure in such patients, the comorbidities they present and the difficult control of arterial hypertension when the filtrate is so low, with the consequent acceleration of hypertensive retinopathy29 and the difficult handling of sodium and water, frequently associated with the appearance of heart failure40-41.
Autonomic nervous system dysfunction and cardiac diastolic dysfunction of the diabetic patient cause a greater number of hypotension in Hemodialysis (HD). In addition, getting a good Auriculoventricular Block (AV) is difficult due to the coexistence, often, of vascular disease. Hypotension has a negative effect for the diabetic patient and can cause angina, intestinal ischemia, cerebral or lower limbs. This alarming picture is produced by:
Poor adaptation to the decrease in plasma volume of dialysis, due to autonomic dysfunction.
Presence of anemia.
Hypoalbuminemia due to malnutrition or an associated nephrotic syndrome. This fact decreases oncotic pressure, slows vascular filling and hinders the recovery of hypotension42.
In the province, there are no studies describing the behavior of the diabetic patient in hemodialysis and that they help the attending physician as an instrument to act on the morbidity and mortality of these patients and to improve their way of life. The main objective of this work was to evaluate the differential behavior of the diabetic patient in relation to the non-diabetic patient on hemodialysis at the Manuel Ascunce Domenech University Hospital, Camagüey, Cuba, in the period between August 2009 and January 2014.
Methodology
A descriptive cross-sectional cohort study was carried out. The study universe consisted of all patients with ESRD, who underwent hemodialysis at the Hospital Universitario Manuel Ascunce Domenech of the Province of Camagüey. The sample consisted of 174 patients in total (stage 3b, 4 and 5), 90 of which were selected from a simple random sample, in order to distribute homogeneously the patients with ESRD both by DN, and by other causes. In turn, those patients who met the following inclusion, exclusion and exit criteria were considered:
Inclusion criteria:
Agree with the participation in the investigation, by signing the informed consent.
Having completed eighteen years.
Exclusion criteria:
Failure to meet inclusion criteria.
Do not wish to participate in the study at any time during the investigation.
Exit criteria:
Change HD center during the study.
Have peritoneal dialysis as a renal replacement method, or go from hemodialysis to peritoneal dialysis at some point in the study.
Receive a kidney transplant (KT) during the study period.
Death during the investigation process. Obtaining the information
The primary data for the investigation was obtained from the Nephrology Service database. The primary source for obtaining the information was the survey, made according to criteria of objectives. The secondary source was formed by the clinical histories and the banners of the hemodialysis patients. The following variables were considered in the survey:
Age group
Time in hemodialysis
Comorbidity
Nutritional status
Type of vascular access
Attempt of vascular accesses
Complications in hemodialysis
Causes of kidney transplant disability
Statistical processing
A data file was prepared with the use of the SPSS Statistical Program package version 15, prior to processing them and obtaining the results. The information obtained was processed on a computer with Windows XP system installation. The methods used were descriptive statistics and frequency distribution (p <0.05). The results obtained were presented in tables and graphs designed for that purpose, in which the information was summarized, in order to address each specific objective. Subsequently, each result obtained was analyzed and then, through the process of synthesis and generalization, conclusions were drawn up.
Semantic control
Vascular access: in hemodialysis, there are three primary modes of access to blood: the intravenous catheter, the internal arteriovenous fistula of Cimino-Brescia (AV) and the synthetic graft. The type of access is influenced by factors such as the expected course of a patient's renal failure time and the condition of their vascularity. Patients may have multiple accesses in a given time, sinceusually a catheter must be used temporarily to perform dialysis, while the permanent access, fistula or arteriovenous graft is maturing43.
Arterial steal syndrome: it is a rare complication of AV required in HD, which normally occurs within thirty days after surgery. It disappears or improves in a few weeks. It manifests with coldness, numbness of the fingers, pain and paleness in the hand and Paresthesias. In extreme cases, it leads to ulcers and gangrene. It is produced by the decrease in arterial flow in the distal part of the limb, as part of the blood supply is diverted to the arteriovenous fistula or prosthetic graft, since this offer less resistance to the passage of blood. It produces ischemia in tissues44,45.
Invalidity for kidney transplantation: are those contraindications, absolute and relative, that make renal transplantation (RT) impossible. The side effects associated with immunosuppression lead to an increased cardiovascular risk, already high in these patients, of infections and neoplastic processes46.
Ethical aspects and field procedure
The research was conducted in accordance with ethical principles for biomedical research in humans. Accordingly, the informed consent of the patients was requested; the objectives of the investigation were explained to them; they were asked to collaborate, under the commitment to use the information only in the context of the study, and they were informed that they were free to refuse, if they so wished.
Results and Discussion
Diabetic nephropathy (DN) is the main chronic complication of type 2 DM, a disease of high social and economic cost and the main cause of admission to dialysis treatment throughout the world. There is a 21% risk of developing DN in type 2 DM in the first twenty years of the disease's evolution. When clinically evident, the average survival is seven years for both sexes and, if the creatinine levels exceed the figure of 176 mmol/l2, two years47.
These patients present significant differences with the rest of patients on dialysis, in terms of demographic characteristics, complications, comorbidities and treatment objectives. All of them are in advanced stages of terminal chronic renal failure (ESRD), that is, in stages 3b and above. They need special management in most areas of hemodialysis (HD), such as dialysis patterns, VA or the control of diabetes, anemia, vasculopathy and retinopathy, diseases that are usually associated with these patients47,48.
Table 2 shows the distribution of patients studied according to age group (all in stage 3b, 4 and 5). Patients with 60 years of age or older predominate, who constitute 54.45% of the cases and, of these, 31.12% are diabetic. The same trend was observed with respect to the investment of the population pyramid in Spain, which has been the result of an improvement in life expectancy and stands at 80,2 years, according to data from the year 2013. Consequently, the incidence of CKD Terminal is much higher in elderly patients than in the general population and, among those who start renal replacement therapy (RRT), it is three times higher than the average in the group older than 75 years31.
Table. 2 Differential characteristic of the diabetic patient in relation to the non-diabetic in hemodialysis Distribution of patients according to age group and sexes (all in stage 3b and more) Nephrology Service. Hospital Universitario Manuel Ascunce Domenech, 2009-2014.
In some autonomous communities, the number of patients older than 80 years with terminal CKD has multiplied tenfold in the last ten years33. It is necessary to consider that the decrease in glomerular filtration rate (GFR), in relation to age, cannot be explained solely by an involutive process, since it is possible to find a population with advanced age and a normal GFR. Lindeman et al. and Rowe et al., in classic prospective studies, show a progressive decrease in GFR, estimated at 1.09 ml/min/year. However, in one third of the individuals in the sample this does not occur; but, on the contrary, in a small group, it does increase. These data, in addition, coincide with those of other authors49-51.
Certainly, the clinical course of CKD in elderly patients is poorly understood. When the mortality risk in the elderly population is stratified, it is found that the relative risk, although high, is lower than in younger populations and attenuation is observed, depending on the relationship between decreased GFR and mortality. Although mortality rates and ESRD are inversely related to GFR for all ages, among patients with comparable GFR, the elderly have a higher risk of mortality and a lower risk of developing ESRD than the younger ones. The relationship between age, progression of kidney disease and GFR is complex. Among those patients with GFR <45 ml/min/1.73m2, those with a decrease greater than 3 ml/min/1.73 m2 are younger and, on the contrary, in those with FG> 45 ml/ min/1.73 m2, the same decrease in FG corresponds to the elderly52. Consequently, and admitting that longevity is the result of an improvement in health and that advanced CKD depends more on comorbidities than on age per se, the prevalence of CKD may not have the expected increase.
Table 2 also shows the distribution of patients according to sex. Could be seen a predominance of male sex, represented by 63.33% of those studied. In demographic studies conducted in Colombia, it was found, coincidentally, that 74.3% belonged to males and 25.7% to females51.
Figure 1 shows the relationship of the patients studied according to time in hemodialysis (HD). A greater number of patients can be seen receiving said treatment in a period between six months and one year (37.76%), with significant differences between the non-diabetic and diabetic population. Overall, it shows lower survival once the dialysis treatment is established, given by a greater comorbidity in this group with the appearance of cardiovascular disorders, such as arrhythmias and acute coronary syndrome.
The latter, even, can attend silently52,53. Also, infectious complications related or not to the atrioventricular block(AV), are manifested to a greater extent, especially when it is an intravascular catheter.
Despite the substantial improvement experienced in all forms of CKD replacement therapy, patients on dialysis continue to suffer significant morbidity and mortality and reduced quality of life54. Their chances of survival are ten to twenty times lower than those of the general population. In patients with CKD secondary to DM, annual mortality increases 40% more. Cardiovascular disease is the leading cause of death in patients on dialysis treatment. More than 50% of patients on dialysis have three or more conditions of comorbidity, the number of days of hospitalization is greater than fifteen, per patient and year, and the quality of life referred to by them is much lower than that required by the population general. Patients undergoing renal replacement therapy, despite advances in their follow-up and treatment, have the worst rates of survival, morbidity, mortality and quality of life, due to their higher comorbidity since they suffer, more frequently, heart failure, ischemic heart disease, peripheral vasculopathy and chronic liver disease. Patients with DM also present a worse functional situation and a worse perception of their health.
In the case of diabetic patients, some authors advise that dialysis starts with higher creatinine clearances, between 12 and 15 mL/min55,56. This is due to the rapid progression of renal failure in such patients, the comorbidities they present and the difficult control of arterial hypertension when the filtrate is so low, with the consequent acceleration of hypertensive retinopathy and the difficult handling of sodium and water, associated, very frequently, with the appearance of heart failure57,58.
Figure 2 refers to comorbidity in patients. A predominance of hypertension, ischemic heart disease and liver disease could be seen in the case of the diabetic population (88.88%, 64.44% and 55.55%, respectively).
Autonomic nervous system dysfunction and cardiac diastolic dysfunction in diabetic patients cause a greater number of hypotension in hemodialysis than in peritoneal dialysis. These episodes of hypotension can have very negative effects in diabetic patients and cause angina, or intestinal, cerebral or lower limb ischemia. At the same time, these hypotensions cause the dialysis time to be shortened and, therefore, the patient to be "infradialized" and to accumulate more fluid and more uremic toxins59.
The presence of peripheral vasculopathy affects between 20 and 40% of diabetic patients on dialysis. Its presence causes great morbidity and mortality, since, in many cases, it is associated with ischemic heart disease and may require multiple interventions, such as bypass, angioplasty or lower limb amputation. A recently published study, conducted with 29,838 dialysis patients, concluded that there was a high prevalence (6%) and a high incidence (2 events/100 patients-year at risk) of lower limb amputations among dialysis patients and that this risk was multiplied by nine in diabetic patients60-62. The classic factors that were associated with the amputations were age, peripheral vascular disease and tobacco. The longest time in dialysis and the alteration of bone and mineral metabolism was associated with specific dialysis factors. In diabetic patients, being male, smoking and having other chronic complications of diabetes, as well as the presence of anemia or malnutrition, were associated with an increased risk of lower limb amputations60,61.
Measures can be adopted to avoid intradialytic hypotension in diabetic patients and thus improve tolerance to this procedure. These are, among others, to carefully evaluate the dry weight (weight that the patient must have when finishing the dialysis, once the excess of liquid of the body is eliminated, with good tolerance on the part of the patient and without producing hypotension), motivate the patient not to have excessive interdialysis weight gains, avoid aggressive ultrafiltration, increase the number of sessions or its duration, avoid taking antihypertensive drugs before dialysis, maintain adequate control of anemia and nutrition and use profiles of sodium in the dialysis bath to better manage the volume62-64.
In Figure 3, in relation to the patients studied according to the Nutritional Status, a greater number of lightweight overweight cases (11.12%) was observed in the diabetic population (ESRD with ND), followed by patients with low weight (10%). of this population). Some cases of obesity are notable.
Many studies have shown that diabetic patients on dialysis have a higher prevalence of malnutrition, especially type 2 diabetic patients, with loss of somatic protein (reflected in a decrease in plasma creatinine) and visceral protein (detected by a decrease in albumin and pre-albumin). Therefore, despite the restrictions of dialysis and diabetes, it is necessary to provide these patients with an adequate caloric intake, with diets that avoid malnutrition: 25-30 kcal/kg/day, 50% complex carbohydrates. The protein content will be 1.3-1.5 g/kg/day. On the other hand, diabetic gastroparesis can cause an erratic absorption of food, producing episodes of both hyperglycemia and hypoglycemia. Therefore, to improve symptoms, these patients are recommended to eat food in small quantities and several times a day63-65.
Figure 4a refers to the distribution of patients studied according to type of VA. A greater number of diabetic patients are shown with double lumen intravascular catheter (17.76%), in relation to the prevalence of patients with arteriovenous fistula in non-diabetics (20.00%).
Figure 4 Relationship of patients studied according to a) type of vascular access and b) vascular access attempts.
Regarding the distribution of patients according to the number of attempts at permanent VA (Figure 4b), it shows that 24.45% of diabetic patients had between six and ten attempts and 17.76%, more than 10 attempts. These figures are higher than those of non-diabetics.
Performing arteriovenous (AV) block for hemodialysis is, in many cases, a problem. Diabetic patients have a higher incidence of arteriopathy, with greater calcification of the distal arteries of the wrist (radiocephalic) and with better preservation of the proximal arteries (humerocephalic) 65. In addition, they have a worse venous system, favored in part by the large number of blood extractions and intravenous treatments that have had to endure. Numerous publications highlight that diabetic patients have a higher rate of complications in arteriovenous fistulas (AVF), such as dysfunction, thrombosis or theft (consisting of the appearance of pain in the hand, with coldness and, occasionally, lividity, which worsens during dialysis, due to insufficient arterial blood flow to the distal area). These circumstances force the nephrologist and the vascular surgeon to consider what would be the best vascular access for hemodialysis in these patients. In general, it is recommended that, in patients in whom there is no contraindication, after a brief evaluation, a radio-cephalic arteriovenous fistula (AVF) should be performed, taking into account its shorter duration. As a second alternative, the creation of an arteriovenous fistula (AVF) humerocephalic is proposed. As a last option, because it presents more complications, the creation of a prosthetic fistula or the placement of a central venous catheter is contemplated63-65.
In many patients, VA is complicated due to insufficient arterial flow, as a consequence of arteriosclerosis and poor venous status that many patients with DM have. This problem is much more pronounced in patients who did not consult in a timely manner the nephrologist, since this delay prevents proper planning of vascular access and imposes the need to place temporary catheters that may compromise the future of permanent VAs. The survival of systemic vascular grafts in diabetic patients is lower than in non-diabetic patients65.
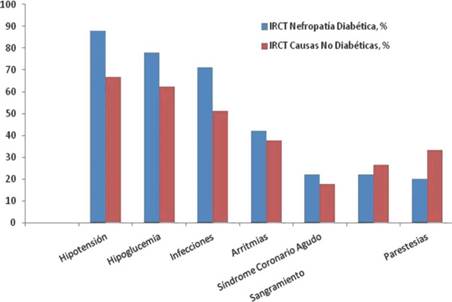
In relation to the patients studied, according to complications associated with HD (Figure 5), it could be seen that the hypotension, hypoglycemia and infections predominated in the diabetic population (88.00%, 78.00% and 71.11%, respectively). In non-diabetics, hypotension and infections occurred more frequently.
Among the main causes of hypotension, in diabetic patients who are undergoing hemodialysis, we have the worst adaptation to the decrease in plasma volume of dialysis, due to autonomic dysfunction, the presence of anemia, hypoalbuminemia due to malnutrition, or an associated nephrotic syndrome. This fact decreases the oncotic pressure, slows vascular filling and hinders the recovery of hypotension64,65.
Regarding blood glucose control in these patients, the current recommendations of the American Diabetes Association indicate to maintain a metabolic control with glycosylated hemoglobin (HbA1c) below 7%, in order to reduce micro-vascular complications. But HbA1c is accepted above 7% in patients with a history of severe hypoglycemia, a shorter life expectancy, associated comorbidities and important micro-vascular or macro-vascular complications, such as the evolved ND. The studies available in this regard, in diabetic patients on dialysis, offer contradictory results. While some show worse survival associated with worse glycemic control, others find no correlation in this regard. On the other hand, there are several studies that indicate that the uremic states of these patients can, by itself, increase the formation of HbA1c and that the use of erythropoietin can also affect erythropoiesis and the formation of HbA1c. Therefore, recently, the use of a correction factor to calculate HbA1c has been suggested based on the doses of erythropoietin and on the state of anemia. Despite these limitations, HbA1c continues to be considered the best index for the control of diabetes, even in patients with terminal chronic disease63.
There is a new concept called "diabetes burned" or diabetes burnt-out. It consists of an alteration of the homeostasis of blood glucose, which occurs in patients with end-stage renal disease. This phenomenon results in the decrease of insulin needs, with spontaneous hypoglycemia, in patients with advanced diabetes. There are several factors that could explain these alterations: the decrease in GFR, which reduces the clearance of insulin and increases its half-life; the reduction of hepatic clearance of insulin by uremic toxins; the decrease in renal gluconeogenesis; the loss of weight and muscle mass and dietary restrictions, among others. Although the practical significance of the syndrome of burned diabetes is not clearly demonstrated, some authors believe that patients who suffer from it have a worse prognosis and higher mortality than those diabetics who remain hyperglycemic on dialysis64.
Regarding the treatment of diabetes in patients on dialysis, insulin requirements decrease as renal function deteriorates, so that their adjustment must be done progressively and individually for each patient. The majority of oral antidiabetics are eliminated by the urinary tract, which is why they are contraindicated when renal function decreases.
There are no studies of these drugs in patients on dialysis and, although repaglinide can be used in cases with very low GFR, there are no studies in patients on dialysis. Some trials with a small number of patients have shown that inhibitors of dipeptidylpeptidase IV, such as vildagliptin, can be used in patients on dialysis, although at a lower dose than in the normal population65.
Finally, regarding the distribution of patients according to the main causes of disability for RT, it was possible to see how, in both groups, the number of patients unfit for kidney graft due to cardiovascular disease, extreme ages and active infection was higher. A greater number of diabetics with cardiovascular diseases and infections were found (66.67% and 48.89%, respectively).
In patients with DM and ESRD, the transplant options are kidney and pancreas, or isolated kidney. The choice of one transplant or another will depend on the age and type of diabetes of the patient, although it will always be essential to conduct a thorough study to determine the advantages and disadvantages of each type of transplant for the recipient. Isolated TR involves a marked improvement in the quality of life of the recipient, but does not influence metabolic control or prevent the chronic complications associated with diabetes. The simultaneous transplantation of pancreas and kidney is a more complex procedure, with greater surgical risk and greater morbidity in the post-transplant period. However, it has some benefits: insulin independence is achieved, the recurrence of diabetic nephropathy on the transplanted kidney is avoided, secondary complications are stabilized or improved, and control of cardiovascular risk factors is improved, with the consequent decrease in long-term morbidity and mortality63-65.
Initially, only patients with an age lower than 45 years were accepted for TR pancreas. Later, with the improvement of the results, this limit was extended to 50 years, which, in general, is still maintained at present. In older patients, an isolated kidney transplant is recommended. However, it is well known that chronological age does not always coincide with biological age, since a young patient may have developed more serious complications than older patients, which condition a worse prognosis. Thus, on occasion, pancreatic TR can be contraindicated in a young patient, but indicated in another older patient, which makes individual assessment essential65.
Other parameters that must be assessed before indicating the type of transplant are: the state of diabetic complications and the presence and severity of these complications at the time the patient is studied for transplantation. Severe vasculopathy is the complication that can most determine the decision. Occasionally, contraindications for replacement therapy (TR) in the pancreas or isolated replacement therapy (TR) may be the same from the point of view of cardiovascular disease.
The implantation of two organs requires a more complex surgery and a longer anesthesia time and implies a greater probability of presenting some type of complication, or needing a surgical reoperation. On the other hand, the presence of severe calcifications in the iliac vessels, where the vascular anastomoses of the organs are usually performed, as well as the existence of a severe peripheral vascular disease, can allow, from the technical point of view, the implantation of a graft. , but making the implementation of the two inadvisable. In these cases, the TR is always given priority.
Conclusions
It was observed that, in the case of patients with terminal chronic renal failure due to diabetic nephropathy, those over 60 years of age, male and with a stay of six months to a year in the hemodialysis plan, predominated. The comorbidity found was mainly arterial hypertension, ischemic heart disease and Hepatopathies, in that order, in both groups.
Chronic renal patients with diabetic nephropathy were distributed between underweight and light overweight, about half, while one third of non-diabetics reported normal weight. The number of patients with double lumen catheter and with at least six attempts of vascular access prevailed in the diabetic population studied. In the non-diabetics arteriovenous fistula predominated and fewer vascular access attempts.
The complications that most frequently occurred in the case of chronic kidney disease due to diabetic nephropathy were: arterial hypotension, hypoglycemia and infections. In non-diabetics they were predominant, with a significantly lower percentage, hypotension and infections. The cardiovascular disease and the extreme ages of the patients invalidated, to a greater extent, the kidney transplant in both groups.
Protection of people and animals
The authors declare that no experiments have been conducted on humans or animals for this research.
Right to privacy and informed consent
The authors declare that patient data does not appear in this article
Contribution of the authors
Milene Benítez Méndez: control and evaluation of diabetic and non-diabetic patients in hemodialysis control.
Dashiell Millet Torres: control and evaluation of diabetic and non-diabetic patients in hemodialysis control.
Leonardo Curbelo Rodríguez: control and evaluation of diabetic and non-diabetic patients in hemodialysis control.
Francisco Prieto García: writing and shaping the article and style and adaptation.











 text in
text in