Introduction
Malignant gastric outlet obstruction (MGOO) is defined as mechanical obstruction of the pylorus or duodenum caused by extrinsic compression or infiltration from advanced locoregional neoplasms, which impede oral intake and lead to associated nutritional compromise1. This condition is due to the narrowing of the gastroduodenal region, delaying the passage of gastric contents from the stomach to the duodenum1,2. Gastroduodenal outlet tract stenosis is most frequently observed in patients with advanced gastric, duodenal, or pancreatic neoplasms1,3. This complication significantly affects the quality of life of these patients, which is why current palliative treatment strategies include surgical gastrojejunostomy, ultrasound-guided endoscopic gastroenterostomy, or the insertion of a duodenal stent2. Given the high surgical risk and short life expectancy of these patients, endoscopic management with duodenal stents has emerged as a non-surgical alternative to improve symptoms and quality of life, and to reduce hospital stays2.
Gastroduodenal stents have been in use since the 1990s to offer a minimally invasive treatment for these cases3. The technical effectiveness of stent insertion is approximately 97%, irrespective of the technique used (insertion through the working channel, fluoroscopic guide with endoscopic vision, or endoscopic guidance alone). The low rate of technical failure is primarily due to severe distal obstruction that prevents guide advancement for proper stent positioning3,4. Symptom resolution typically occurs around four days post-stent insertion, with improvements in food intake and oral tolerance seen in over 87% of cases. Cases where patients do not exhibit symptomatic improvement are usually due to disease progression or early stent migration5.
The objective of this case series is to describe the experience of duodenal stent insertion in patients with malignant gastric outlet obstruction at a tertiary reference center in the department of Cundinamarca, Colombia.
Materials and methods
This is an observational study, presented as a case series. Data were collected from 17 patients over 18 years old diagnosed with MGOO between December 2019 and February 2022. These patients underwent duodenal self-expanding metal stent insertion in the gastroenterology unit at Hospital Universitario de la Samaritana.
The WallFlex™ duodenal self-expanding metal stent from Boston Scientific, available in sizes of 6 cm, 9 cm, and 12 cm, was used. The stent size was determined based on the length of the stenosis identified through upper gastrointestinal radiography, contrast-enhanced abdominal computed tomography (CT) scan, or during the endoscopic procedure when equipment passage through the stenosis was possible before stent deployment. Most procedures were performed with fluoroscopic guidance and under sedation managed by an anesthesiologist. The Olympus® EVIS Exera II CV 180 equipment was used.
Results
Of the 17 patients included, 76% were men, with a mean age of 69 years (standard deviation [SD]: 11 years). The indication for duodenal stent insertion was malignant pyloric syndrome with oral intake intolerance in all cases (100%), primarily caused by gastric adenocarcinoma confirmed histologically in 82% (14 patients). In two patients, the obstruction was due to compression and infiltration by pancreatic cancer, and in one patient, there was no histological confirmation, with suspected lymphoproliferative disease. 12% (2 patients) had liver metastasis, and 41% (7 patients) had peritoneal carcinomatosis. The technical success rate was 100%, and clinical success, defined as tolerance to a liquid and soft diet, was 88% (15 patients). Clinical success was not achieved in two cases due to persistent nausea and vomiting caused by peritoneal carcinomatosis and distal obstruction. Regarding the stent sizes used, 35% (6 patients) had a 12 cm stent, 53% (9 patients) had a 9 cm stent, and 12% (2 patients) had a 6 cm stent. Fluoroscopic and endoscopic guidance was used in 88% of the cases, as illustrated in Figure 1. The average patient survival during follow-up was 84 days (2.8 months; range: 0-414 days), with one patient still under follow-up after stent insertion within the study period.
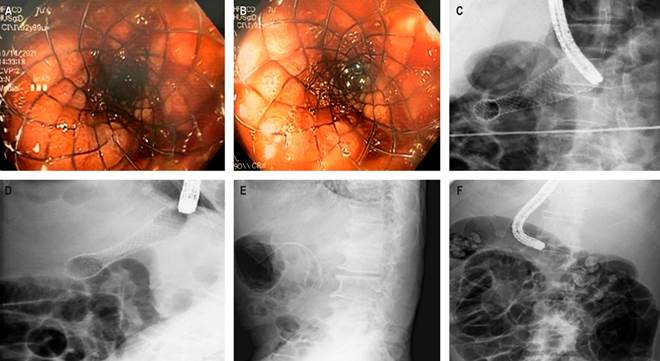
Source: Author’s File.
Figure 1 A and B. Endoscopic images from two cases showing the proximal cup of the deployed stent in the stenosis area. C, D, E, and F. Fluoroscopic images showing stent positioning in cases with different stent sizes.
In patients with gastric adenocarcinoma, the obstruction was located above the papilla, whereas in others, it was due to infiltration of the duodenal bulb and the second portion. No patient experienced stent migration. Due to the short survival of the patients given their advanced oncological condition, no stent intrusion, migration, or obstruction was observed during follow-up. The clinical success allowed for early hospital discharge with tolerance to oral intake, and patients continued in end-of-life care management.
Discussion
Malignant gastric outlet obstruction (MGOO) is caused by the narrowing of the gastroduodenal region, leading to a delay or failure in the passage of gastric contents from the stomach to the duodenum1,2. This condition typically presents with early satiety, weight loss, nausea, vomiting, and abdominal pain1. It is commonly found in patients with advanced gastric, duodenal, or pancreatic neoplasms1,3. In Colombia, the incidence rate of gastric cancer in 2020 was 12.8 per 100,000 inhabitants for both men and women, with a total of 8214 new cases, accounting for 7.5% of all diagnosed cancers6. The prevalence is 4.1%, corresponding to 11,611 cases over the past five years6. The mortality rate for the same year was 9.9 per 100,000 inhabitants, with 6451 deaths from this pathology, making it the third leading cause of cancer-related death6.
Among the complications of gastric cancer, MGOO occurs in 20% of cases, significantly limiting curative treatment options7. MGOO manifests with symptoms such as nausea, difficult-to-manage vomiting, dehydration, abdominal pain, and malnutrition8. Other causes of gastric outlet obstruction include pancreatic neoplasms and, less frequently, duodenal or ampullary neoplasms, cholangiocarcinoma, lymphoma, or adenopathies from other neoplasms9. As previously noted, this complication severely impacts the quality of life of these patients. Current palliative treatment strategies include surgical gastrojejunostomy, ultrasound-guided endoscopic gastroenterostomy with LAMS (lumen-apposing metal stents), or the insertion of a duodenal stent2.
The practice of inserting gastroduodenal stents for malignant pathology has demonstrated similar outcomes regarding success rates, adverse events, and improvements in symptoms and quality of life among experienced groups from Europe, Australia, Japan, and the United States10-13. It has been considered a feasible and safe procedure for managing malignant gastric outlet obstruction. In Colombia, studies have been published comparing duodenal stent insertion with gastrojejunostomy. Castaño and colleagues described a study with 70 patients, which found that the insertion of self-expanding metal stents resulted in better outcomes than surgery in terms of hospital stay duration, oral intake tolerance, and lower morbidity14. Another study conducted in Colombia by Vargas Rubio and colleagues with 31 patients with distal gastric cancer who underwent duodenal stent insertion showed similar results in effectiveness and symptom improvement compared to international studies15.
When comparing the results from our patients with those described in the literature, the average age of our patients is similar to that reported by JP Ratone and colleagues11. Unlike reports from France and Spain, where the primary cause of MGOO is pancreatic cancer10,11, in our study, as well as in the studies by Castaño and colleagues14 and Vargas and colleagues15, the primary cancer causing MGOO is gastric adenocarcinoma.
The technical success rate of stent placement in our study was 100%, comparable to what is reported in the literature, as was the clinical success rate, defined as tolerance to oral intake, which was 88% in our patients3,5. In the study by Vargas and colleagues15, patient survival was 91 days, with similar findings in European case reports10,11. In our study, survival was slightly lower, which may be related to the tumor stage at diagnosis and the characteristics of the patients at our hospital. As a reference center for the department, we serve a population from distant rural areas with significant barriers to healthcare access, which may explain the late diagnosis and advanced disease stage at the time of diagnosis in our patients.
Regarding severe complications associated with the procedure, bleeding and perforation occur in about 1% of cases. Other non-severe complications include stent obstruction, abdominal pain, fever, vomiting, and stent migration5. No other complications were observed in our series. As noted earlier, patients without clinical success had distal obstruction of the stent due to peritoneal carcinomatosis.
In the palliation of malignant gastroduodenal obstruction, several studies have compared the efficacy of metallic gastroduodenal stents and lumen-apposing metal stents released with ultrasound to the standard treatment of surgical gastrojejunostomy.
A study by Jeurnink and colleagues compared self-expanding metal stents with gastrojejunostomy for palliation of malignant gastroduodenal obstruction. The results indicated that self-expanding metal stents could be an effective alternative for palliation in these cases, while surgery is reserved for patients with a longer expected survival (more than six months)16.
Nagaraja and colleagues conducted a meta-analysis comparing surgical gastrojejunostomy and endoscopic stenting for the palliation of malignant gastric outlet obstruction. The results suggest that stent placement is associated with better short-term outcomes, making duodenal stenting a safe means of palliating malignant stomach obstruction17.
We do not have the availability or experience with the use of lumen-apposing metal stents for managing malignant gastric outlet obstruction at our institution.











 text in
text in 



