Introduction
A liver abscess is defined as a collection of pus encapsulated by a membrane, resulting from an infection that causes destruction of the liver parenchyma and stroma1. The incidence in North America is 2.3 per 100,000 hospital admissions, while in Taiwan it is 275.4 per 100,0002. If not properly diagnosed and treated, this condition has a high rate of morbidity and mortality. The most significant predisposing factors for developing a liver abscess are diabetes mellitus (39.6%), gallbladder or biliary tract surgeries (21.3%), and chronic alcohol abuse (10.5%)3.
Liver abscesses caused by foreign bodies, particularly fish bones, represent a potentially severe condition. It is essential to describe this case, characterized by an insidious clinical presentation, nonspecific symptoms, and an unclear history of foreign body ingestion, similar to cases reported in the literature. This case highlights the importance of early diagnosis and appropriate multidisciplinary management, which led to complete resolution of the disease in a short period. When the presence of a foreign body is not initially identified, treatment may be prolonged due to its persistence in the liver, causing abscess recurrence and necessitating multiple percutaneous or open drainage procedures.
Case Report
This case involves a 55-year-old male patient presenting with a one-year history of intermittent abdominal pain localized to the epigastric and left iliac fossa regions, without other associated symptoms. He denied having fever, jaundice, or ingesting any foreign body. His medical history included obesity, hypertension, and frequent alcohol consumption. He presented to our institution for an abdominal ultrasound, which identified a liver abscess in segments II and III containing a foreign body, along with inflammatory changes in the fat of the gastrohepatic omentum (Figure 1). Subsequently, an abdominal CT scan was requested to confirm these findings (Figure 2). The general surgery team opted for hospitalization to provide antibiotic therapy with intravenous ciprofloxacin 200 mg every 12 hours and metronidazole 500 mg every 8 hours. Admission laboratory tests indicated elevated acute-phase reactants (leukocytosis, mild neutrophilia, and C-reactive protein [CRP]), mild alteration in liver enzymes (aspartate aminotransferase [AST]: 52.3 U/L and alanine aminotransferase [ALT]: 23.3 U/L), with bilirubin levels, alkaline phosphatase, and coagulation times within normal limits.

Source: Department of Radiology, Clínica Diagnosticar Clinic. Quibdó, Chocó.
Figure 1 Abdominal ultrasound showing a 3.7 cm linear echogenic structure consistent with a foreign body within, along with an abscess in the left liver lobe.

Source: Department of Radiology, Clínica Diagnosticar. Quibdó, Chocó.
Figure 2 Abdominal CT scan, demonstrating a liver abscess in segments II and III, with a foreign body extending into the adjacent liver parenchyma.
On the first day of hospitalization, an attempt was made to extract the foreign body percutaneously, which was unsuccessful. The patient was then taken for a laparotomy with intraoperative ultrasound to mark the abscess and locate the foreign body. The abscess was successfully drained, and the fish bone was removed (Figures 3, 4 and 5) through a single incision in the liver with minimal bleeding. Hemostatic hepatorrhaphy was subsequently performed using chromic catgut suture with a BP1 atraumatic needle, and a drainage system was left in place. Cultures from the secretion isolated Streptococcus constellatus, a bacterium that is part of the oropharyngeal flora and was sensitive to the empirically initiated antibiotics. In-hospital antibiotic therapy was administered for five days, followed by outpatient treatment to complete a 21-day course. Prior to discharge, an ultrasound showed resolution of the liver abscess and recent postoperative changes in the left lobe (Figure 6).
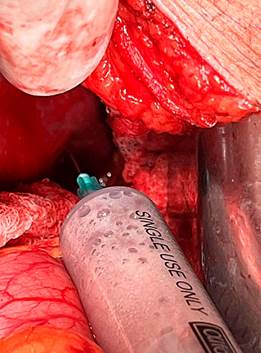
Source: Department of Surgery, Clínica Diagnosticar. Quibdó, Chocó.
Figure 3 Liver abscess drainage.

Source: Department of Surgery, Clínica Diagnosticar. Quibdó, Chocó.
Figure 4 Foreign body (fish bone) removal.

Source: Department of Surgery, Clínica Diagnosticar. Quibdó, Chocó.
Figure 5 Foreign body (fish bone).
Discussion
A liver abscess is a collection of pus and cellular debris within the liver parenchyma due to parasitic, bacterial, or fungal colonization4. The incidence and mortality are more closely associated with bacterial abscesses, and these rates have declined since the introduction of percutaneous drainage, affecting 20% to 60% of cases5, with rupture being the primary complication4. Currently, no studies in our region indicate its prevalence; however, due to sociocultural conditions, limited access to public services, and sanitation levels, the primary presentation of liver abscesses in Colombia is amebic6. Pyogenic abscesses have an incidence of 2.3 cases per 100,000 population7. The etiology is polymicrobial, with pathogens such as Klebsiella pneumoniae, Escherichia coli, and Streptococcus species (when produced by foreign bodies8,9), including the Anginosus group, which has three representative species including constellatus, commonly found in oropharyngeal, upper gastrointestinal, and urinary tract flora8. While mortality from liver abscesses remains significant, recent studies report a substantial decline, with rates varying between 11% and 31%. Streptococcus is the most frequently isolated pathogen, although the etiologic agent remains unknown in about half of the cases10. Predisposing factors for pyogenic liver abscesses include diabetes mellitus (39.6% of cases), biliary tract interventions (21.3%), and chronic alcohol abuse (10.5% of cases)3.
Liver abscesses due to foreign bodies are extremely rare and may result from the ingestion of materials like needles, chicken bones, and fish bones-the latter being the most common among adults11. The first case of liver abscess associated with an intrahepatic foreign body was reported in 189812, but liver abscesses specifically related to fish bones remain scarcely reported, limited to isolated case reports. Once a foreign body is ingested, the primary sites for penetration into the liver are the stomach and duodenum13, where it typically lodges in the liver’s left lobe11. Only 1% of accidental foreign body ingestion results in perforation14, making these severe and unusual cases that pose diagnostic and therapeutic challenges. Symptoms may vary from one to three weeks15,16 or extend over months or even years11 and include nonspecific symptoms such as fever, upper abdominal quadrant pain, weight loss, vomiting, and anorexia9. Migration of a foreign body to the liver can remain asymptomatic for an extended period and is generally detected only once infection or abscess formation occurs. Therefore, diagnosis based on medical history and physical examination is challenging: suspicion is typically low due to both the patient’s lack of awareness of foreign body ingestion and the nonspecific nature of symptoms, which can mimic other causes of abdominal pain, including renal abscess, subphrenic abscess, acute cholecystitis, acute appendicitis, cholangitis, pleurisy, lung abscess, and severe infectious diseases in general10.
In the presence of a foreign body, the ideal treatment involves a combination of object removal, abscess drainage, and antibiotic therapy, as very few cases can be successfully managed with conservative approaches alone in this context11,17,18. Broad-spectrum antibiotic therapy should be initiated promptly and should not be delayed by awaiting culture results. The duration of antibiotic therapy should extend to a maximum of two weeks, followed by appropriate oral treatment for an additional four to six weeks18.
Advances in combining surgical techniques and imaging have made it possible to use flexible-tip laparoscopic ultrasound in minimally invasive procedures, allowing for fewer incisions and high success rates with reduced tissue damage. In our case, laparotomy with intraoperative ultrasound marking was used due to local resource availability, yielding excellent results as only a single incision was required for abscess drainage and foreign body extraction19-21.
Conclusion
The overall prognosis for patients with this type of abscess depends on comorbidities and the speed of diagnosis and treatment. For abscesses requiring multiple drainages or with atypical contents, the possibility of an associated foreign body should be considered to enable a timely and appropriate therapeutic approach with suitable surgical techniques, as in this case, to reduce mortality in these patients.











 text in
text in 




