INTRODUCTION
Infertility, a global health concern affecting one out of six couples, often leads to profound emotional pain. Infertile couples experience feelings of vulnerability, fear, and overwhelming grief, challenging their life-defining narratives. While ethical analysis often focuses on the objective aspects of technologies, it often overlooks their impact on a deeply personal level. Here, the Church's role becomes indispensable. It provides compassionate pastoral care and support, proving the fruitfulness of married lives without progeny in all its ways and spheres, including marriages without the blessing of children (1 p23). The Church is committed to providing accurate information and correcting misconceptions in counseling. It continues to guide couples through moral conflicts and technology-related practices. This article aims to investigate infertility issues and treatments, with a specific emphasis on the Church's role in addressing this problem. It provides a framework to address complex questions and dilemmas associated with infertility.
1. DEFINITION AND CAUSES OF INFERTILITY
The medical definition of infertility is failure to conceive after one year of unprotected (without contraception) sexual intercourse 2-4. The time limit of twelve months is arbitrary but corresponds with many couples who achieve pregnancy spontaneously within one year. So here, it is clear that if the couple has familial reason to suspect infertility in any of them, there is no need to postpone the investigation for infertility until the period of one year (5 p20). In scientific literature, infertility is divided into primary and secondary. Primary infertility, also called "absolute," refers to the woman who has never conceived despite regular intercourse without contraception for twelve months (3,6 p413,7). Secondary or relative infertility is defined as the inability to carry a baby who has previously conceived (3,6 p412,7). Infertility can be caused by prolonged use of hormonal contraception, various environmental influences, genetic disorders, increased stress levels, and sexually transmitted diseases, while achieving pregnancy requires adequate hormone levels and proper physiology 8. Although the inability to achieve a pregnancy within twelve months may be an indication of possible infertility, the doctor must carry out a thorough assessment of the couple to determine the cause and institute the proper measures to address the problem.
1.1 Female Infertility Causes
Female infertility can result from a multitude of causes, each affecting the reproductive system differently. These causes can be broadly categorized into ovulation problems, structural issues with the reproductive organs, and other health conditions 9. The following are some of the causes of female infertility 3,8,10-13.
Ovulation Disorders-occurs when disruption in the part of the brain that regulates ovulation causes low levels of luteinizing hormone (LH) and follicle-stimulating hormone (FSH). Even slight irregularities in the hormone system can prevent the ovaries from releasing eggs, leading to anovulation 13.
Polycystic Ovary Syndrome (PCOS)-results from excessive production of androgen hormones, which affects ovulation 11. The ovaries may not release an egg regularly or may not release a viable, healthy egg. Additionally, in women with PCOS, even if a healthy egg is released and fertilized, the uterus may not be receptive to the implantation of the fertilized egg.
Poor Egg Quality-eggs that are damaged or developed chromosomal abnormalities cannot sustain a pregnancy 12. This issue is often related to age.
Elevated Prolactin (Hyperprolactinemia)-is characterized by high levels of the hormone prolactin, which is responsible for milk production in women and can disrupt ovulation. An excess of prolactin can lessen estrogen production, causing infertility and affecting testosterone levels 14.
Early Menopause (Premature Ovarian Failure)-is defined as the absence of menstruation, and it occurs before the age of 40 15. Certain conditions are associated with early menopause, including immune system diseases, radiation or chemotherapy treatment, and smoking.
Thyroid Problems-include disorders of the thyroid gland, such as hyperthyroidism (excessive thyroid hormone) or hypothyroidism (insufficient thyroid hormone), which can disrupt the menstrual cycle and cause infertility 16.
Damage to the Fallopian Tube-usually results from inflammation of the fallopian tube (salpingitis). Tubal damage may result in a pregnancy in which the fertilized egg is unable to make its way through the fallopian tube to implant in the uterus (ectopic pregnancy) (17 p129,18 p141).
Pelvic Adhesions-occur when bands of scar tissue bind organs after pelvic inflection, appendicitis, or abdominal or pelvic surgery. This scar tissue formation can impair fertility (19 p605).
Uterine Fibroids-are noncancerous clumps of tissue and muscle on the uterus wall, common in women in their thirties and forties (20 p20). Rarely, they may cause infertility by blocking the fallopian tubes and interfering with the proper implantation of fertilized eggs 21.
Endometriosis-occurs when the uterine tissue implants and grows outside the uterus. This can lead to scarring and inflammation, resulting in pelvic pain and infertility in women 22.
1.2 Male Infertility Causes
The male fertility process involves the production of mature sperm that must reach and fertilize the egg. Issues with meeting any of these conditions can contribute to infertility (8 p6). Male infertility can result from various factors that affect sperm production, function, or delivery. Male infertility cases are often due to a combination of biological and environmental factors 8,10-12,23, such as:
Sperm Disorders-including low or no sperm counts, poor motility of sperm, and abnormally-shaped sperm unable to reach or penetrate the egg, can all lead to infertility 24.
Varicocele-happens when the veins on a man's testicle are too large, which may prevent normal cooling of the testicle, leading to reduced sperm count and motility 25.
Undescended Testicle-occurs when one or both testicles fail to descend from the abdomen into the scrotum during fetal development. Due to higher internal body temperature, sperm production may be affected 24.
Testosterone Deficiency (Male Hypogonadism)-can result from a disorder of the testicles themselves or an abnormality affecting the hypothalamus or pituitary gland, which produces the hormones that control the testicles 26.
Inflections-may temporarily affect sperm motility. Repeated bouts of sexually transmitted diseases (STDs), such as Chlamydia and gonorrhea, are often linked to male infertility, as they can cause scarring and block sperm passage. If mumps, a viral infection usually affecting young children, occurs after puberty, inflammation of the prostate (prostatitis), urethra, or epididymis may potentially alter sperm motility 8,27.
Genetic Defects-include conditions like Klinefelter's syndrome, where a man has two X chromosomes and one Y chromosome instead of one X and one Y. This causes abnormal development of the testicles, resulting in low or absent sperm production and possibly low testosterone levels. Other genetic syndromes associated with infertility include cystic fibrosis and Kallmann's syndrome 28.
Impaired Delivery of Sperm-may involve sexual issues such as erectile dysfunction, premature ejaculation, painful intercourse (dyspareunia), or psychological or relationship problems. Other causes include retrograde ejaculation (when semen enters the bladder during ejaculation rather than emerging out through the penis), blockage of the epididymis or ejaculatory ducts, lack of semen (ejaculate) resulting from spinal cord injuries or diseases, and anti-sperm anti-bodies that weaken or disable sperm 29.
In conclusion, infertility in both females and males can be attributed to a diverse range of biological, environmental, industrial-chemicals, radiation-and lifestyle factors-obesity, excessive substance use, smoking weight, and stress-each impacting the reproductive system in different ways. Understanding these varied causes is crucial for effective diagnosis and treatment, ultimately helping many couples achieve their goal of parenthood.
2. TREATMENTS FOR THE INFERTILE COUPLES
Successful treatment relies on the efficient and informed evaluation of affected couples, as it helps avoid unnecessary high-level interventions (30 p344,31 pp85-87). Evaluating both partners is crucial for identifying causes and developing a treatment plan, as the couple's health is vital for positive outcomes. Preconception care helps the couple conceive an optimum state of health by including health promotion, risk assessment, and interventions per individual needs 32-34. According to WHO policy (2013), preconception care involves providing biomedical, behavioral, and social health interventions to women and couples before conception 35,36. Key aspects of health promotion are nutrition, exercise/weight management, avoiding substance use, stress management, and screening for sexually transmitted infections 32-34,37,38. Additionally, managing preexisting medical conditions and their medication is essential before planning a pregnancy 39,40.
Accordingly, effective preconception care provides preventive, promotive, or curative health and social interventions, maximizing the chance of conception without complications. For example, there may not be treatment for some women, those who have been using contraceptive pills for years, but simply more time for the resumption of ovulation 41. Optimizing the chance of conception involves identifying the most fertile days and understanding the best timing for intercourse. In short, making conscious choices to optimize both partners' health and well-being before pregnancy through proactive steps increases their chance of conceiving successfully. All these possibilities should be considered before undergoing infertility treatment 33.
Due to the significant technological advance, surgery 42,43 utilizing the operative microscope treats tubal obstruction. In short, blocked fallopian tubes can be treated with microsurgery 44 and tubal recanalization 45,46, potentially restoring fertility in couples who have undergone sterilization. Varicocele, a correctable cause of male infertility, can be treated through a surgical procedure called varicocelectomy 25. In case the cause of infertility is ovulation defects, ovulation induction may be used with a mild stimulation protocol of superovulation hormones under controlled conditions to induce a normal ovulatory cycle 47. Ovulation induction in anovulatory women is a landmark in reproductive endocrinology, involving follicle development to treat anovulatory patient, either alone or in combination with other treatments, such as intrauterine insemination (IUI) or other assisted reproductive techniques 48,49. IUI can be performed in a natural cycle as well as in combination with controlled ovarian hyperstimulation (COH) 50. This fertility treatment involves placing sperm directly into the uterus to increase the number reaching the fallopian tubes, thereby enhancing the chance of conception (13 p7). Controlled ovarian stimulation with low-dose gonadotropins combined with IUI offers significant pregnancy benefits compared with natural cycle or timed intercourse while reducing complications such as multiple pregnancies and ovarian hyperstimulation syndrome2 (OHSS) 51. Strict patient selection criteria and individualized stimulation protocols tailored according to the age and etiology of the patient with a strict cycle cancelation policy will help to reduce complications and maximize pregnancy outcomes 52. In short, ovulation induction,3 surgery, and artificial insemination are still the most widely used approaches for overcoming infertility, and recently, NaProTechnology has opened new ways to treat infertility problems.
2.1 NaProTECHNOLOGY
NaProTECHNOLOGY4 (NPT), or Natural Procreative Technology, is considered a restorative reproductive medicine5 (RRM) 54 and relies on Fertility Awareness-Based Methods (FABMs) like the Creighton Model FertilityCare™ System (CrMS) to diagnose and treat chronic disorder affecting fertility, thereby restoring the body's natural ability to conceive (55 p191,56 p19,57,58). NPT integrates family planning with procreative and gynecologic health monitoring and maintenance, promoting cooperation with the woman's cycle and allowing knowledge, understanding, and medical applications to unleash the power within it (56 p19). NPT, a medical approach that combines education and advanced technology (targeted hormone surveys, expert ultrasound evaluations, and surgical techniques like laser technology and microsurgery), educates women about their bodies, improves their health, and resolves reproductive issues, enabling physicians to identify and treat underlying conditions effectively 59. This system is a highly reliable family planning system and is good in evaluating and treating women who have infertility and reproductive disorders, abnormal bleeding, hormonal issues like recurrent ovarian cysts and premenstrual syndrome, pregnancy dating, and postpartum depression, and various other conditions 55,56,59,60. In short, NPT is a medical science founded on patient education and integrated with good medical practice. In particular, it teaches women about their menstrual and fertility cycles, enabling them to partner with trained physicians to evaluate and treat gynecologic or reproductive issues 59. Modern medicine has generated a host of new choices that were unimaginable to people in previous generations.
2.2 Assisted Reproductive Technologies (ARTs)
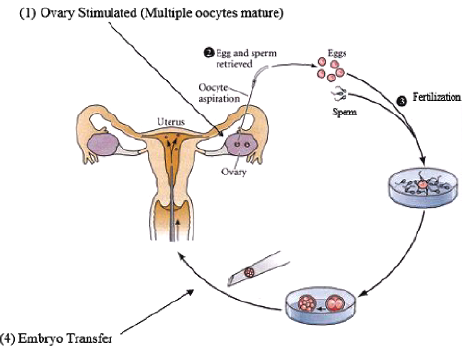
Assisted reproductive technologies (ARTs) are any attempts, treatment, technique, or procedure to overcome obstacles to bearing a child in the biological continuum of events 61,62. This study gives importance only to the hypothesis of infertility treatment through homologous artificial fertilization. The issue of heterologous fertilization will not be addressed, which discloses, in addition to those relating to the technique, further severe ethical problems due to the involvement of third parties outside the couple in the fertilization and gestation process. The extracorporeal fertilization and embryo transfer became a reality with the birth of Louise Brown in 1978 (63 p101,64). "The most frequently used infertility treatment procedure is the fertilization of eggs by the sperm by IVF followed by embryo transfer to the uterus (ET)" 65. In vitro fertilization6 66 and embryo transfer (IVF-ET) were devised because of obstruction of the fallopian tubes 67. All assisted reproduction shared a common goal of bypassing pathological obstacles such as blocked fallopian tubes and non-functioning ovaries in females and blocked vas deferens and low sperm count in males 68. The procedures of ARTs (69 p101) are individualized for the couple being treated. Figure 1 (70 p66) illustrates the four IVF process steps divided into 1. Ovarian Stimulation, 2. Egg Retrieval, 3. Fertilization, and 4. Embryo Transfer into the Uterus.
At present, various treatment options for infertility can be categorized by whether the sperm and oocytes are brought together in the uterus (intrauterine insemination) or laboratory (IVF and intracytoplasmic sperm injection - ICSI) 65,71. Several alternatives to IVF-ET have been introduced, including gamete intrafallopian transfer (GIFT)7 and zygote intrafallopian transfer (ZIFT). In these methods, either oocytes and sperm or fertilized oocytes are transferred into the fallopian tube (72 p84). GIFT was popularized by Ricardo H. Asch from the USA, while ZIFT was pioneered by Paul Devroey and colleagues in Belgium 31. ZIFT covers all other acronyms that have been used in the past to describe similar or related procedures such as pronuclear stage transfer (PROST), tubal embryo transfer (TET), tubal embryo stage transfer (TEST), and surgical embryo transfer (SET) 31. There is another procedure called gamete intrauterine transfer (GIUT), which is a simplified version of GIFT, and the significant difference between GIUT and GIFT is that the fertilized egg and sperm are placed into the uterus and not into the fallopian tube (73 p7).
Although nonsurgical procedures are being investigated for the transvaginal delivery of gametes into the fallopian tube, this approach remains experimental. However, it has been reported that a successful pregnancy resulted from a transvaginal, intraperitoneal injection approach, i.e., peritoneal ovum sperm transfer (POST) 62. A significant development in in-vitro fertilization is the application of micromanipulation to human oocytes and embryos. The technique of zona drilling (ZD) or partial zona dissection (PZD) involves micromanipulation techniques that have been devised to provide fertilization assistance that entails the mechanical introduction of any opening in the zona pellucida, thereby allowing sperm direct access to the oocyte (62 p40). In addition, these procedures are associated with many other serious complications.
3. ARE INFERTILITY TREATMENTS SAFE?
Although infertility treatments using in vitro fertilization often result in pregnancy, they also carry risks. The medical risks of ARTs depend on each step of the process. The primary risk caused by ovarian stimulation is ovarian hyperstimulation syndrome (OHSS) and its complications 51,74-77 p16). Transferring more than one embryo in ARTs raises the risk of multiple pregnancies 31,78 and preterm delivery with lifelong disabilities. The chance of ectopic pregnancy8 and miscarriage are risk factors in ART procedures 80. When ICSI is used in cases of severe male factor infertility, a genetic cause of male infertility may be passed on to the offspring. The list of possible risks related to the ART procedure, which can be seen in all aspects, is given in Table 1 81 p152,82).
Table 1 Potential Risks Associated with ARTs I Potential Risks Iatrogenic to ARTs
| Potential Risks Iatrogenic to ARTs | |
|---|---|
|
Hyperstimulation Ovarian torsion Infection, bleeding, and even death Failure to conceive Multiple gestation Prematurity and "small for gestational age" infants |
Birth defects Health risks later in the life of children born after ART Disorder of epigenetic imprinting Risks from handling of gametes and embryos Risks of culture Risks associated with cryopreservation Gamete and embryo "mix-ups" |
Source: Taken from 81.
Furthermore, ARTs involve significant physical, psychological, financial, and emotional stress on the part of couples, particularly when facing the repeated failure of implantation (RIF) or recurrent pregnancy loss (RPL) 83. The potential risks of ARTs are variable due to different factors, including sperm morphology, infertility causes, baseline levels of follicle-stimulation hormone (FSH) and estradiol, preconception folic acid supplementation, type ARTs, the day of embryo transfer, the number of transferred embryos, the ovarian stimulation protocol, history of ovarian hyperstimulation syndrome, the mean number of retrieved eggs, fertilized eggs, viability, and quality of the embryo 84. Therefore, there are serious questions about ARTs, including their safety and potential effects on the health of mothers and children.
3.1 Risks for the Mother
Some research indicates that ARTs pose risks to maternal health, including pregnancy-related hypertensive complications 85, gestational diabetes 86, and other maternal morbidities 87, such as increased risk of hemorrhage, mood swings, and cesarean delivery 70,88-90. Ovarian stimulation is associated with risks to the mother, such as that it can lead to hyperstimulation, causing the ovaries to become swollen and painful 77 p15). Ovarian hyperstimulation can lead to dangerous side effects such as increased hormone production, excess fluid collection, cyst development, blood coagulation problems, stroke, cardiac arrest, molar pregnancy (abnormal, non-fetal cell development) and ovarian cancer 66,70,75,77,91,92 p74). There is also a chance for multiple pregnancies in ARTs involving multiple fetuses to pose increased risks of spontaneous preterm delivery, maternal complications, and increased mortality rates (82 p765). The risks of cerebral palsy, periventricular leukomalacia, and intraventricular hemorrhage are increased by preterm delivery, especially in cases of multiple gestations 82,93. Women undergoing IVF have a twofold higher risk of tubal pregnancy due to the placement of the catheter and the high volume of fluid injected together with the embryo, which can cause them to back up and implant into the oviduct instead of the uterus 66,70. However, to avoid the risks attached to the birth of several children at the same time will lead to selective reduction; that is, abortion of one or several fetuses has been offered to mothers in cases of multiple pregnancies. The procedure requires the mother's informed consent, which involves the destruction of some of her unborn children and may additionally affect her physical and psychological well-being 66. Finally, there exists a chance of infectious disease transmission between the mother and the child in certain IVF situations involving sperm donation, such as human immunodeficiency virus (HIV) types 1 and 2, and hepatitis B (HBV) and C (HCV) viruses (66 p14,94-96.
3.2 Risks for the Embryo or the Child
Superovulation treatment can disrupt the mother's hormone balance, potentially affecting the uterine lining and rendering it less receptive to embryo implantation, causing early embryo loss 83,97. Because endometriosis has significant physiological effects, such as immunological dysfunction, hormonal imbalances, and decreased endometrial receptivity, pursuing IVF for associated infertility may appear hopeless due to diminished gamete and embryo competence 97,98. The possibility for manipulation of embryos in ARTs is high. These include the overproduction and freezing of embryos to maximize the success rate, the reduction of embryos, or the random suppression of some implanted embryos to reduce the risk of multiple pregnancies, and the possibility of selecting the embryos to produce (following preimplantation genetic tests) 82,99,100. Advancements in embryo culture, preimplantation genetic screening, growing awareness of multiple gestation risks, and optimizing perinatal outcomes have made focus on single-embryo transfer 82. Then, the main risk of the embryo is that once fertilized, it could not arrive at autonomous life because it is not transferred to the woman's reproductive tract, and as it did not attach to the uterus, there are chances for a spontaneous or a provoked abortion (101 p474).
Scientific studies indicate that children born through ARTs show a greater predisposition to suffer from hypertension, diabetes, thyroid disease, and certain neoplasms, particularly leukemia 93. Children born by ARTs may have higher risks for epigenetic alternation and adverse perinatal outcomes, which may be associated with childhood cancers. A nationwide population-based cohort study of 2,308,016 eligible parent-child triads in Taiwan from 2004 to 2017 identified 1,880 children with incident childhood cancer like leukemias, hepatic tumors, and incidence rate of retinoblastoma, with data analyzed from 2020 to 2022 102. This cohort study revealed that out of 2,308,016 children, 188,231 (8.16 %) were preterm, and 170,312 (7.38 %) had low birth weight, with the highest percentages of multiple gestations (23,081 [48.95 %]), preterm birth (17,185 [36.45 %]), and low birth weight (17,141 [36.35 %]). An excess risk of minor and major congenital malformation (CMs) or anomalies in infants born after ARTs has also been detected (84,103 p24,104). The frequent structural congenital malformations are congenital heart defects, neural tube defects (NTDs), facial cleft, gastrointestinal malformations, genitourinary malformations, and imprinting disorders (ImpDis) 88,105--107. There was also an increased risk of imprinting disorders like Beckwith-Wiedemann syndrome (BWS) and Angelman syndrome (AS), Silver-Russell syndrome (SRS), maternal hypomethylation syndrome, and Prader-Willi syndrome (PWS) 108-113. To summarize, infertility treatments can carry significant risks, and the future of offspring is uncertain due to potential unexplored problems (93 p40). Therefore, it is the physician's responsibility to ensure the welfare of the infertile patient by providing an objective assessment and proposing therapies that balance medically acceptable risks with potential benefits 62. Ultimately, couples should make their own decisions about infertility treatment, considering their characteristics and values.
4. DIFFICULT ETHICAL DILEMMAS POSED BY THE PHENOMENON OF INFERTILITY
According to recent studies by the World Health Organization (WHO), infertility is a global health issue affecting approximately between 48 million couples and 186 million individuals 114. Medical science explained infertility as a medical problem and increased the chance of giving solutions to the problem with different treatment options. The primary motivation for the development of infertility treatments is the desire to have children, and it is entirely legitimate to find ways to overcome infertility. The couples should be aware of the moral implications of ARTs, which involve procedures meant to increase the success rate, like the production of supernumerary embryos or selective abortion to eliminate extra embryos as well as multiple pregnancies, greater risks of health complications for the child and the mother, and the instrumental treatment of thus conceived life (115 p226,116 p99). ARTs can alter traditional ways of forming families and of individuals relating to each other by violating the natural order of procreation; that means they offer a possibility to initiate human life with the omission of conjugal sexual acts 116,117. Generally, these treatment options raise many serious ethical problems related to human procreation and safeguarding the conjugal unity and the life and dignity of the embryo.
The ART process may transform the first moment of life into a technological production, with the human embryo becoming a biological product that fullfils our desires, replacing procreation with production (116 p103). The central figure in the process of assisted reproduction, directly affected by every action, is the child born with the aid of infertile treatments (118 p37). Treating a child like a commodity for parents' desires will neglect their dignity, leading to the view of a child as personal property, with certain infertile treatment options (119 p51). It is a slippery slope that undermines human dignity as children become products of technology, consumer goods that parents paid for and have a right to expect 115. Here, we must keep in mind that "what is technically possible is not for that very reason morally admissible" (120 n4); human procreation is a personal act of the couple, involving the responsibility of the spouses' marital structure (121 p475). Therefore, we have to consider and welcome children as gifts and must treat them as equals to us despite their dependency and powerlessness 1. It is so hard for an infertile couple to cope with the challenge of their natural desire to be parents and establish a family. However, the infertility clinics do not provide appropriate moral guidance about the treatment option under consideration, nor spiritual support to couples. Thus, the new ARTs will inevitably raise moral and religious questions about using technology to reproduce.
4.1 The Catholic Principles to Determine the Morality of ARTs
The ethical evaluation regarding the new reproductive techniques came about simultaneously with its progress, and the mere existence of technological intervention does not provide moral acceptance of its issue. However, in the Catholic Church, theologians expressed an appropriate evaluation immediately after the first successes of in vitro fertilization, and it helped us to foresee the imaginable implications of the new biological reproductive technologies. In the light of the instruction "Donum vitae," the criteria used by the Church to determine the morality of reproductive technologies pertains to the nature and fundamental goods of the human person about the marriage and the family, human sexuality, and the defense of human life before birth (122 p33).
4.1.1 Respect Life as a Gift from the Beginning Itself
The infertility treatment options raise many moral questions about human life. We can make fundamental human life decisions by properly understanding life and its value. The theological aspect of "created in the image of God" leads to the reality of human life. The significance of man lies in the image of God he bears upon himself (123,124 p697). The reflection on the biblical account of creation clarifies the theme of the human person as the image of God by two essential aspects of human mirroring of God: "beings endowed with intellects and free will" (125 p39). The aspect of His image-bearing confers significance upon all the dimensions of man and makes man the ground of all other values. The Instruction for Human Life (Donum vitae) starts by referencing the gift of life and our responsibility towards human life 122. Created life should be accepted as a gift and have an author and source beyond itself. Here, gifts have a metaphysical implication: "The category of giving belongs to the metaphysical act of creating a person, and the category of gift is itself a metaphysical element of man's existence" (126 p72). Man's existence is given to him, and his existence is essentially and necessarily a gift. Therefore, we should respect the moral status of the human embryo, stating that every human being has a right to life from conception itself.
4.1.2 The Moral Status of the Human Embryo
According to science, from conception, a living being is biologically separate from the mother, and this new being is unique. Here, it is apt to analyze the term embryo, which is derived from a Greek word meaning "growing within" and the successful fusion of sperm and egg results in the formation of a new diploid cell, zygote, which is derived from the Greek word, meaning "yoked together" (127 p322). We can call a zygote totipotent because, by virtue of its human genome, it is intrinsically capable of giving rise to the whole offspring 127. Thus, an actual human individual begins their existence from the moment of conception itself (120 I nl). The scientific studies state that the biological process is characterized by the continuous emergence of a form from previous stages without discontinuity (epigenesis):
Three properties are verified across the stages of the zygote, blastocyst, and embryonic disc with implantation in the uterus: 1) co-ordination, with a consequent interaction and co-ordination of cellular and molecular activities under the control of a new genome, modulated by an uninterrupted cascade of signals transmitted from one cell to another; 2) uninterrupted continuity in the process of development of the progressive differentiation of the individual and realization of its proper identity; 3) gradual development towards a growing complexity of the whole. The individual cells of this embryo cannot be considered separately from each other, for they are tightly integrated within a single dynamic process, constituting a unity of being. (128 p209)
The Church teaches that each person must be respected as intrinsically good from the moment of conception, and this right to life is the fundamental right from which all other rights flow (129 n2). Therefore, the human embryo, beginning with the fusion of the gametes, has the value and title of a human person, with a fundamental right and dignity to life, to the love of his parents (128,130,131 p28).
4.1.3 The Unitive and Procreative Dimension of the Conjugal Act
A child is conceived by loving sexual intercourse, which is the result of the loving personal action of parents (132 n80-81). The unitive and procreative dimensions belong to the divine design for human procreation. According to Humanae Vitae, the married couple can achieve the vocation to parenthood willed by God only by respecting the inseparable connection between the two aspects of the conjugal act: the unitive and the procreative meaning (133 n12). The unitive and procreative dimensions of the conjugal act are fulfilled in and through the mutual gift that necessarily includes their procreative capacity and a complete interpersonal union (134 p104,135 n48). Then, any technologies or intervention separating the inseparability of the unitive and procreative union of conjugal acts will be morally illicit.
4.1.4 Assisting versus R1eplacing the Conjugal Act
The child is a special gift because it is begotten, not made, by a being with its parents; therefore, they are equal as human beings. The Instruction for Human Life explains that generating human life outside the marital act is wrong because doing so treats the child as if they were a product or just like a possession (136 nlII). The Catechism of the Catholic Church declares morally unacceptable techniques that "disassociate the sexual act from the procreative act" (CCC 2377). It is important to differentiate the meaning of "the substitution" and "the replacement" in the conjugal act. Since assistance to the marital act includes assistance to the generative process as a natural objective beyond the physical act, the meaning of substitution or replacement must also refer to that process beyond coitus (137 p79).
We will get a clear idea from the distinction between assistance and replacement from the general idea of "principal cause" and "instrumental cause" (137 p81). A principal cause can be defined as "one that is per se responsible for whatever effect it produces" and which acts by its power (138 p288). Thus, the principal cause is necessarily ordered to its effects, and there will be a link between effect and cause. The marital act is described in terms of per se causality in the Instruction for Human Life, where it states that the marital act is "per se suitable for the generation of children to which marriage is ordered by its nature and by which the spouse become one flesh" (120 IIB, n4). Therefore, we can say that the marital act of spouses stands as a principal cause since both spouses act together as principal agents in action ordered to the effect of the existence of a new human life (120 IIB n4). Thus, the spouses are the conjoined principal cause of the child in and through their conjugal act. An instrumental cause is intrinsic to the principal cause or agent, which uses the instrument to effect. So, the effect is not produced by the instrument but by using the instrument and in virtue of the principal cause (139 p152). ARTs, in general, reduce the sense of generating a child to the mere biological act that derives from a decision and forget that life is the fruit of an act of love; it is openness to possibility inscribed in existence, but only a possibility, not a duty 1. Therefore, procedures that assist or facilitate the marital act will be morally permissible; those that replace the conjugal act and fertilization outside the mother's body are unacceptable. This moral norm respects the unitive and procreative dimension of the marital act.
4.1.5 Responsible Parenthood
Responsible parenthood refers to moral conduct, one of the dearest expressions of the moral agent's liberty. The term "responsible parenthood" intended the decision to procreate or not to procreate and the execution of this decision, which should take account of the concrete circumstances of spouses for the education of children, society, and the Church 140. Responsible parenthood reminds us that there is a profound link between the marital bond and the gift of life, which means the spouses are called to give life, and there must exist grave reasons before they decide not to procreate. In the pro-choice culture, the sense of parenthood and responsibility reduces merely to procreative capacity relating to a choice 1. Here comes the question of the implementation of a morally correct decision not to procreate by any contraception, which is regarded objectively as morally wrong. In the encyclical letter, Humanae Vitae taught that the contraceptive act, used in the execution of decisions, is always objectively illicit. We can say that the decision not to procreate can only have legitimate, ethical execution by engaging in the marital act during the wife's infertile period. Therefore, true responsible parenthood implies an education in virtue because there is always a slippery slope that natural methods can be employed in the context of the contraceptive mentality 140. Spouses can use natural methods to support a procreative decision. However, spouses can fulfill all the responsibilities of parenthood only with mutual support based on a sincere commitment.
5. COMPASSIONATE PASTORAL ACCOMPANIMENT TO THE INFERTILE COUPLE
The role of the Church is unique and irreplaceable; it offers compassionate pastoral care and support to help infertile couples carry their sufferings. The Church acknowledges the pain caused by infertility and urges scientists and medical professionals to investigate its causes as well as potential preventative and therapeutic solutions, as outlined in the Instruction "Donum Vitae" by the Congregation for the Doctrine of the Faith (66 p40,120 IIB n8,141 p257). At the 18th General Assembly of the Pontifical Academy for Life (2012), scientists were encouraged to pursue ethical and scientifically sound solutions to infertility, respecting the integral humanity of the subjects involved 142. The Church advocates for medical techniques that assist the procreative act rather than replacing or substituting it, ensuring the moral obligation that the provided means must respect the dignity of spouses and children (CCC 2376).
5.1 Promoting Science Compatibility with Catholic Teaching
The Church always gives importance to the service of science to the integral good of the life and dignity of every human being (CCC 2375) (143 n3). Catholic opposition to certain forms of assisted reproduction is not rooted in an anti-technological mindset (CCC 2377) but rather prioritizes the intrinsic value of human life. That means, rather than pursuing immoral techniques to obtain conception, the Church, in Her wisdom, advocates for the healing of whatever is not working properly in human bodies that causes infertility. So, the Church is not rejecting all infertility treatments; for example, hormonal treatments for infertility and surgery for endometriosis are both perfectly acceptable. The Church defines permissible ARTs as procedures that relocate sperm or ova before or after sexual intercourse, such as a surgical procedure to move sperm past an epididymis blockage, followed by regular sexual intercourse (144 p109). Low tubal ovum transfer (LTOT) was developed in Dayton, Ohio, by Dr. David McLaughlin as a remedy for blocked or diseased fallopian tubes, which involves relocating the ovum from a woman's ovary and then reinserting it in the lower portion of the tube or the uterus (144 p109,145 p409). The couple was encouraged to engage in marital intercourse before and after the scheduled LTOT procedure, which directly introduces sperm to the ovum, making it morally licit and facilitating union (146 p 81). Some marital acts are fruitless because the husband's sperm does not migrate enough into the reproductive tract of his wife. So, after the marital act, the physician uses a syringe to extract the semen from the vagina and propel it into the uterus and fallopian tubes (146 p81,147 p111). Here, it is evident that this procedure assists the marital act and does not replace it by removing obstacles that prevent the fruitful marital act or providing necessary conditions for its effectiveness. In the language of the Instruction for Human Life, these techniques are "authentic" because: "once the problem causing infertility has been resolved, the married couple can engage in conjugal acts resulting in procreation without the physician's action directly interfering in that act itself' (143 n13). Thus, a medical intervention that respects the dignity of persons when seeking to assist the conjugal act is morally acceptable, but a medical procedure that technologically replaces the conjugal act is morally unacceptable (120 IIB n7). The Church supports integrated primary infertility treatment methods provided by trained generalist physicians, such as natural procreative technology, which has the potential to improve access to care for infertile couples in primary care settings. The Church never conflicts with science but accompanies humans with courage and hope with its full consciousness of every human procedure.
5.1.1 Moral Acceptance of NaProTechnology
NPT is morally accepted by the Catholic Church as a way of managing fertility that protects the dignity of the couple's sexual relationship and was developed on the functional principles of the Encyclical letter, Humanae Vitae (Human Life) 148. NPT avoids suppressive or destructive methods, using a fertility-care approach that works cooperatively with the procreative and gynecologic systems 149,150 p65). Studies have shown that using the CrMS, 20 % to 40 % of infertile couples can achieve pregnancy within 6 to 12 months, similar to the success rate of a single IVF cycle 151. When combined with NPT, the success rate can increase to 80 % depending on the underlying medical condition 152. Research in RRM shows that NPT is nearly three times more successful than IVF in assisting infertile couples, avoiding early abortions or frozen embryos (56 pp677-693). Several retrospective single-clinic studies from Canada, Ireland, and the USA, with subfertile couples receiving restorative reproductive medicine, mostly natural pro-creative technology, have reported adjusted cumulative live birth rates ranging from 29 % to 66 % for treatment for up to 2 years, with a mean women's age of about 35 years 58. It also reduces multiple pregnancy rates and has lowered the prematurity birth rate from 12.1 % to 7 % (56 pp747-773). This is also clear from the more recent study on NPT in Ireland (2018), which confirms that rates of prematurity and low birth weight among RRM live births are comparable to those of the general population of Irish women of all reproductive ages (Ireland's premature birth rate: 6 %, RRM rate: 5.5 %; Ireland's low birth weight rate: 6 %, RRM: 8.2 %) 53.
Multicenter prospective studies demonstrate that NPT is an efficient, less invasive, cost-effective holistic system of infertility treatment based on characteristics linked to successful NPT treatment 53,54,58,93,115,152-156.
The impact of "financial access" on infertility treatments is significant, with income and insurance coverage affecting couple's choices 157. IVF's high cost makes it inaccessible for many, but NPT provides a more affordable and effective alternative by addressing the root causes of infertility 158. NPT treats each woman's body uniquely to restore normal reproductive health, while IVF aims for pregnancy at any cost 153.
It is reasonable to assume that NPT will result in better pregnancy outcomes, such as a decreased risk of miscarriage, low birth weight, perinatal mortality, and low prematurity rate, and there are no frozen embryos 55,153. The primary difference between ARTs and NPT approaches to infertility is a commitment to exhaustively identify and treat the underlying correctable causes of infertility to enhance the probability of conception in vivo115. The biomarker monitoring of the CrMS guides the treatments used in NPT, including standard fertility medications and surgeries, and its response is assessed objectively by luteal hormonal testing 154. RRM focuses on correcting recognized abnormalities in reproductive physiology before conception to ensure proper ovarian hormone production, successful ovulation, and high-quality cervical mucus formation to aid sperm transport 53. NPT offers several advantages, such as medical safety, accuracy, personalization, respect for a woman's natural cycle, preservation of dignity and marital integrity, respect for women's health, and active participation from both spouses 116. Consequently, because it reduces risks and promotes conception while preserving intimacy and personal dignity, it is a morally and medically sound alternative to ARTs 115.
5.2 Reaffirmation of the Human and Christian Value of Adoption
We must reaffirm the human and social-religious value of adoption rather than encouraging the new advanced reproductive technologies, which can result in genetically related children with severe psycho-physical and social harms. The Church supports adoption as a wonderful way to build a family, so this process can be completed in ways that respect the dignity of everyone involved (143 n13,159 p140). As Christians, we have to appreciate this, as we are all sons and daughters of God by adoption (Cf. Gal 4:5). Adoption is a natural Christian choice for ARTs because adoption is a gift to the child who receives a new family and to parents who want a child (160 p209). Adoption benefits society by contributing to a culture of life in which the inherent dignity of every child is recognized 161. Adoption is often a complex and bureaucratic process, but many children need homes. So we should do our best to better the adoption of children, with correct laws and absolute control to avoid misuse regarding it 162.
5.3 The Church on Its Way to Dynamic Compassion
According to the Catholic Church, the essentials of fruitful married love are openness to new life and the willingness to beget and raise children together (CCC 1664) (132 n.1). Many couples who desire children are facing challenges, highlighting the Church's role and urging for significant attention to address this sensitive issue. In our pastoral accompaniment, we must provide holistic care that not only addresses the psychological, social, and cultural needs of individuals but also their religious and spiritual needs. While educating that children are "the blessing" in the sacrament of marriage, we should disseminate the gospel to those afflicted that fruitfulness is also a part of a blessing, even in the face of infertility 163. Then education can bring enlightenment and hope to those afflicted. Thus, as the mother embraces the child, the Church as a mother 164 should be able to keep and console the childless couples within her protecting arms. This care should have to start with the marriage preparation. To be effective, marriage preparation needs to include education about sterility, infertility treatment, and alternative parenting by adoption.
Many couples do not know whom to talk to about their suffering. Due to the close association between infertility and sexuality, it will be uncomfortable to discuss or disclose personal information about sexual behavior concerns. Infertile couples often experience emotional distress and fear, necessitating the Church to grasp the gravity of the experience to go a long way to accompany them sensitively and persistently. Active listening with confidentiality is an essential element in the pastoring of infertile couples. It shows the need for infertility counseling centers that may provide a more holistic approach to infertility and assist couples in better coping with their experience. Since it is priests who first encounter infertile couples seeking counsel, they need to know where to refer them, in addition to offering basic counseling. There is an urge call for all the diocesan bishops to ensure that all priests in the diocese are well informed about the Church's teaching about the ARTs. Pastoral awareness is so crucial in dealing with infertility families seeking medical advice or treatment, as it helps them understand their specific challenges, provides safe, morally acceptable medical remedies, and offers them hope for their journey. The Church must assist the couple in coping with the infertility crisis by facilitating community connection. The bishops should organize a gathering in both dioceses and at the parish level for those facing the same issue to discuss their struggles and ethical concerns. It is necessary to incorporate policies in the diocesan pastoral planning that directly or indirectly address the pastoral needs and cares of infertile couples. There is a need for a new pastoral approach to families to overcome the challenges facing families today, with two clear goals: helping them grow in love and overcome problems and difficulties (132 n211).
NPT, a restorative reproductive healthcare approach, is often overlooked in traditional medical school curriculums, limiting access for many women and couples 165. The Church's global presence in healthcare services can serve as a platform to educate and promote non-invasive medical options, including microsurgery and natural procreative technologies. The Church never fails to educate the people on the advantages of Catholic treatment options with moral acceptance, offer medical safety, promote shared responsibility, strengthen marriage, educate women on body knowledge, and address infertility causes while respecting human dignity. In parallel to the path of explaining the adversities of ARTs, it should accomplish its task to confront the reality of barrenness as a Godly call and entrustment rather than as a punishment. The church should take its twin role in enlightening and awakening the childless ones with opportunities to be generative towards society in the name of Christ and his great call on them. According to the Instruction for the Human Life, "spouses who find themselves in a particular way in the Lord's cross are the source of spiritual fruitfulness" (120 IIB n8). Like suffering, infertility also had specific significance and value from human and Christian perspectives. According to Familiaris Consortio, the situation of infertility provides a unique chance to serve God and mankind via compassion:
It must not be forgotten, however, that even when procreation is not possible, conjugal life does not, for this reason, lose its value. Physical sterility, in fact, can be for spouses the occasion for other important services to the life of a human person, for example, adoption, various forms of educational work, and assistance to other families and to poor or handicapped children. (166 n.14)
An infertile couple must recognize their vocation to become instruments of God for the service to the Church and humanity and thus assume spiritual parenthood (167 p27). So, by assuming their spiritual parenthood, the service will channel their suffering. Here, we must note that society, including the Church, must offer comprehensive psychological support to safeguard the human dignity and physical and psycho-social well-being of the infertile couple (168 pp120-122,169 p1301).
Thus, the dynamic perspective of compassion as a habitus, rather than a theoretical construct, includes a desire to alleviate the pain of others, the ability to act on behalf of others, and a commitment to sustaining engagement with others' suffering with solidarity 170. Above all, for the actual lending of hands to the situation of childlessness, the Church should be able to admit that if the followers take its advice and avoid modern fertility solutions that contradict Catholic teaching, then they are equivalent to being nailed to the Cross of Calvary without bloodshed. If so, the Church should be Mother Mary, who stood close to the cross.
CONCLUSION
Providing pastoral care to infertile couples is a multifaceted issue involving biological, psychological, therapeutic, and ethical dilemmas that can threaten individual, marital, family, and social stability. The Church, society, and family members must be empathetic companions, accompanying couples with support and guidance on their journey, providing other safe medical remedies that are morally acceptable, and offering them hope. The Church must be dynamic in its compassion, as outlined in the Encyclical Humanae Vitae, which plays a crucial role as both mother and teacher, providing love, care, and proper guidance with clarity to self-empowerment and self-worth in their journey towards parenthood. Infertility does not limit marriage but encourages fruitful partnerships by assuming spiritual parenthood. Couples carrying the cross of infertility serve as witnesses to Christ's "great mystery" through their fidelity and courageous discernment. The Church's advocacy for the culture of life inspires and motivates couples, and the problem of infertility is seen in the integral vision of man, both in his natural and supernatural vocation.