Introduction
Currently, the World Health Organization (WHO) defines cardiovascular diseases (CVDs) as a group of cardiac and blood vessel disorders 1 constituting one of the main causes of morbidity and mortality worldwide in the group of chronic non-communicable diseases (CNCDs) 2.
In April 2021, during the socialization of the Global Health Status Report, the WHO documented that CNCDs represented approximately 71 % of the total number of deaths in the world, a worrisome situation considering the comparison of this phenomenon ten years ago, as this cause of death only represented 63 % in 2011. In addition, this report emphasizes that, among CNCDs, CVDs caused 55.24 % of deaths in the age groups of adults and older adults 3.
This becomes a public health problem and a risk to comply with one of the targets established in the Sustainable Development Goals regarding a maximum 33 % reduction in the number of premature deaths due to CNCDs by 2030 4.
These diseases disproportionately affect middle- and low-income countries when compared to high-income ones, as their onset is associated with factors such as globalization (integration of external habits from one country to another), unhealthy ways of living and eating habits, population aging and rapid unplanned urbanization, all associated with harmful health habits such as sedentary lifestyles 5.
At the World Economic Forum, the economic wear out that CVD development causes in the countries was evidenced, describing that the losses in middle- and low-income countries were over US$ 3 million for 2010 and that they are projected at US$ 8.6 million for 2030 6, which affects the direct and indirect cost estimations due to CVDs in the world, making them rise from US$ 863,000 million in 2010 to US$ 1,040,000 million for 2030.
In the United States, according to the summary of heart diseases statistics published in 2021, approximately 2,200 people die due to CVDs every year, which represents one out of three deaths in the CNCD group; however, there is an additional problem as around 90 million Americans live with some type of CVD or their sequelae 7.
The National Observatory belonging to the Colombian National Health Institute established that CVS represented the leading cause of death in the group of CNCDs in the country. In 2019, CVDs were the trigger for 69 % of all deaths, and a 15 % increase was projected for the 2010-2020 period, which would total 73 % and 60 % of the mortality and morbidity burdens, respectively 8. This generates disability life years in people, as the Colombian female and male populations currently hope to live a mean of 76.1 and 70.6 years, respectively, of which 18.2 and 17.8 years will represent disability life years, mostly secondary to CNCDs, with a significant percentage corresponding to CVDs 9.
In Colombia, the proportion of deaths due to the CVD group is as follows: 30.6 % for stroke; 0.5 % for chronic rheumatic heart disease; and 12.4 % for hypertension, whereas the highest percentage (56.3 %) corresponds to ischemic heart disease 10. This shows the need to interact with patients with ischemic heart disease, defined by the WHO as blood vessel narrowing or blockage 11, with two presentations: a chronic and stable clinical condition and another acute (Acute Coronary Syndrome or ACS), which requires specific clinical management and treatments, mainly angioplasty and coronary bypass 12.
In addition, it is not only necessary to discard mortality based on ischemic heart disease but it is also important to mention the high rate of sequelae that may be developed in people who suffer or have suffered the illness, the reason why it is opportune to address these patients since they cardiovascular rehabilitation. This concept emerges now as the result of years of observation and evidence that began in 1957, when Hellerstein and Ford 13 spoke for the first time about cardiac rehabilitation and its components, followed by the WHO in 1963, which defines it as “the set of necessary activities to ensure optimum physical, mental and social conditions for people with CVDs, allowing them to occupy by their own means the most normal place in society as they can” 14.
Based on the aforementioned, the Revista Uruguaya de Cardiología15 describes the phases of cardiac rehabilitation programs: the first one, known as the hospital period, takes place during the patient’s admission to the care center, in the acute stage of the disease or decompensation. Their main difficulty is that the hospitalization periods are increasingly shorter, impairing actions in this stage.
The second phase (Active or Outpatient Rehabilitation) encompasses the 2-3 first post-discharge months, after the initial effort test, and is performed in hospital units or heart centers according to each patient’s baseline risk; this is the best moment to counsel on adequate control of the risk factors.
The third phase (Maintenance) is limited in terms of duration and is usually conducted at the patient’s homes, either in heart centers or duly equipped gyms. The main objective of this phase is to keep the patients motivated to continue practicing the healthy lifestyles acquired 15.
As stated by the Inter-American Cardiology Society, the South American Cardiology Society and the Cardiovascular Prevention and Rehabilitation Inter-American Committee in the Consensus on Cardiovascular Rehabilitation and Secondary Prevention of the Inter- and South American Cardiology Societies16, cardiac rehabilitation programs are essential in the secondary prevention axis for cardiovascular events, as their objectives are targeted at assisting patients at a high risk of developing coronary diseases, comprehensively rehabilitating them and educating them so that they maintain healthy habits, as well as to prevent cardiovascular events and ensure adequate control of the risk factors.
These programs are designed to limit the physiological and psychological effects of heart diseases, mainly reducing the sudden death risk based on controlling cardiac symptoms, stabilizing or reverting the atherosclerotic process and increasing the psychosocial well-being state 17, defined by the WHO as the well-being condition in which a person can put their capabilities into practice and can face normal life-related stress, as well as to work productively and contribute to their community 18. A Cardiac Rehabilitation Program (CRP) is characterized by interdisciplinary and structured management, adequate prescription and monitoring of physical exercises, and education, follow-up and motivation of the patients for them to sustain healthy habits and adhere to the treatment 19.
Organizations such as the American Heart Association 20 and the American Cardiology College 21 agree upon the importance of CRPs and recognize them as an essential part of the care of cardiovascular patients, the reason why they are recommended as useful and effective (Class I). On the other hand, the consensus achieved between the Pulmonary and Cardiovascular Rehabilitation American Association, the Agency for the Medical Care Policy and the American Heart Association established that to comply with the objectives of creating these programs, they should be offered in a multifaceted and multidisciplinary fashion, carrying out interventions targeted at reducing cardiovascular risk, so that they not only offer physical training but also educational interventions 22.
The evidence shows that these programs have proven to reduce mortality by 20 % to 25 % among patients who have suffered an Acute Myocardial Infarction, lowering the number of re-infarctions 23; in addition, they have also proven to reduce the rate of major cardiovascular events after performing coronary angioplasties 24. In patients with heart failure, they have also shown efficacy both in achieving a reduction in terms of mortality and in reducing the number of hospitalizations 25.
Consequently, this review gains importance in searching scientific literature in Spanish with a suitable information validation process, which includes studies assessed based on their methodological quality to have the best available evidence and contribute to reinforcing how people with CVDs are intervened on. Based on this, it is possible to document the information regarding the effect of these educational interventions, so that the phenomenon can be known in depth and strategies can be devised for patients undergoing rehabilitation processes. Given the above, the following research question emerges: What is the effect of educational interventions during cardiac rehabilitation to foster health in patients with ischemic coronary disease?
Materials and methods
A systematic review was conducted in the PubMed, SciELO, LILACS, EBSCO, MEDES, CUIDEN, Dialnet, ScienceDirect and CUIDATGE databases, with no restriction in terms of results. To create the search equations, the words ‘rehabilitación cardiaca, enfermedad cardiovascular and intervención educativa were used, which were combined with the AND Boolean operator for the setup and adapted to the English and Portuguese languages, as follows: ‹cardiac rehabilitation‹ / ‹reabilitação cardíaca;’ ‹cardiovascular disease› / ‹doença cardiovascular;’ and ‹educational intervention› / ‹intervenção educativa.’
The bibliographic search was scheduled between February and September 2022, considering the protocol established in the PRISMA statement 26, which serves as a guide to provide information on how the question is formulated, data extraction, quality of the studies and risks of bias in systematic reviews. In addition, the project was registered in the Prospero database 27 (CRD42023398444). The results were extracted, selected and analyzed in October and November 2022; this phase was performed by implementing a blinded evaluation in charge of the lead and deputy researchers.
Table 1 Inclusion criteria
| Participants | Patients with ischemic heart disease who underwent cardiac rehabilitation. |
| Result measures | Physical, psychological or social clinical evaluations in the patients after cardiac rehabilitation. |
| Comparison | Conventional cardiac rehabilitation interventions versus Conventional cardiac rehabilitation interventions + Additional educational project. |
| Intervention | Educational strategies used during cardiac rehabilitation in patients with ischemic heart disease. |
| Language | Publications in Spanish, English, and Portuguese. |
| Design | Randomized controlled trials or clinical trials investigating an Experimental Group and a Control Group. |
Source: Prepared by the authors.
Studies published in the last ten years (2011-2021) were selected for the analysis to have updated scientific literature, considering that the concept of cardiac rehabilitation as known today was started to be worked on at the end of the 1970s; however, forty years after being implemented, underutilization of this service was described and, during the period selected, the patient’s adherence and the professionals’ interest in showing the benefits referring to the topic were evidenced.
The studies included had to be quantitative, of the experimental or quasi-experimental type, and assess the effectiveness of the cardiac rehabilitation educational interventions in patients with ischemic heart disease. The studies had to be in full-text format, although sample size and/or number of interventions were not considered to select the articles. The materials excluded from the review were studies belonging to the Gray Literature and/or systematic reviews, as well as those that presented a rating below 3 according to the Jadad scale 28, which allows for evaluating the methodological quality of clinical trials based on criteria described in the articles’ methodological section.
The first step for their selection was to read titles and abstracts; subsequently, duplicate texts were removed, and the articles were read in full. Finally, the Jadad scale was applied to assess their quality and mitigate possible methodological and/or publication biases, a procedure with which the randomization criteria for the participants’ allocation and their losses and withdrawals were evaluated and scored, assigning these values: 1, 0 or -1. Based on the sum of all five criteria, if the score is greater than 3 it can be inferred that the methodological quality is optimal Figure 1).
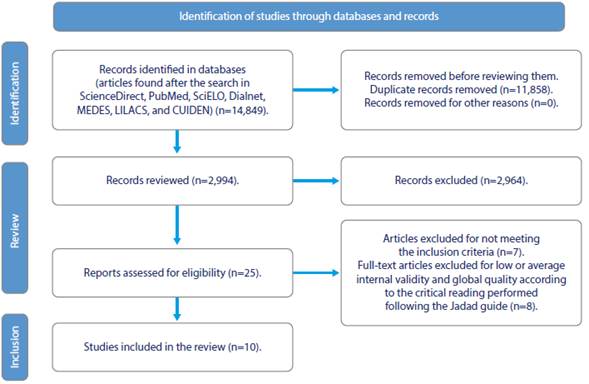
Source: Prepared by the authors based on the PRISMA statement guide.
Figure 1 Article Selection Process: Identification, Selection, Analysis, and Inclusion
Of all 25 full-text articles assessed for eligibility, 7 were removed after full-reading for not meeting the inclusion criteria; the remaining 18 were submitted to bias and methodological quality assessments using the Jadad scale, from where it was observed that 8 studies were of low methodological quality (1 point each), thus being excluded, with a total of 10 studies remaining to prepare the narrative synthesis table corresponding to the selection.
The data extracted were stored in a Microsoft Excel spreadsheet where the population characteristics, the type of intervention, the randomization procedure, the results of the intervention and the follow-up performed in each study were described. Finally, the authors adhere to the ethical criteria and responsibilities outlined in Resolution No. 8,430 of 1993 by the Colombian Ministry of Health 29, which categorizes this study as no-risk research, in addition to stating that no experiments with human beings or animals were conducted in this survey. Regarding data confidentiality, no personal identification data from the patients are included in this article.
The analysis unit derives from the findings in the publications and, for that purpose, aspects referring to quality of life, selfefficacy, anxiety and depression were observed, in addition to biomarkers (lipid profile, weight, hospitalizations due to cardiovascular reasons during the study period). The descriptive statistical analysis was based on frequency, mean and standard deviation tables, and only two articles presented variance and covariance results.
Results
Regarding the general characteristics of the studies, they were randomized clinical trials from the methodological point of view. Regarding the loci, the studies were developed in different world areas, the reason why four of all ten articles are from Latin America and the Caribbean (Brazil, Chile, Cuba) and one article from North America (Canada) was selected, as well as two studies from the European continent (Spain and Germany), another two from Asia (China and India) and one from Oceania (Australia) (Figure 2). Referring to the year of publication, it is evidenced that most of the articles (three) were published in 2014, followed by two in 2020 and one in 2011, 2016, 2017, 2018 and 2021. Finally, in terms of language, all the articles selected are written in English (Table 2).
Table 2 Narrative Synthesis Corresponding to the Selection
| Article | Main author - Year of publication - Country - Language | Methodological quality assessment Jadad | Analysis | Method |
|---|---|---|---|---|
| Berenguel et al, 2017, Spain 30 | 1 | Excluded. | Does not apply. | |
| Martínez et al, 2015 31 | 1 | Excluded. | Does not apply. | |
| I | Frederix et al - 2016 - Spain - English 32 | 3 | Selected. | Multicenter, prospective, and randomized and controlled clinical trial. |
| II | Furuya et al - 2014 - Brazil - English 33 | 3 | Selected. | Randomized controlled clinical trial. |
| De Melo et al, 2015, Canada 34 | 2 | Excluded. | Does not apply. | |
| De Melo et al, 2015, Canada 35 | 2 | Excluded. | Does not apply. | |
| III | Lumertz et al - 2014 - Brazil - English 36 | 3 | Selected. | Randomized controlled clinical trial. |
| Widmer et al, 2017, USA 37 | 2 | Excluded. | Does not apply. | |
| Naranjo et al, 2012, Colombia 38 | 2 | Excluded. | Does not apply. | |
| IV | Hwang et al - 2017 - Australia - English 39 | 3 | Selected. | Parallel non-inferiority trial of two groups with blinded result evaluators. |
| V | Peng et al - 2018 - China - English 40 | 3 | Selected. | Randomized controlled clinical trial. |
| VI | Stoevesandt - 2020 - Germany- English 41 | 3 | Selected. | Randomized controlled clinical trial. |
| VII | De Melo et al - 2020 - Canada - English 42 | 3 | Selected. | Multicenter trial. |
| VIII | Guerra et al - 2011 - Cuba - English 43 | 3 | Selected. | Randomized controlled clinical trial. |
| IX | Brevis et al - 2014 - Chile - English 44 | 3 | Selected. | Randomized controlled clinical trial. |
| X | Arjunan et al - 2021 - India - English 45 | 4 | Selected. | Randomized controlled clinical trial. |
Does not apply: Excluded for not meeting the methodological quality criterion after applying the Jadad scale.
Source: Prepared by the authors based on the reviewed articles.
As for the sociodemographic data recorded in the articles, we found that the participants included in the studies were mostly male (60 %-70 %) and with average and high schooling levels; in terms of occupation, they were retirees (65 %) and assigned to phases II and III of the rehabilitation program; finally, regarding their age, the mean was 63 years old (Table 3).
Table 3 Characterization Regarding the Sociodemographic Data of the Selected Studies
| Age (Years old) | Gender | Connection to the rehabilitation program | ||||||
| Intervention | Control | |||||||
| Intervention | Control | ale | Female | Male | Female | Intervention | Control | |
| I | 62 | 63 | 86 % | 14 % | 79 % | 21 % | Phase II | Phase II |
| II | 63 | 60 | 60 % | 40 % | 53 % | 47 % | Phase II | Phase II |
| III | 60 | 60 | 56 % | 44 % | 41 % | 59 % | Phase II | Phase II |
| IV | 68 | 67 | 57.1 % | 42.9 % | 61.2 % | 38.8 % | Phase II | Phase II |
| V | 61 | 68 | 79 % | 21 % | 71 % | 29 % | Phase II | Phase II |
| VI | 62 | 64 | 80 % | 20 % | 75 % | 25 % | Phase I | Phase I |
| VII | 60 | 62 | 71 % | 39 % | 68 % | 32 % | Phase II | Phase II |
| VIII | 64 | 60 | 54 % | 46 % | 60 % | 40 % | Phase II | Phase II |
| IX | 67 | 68 | 72 % | 28 % | 49 % | 51 % | Phase II | Phase II |
| X | 63 | 64 | 52 % | 48 % | 65 % | 35 % | Phase II | Phase II |
| Mean | 63 | 63.3 |
Source: Prepared by the authors based on the articles reviewed.
The following inclusion criteria were established as requirements to participate in the studies: Voluntary participation of candidates for coronary angioplasty treatments: patients with ischemic coronary disease; and patients requiring rehabilitation programs, although not necessarily hospitalized. It was found that six studies 32,33,36,39,40,41 were developed in the Telemedicine modality, resorting to voice calls, text messages, own software programs and digital platforms for synchronous and asynchronous meetings. As for the participants’ allocation to the intervention or control groups, they were randomly assigned by professionals that would not develop any intervention directly with the participants.
Educational Interventions Implemented during Cardiac Rehabilitation
The educational interventions were developed during a mean of twenty-four weeks. According to the new technologies to implement the interventions, two sessions per week were conducted before applying the pre-test (baseline).
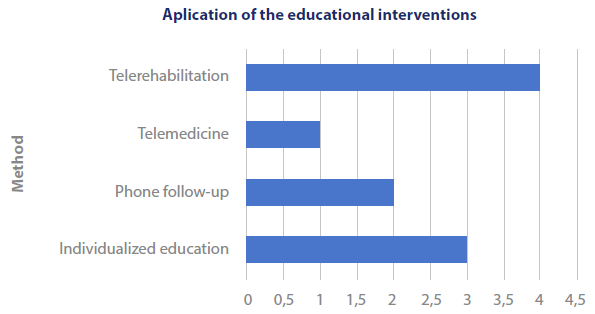
Source: Prepared by the authors based on the articles reviewed.
Figure 3 Method Used to Develop the Intervention in the Designated Group
The individualized education projects were designed to contribute to health literacy and self-management on the part of patients and family members, according to the needs detected during each patient’s initial evaluation when entering the program. Regarding the topics developed in the interventions, they were focused on surgical and pharmacological treatments, education on heart diseases, nutrition and healthy habits (such as smoking cessation, performing physical activity and weight control), wound healing and management, and the need to change life habits and cardiovascular risk factors.
The aforementioned allows for identifying the application of new technologies in the development of CRPs, which are of vital importance because they ease follow-up and development of educational interventions, contributing to ensuring their effectiveness when compared to traditional rehabilitation (Table 4).
Table 4 Synthesis of the Educational Interventions Implemented in the Selected Studies
| Article | Population | Intervention | Duration |
|---|---|---|---|
| I | 139 patients randomly allocated to two groups: Intervention (IG) and Control (CG). | CG: They took part in a conventional CRP. IG: They took part in a 24-week Telerehabilitation program based on physical activity Telemonitoring and Telecoaching on nutrition, healthy habits and physical activity from the sixth week onwards. | 24 weeks |
| II | 60 patients randomly allocated to two groups: IG and CG. | CG: They were offered education at discharge and took part in conventional control outpatient appointments. IG: They took part in an individualized educational program based on healthy habits, adherence to the treatment and education about the disease, by means of telephone follow-up. The program sessions were on the first, eighth and sixteenth week after hospital discharge. | 18 weeks |
| III | 74 patients randomly allocated to two groups: IG and CG. | CG: They were offered conventional medical follow-up and general and unstructured counseling on lifestyles. IG: They were offered individual counseling sessions for one year about CVDs, modification of risk factors, healthy habits and nutritional control; in addition, they received counseling once a month via telephone calls. | 12 months |
| IV | 53 patients randomly allocated to two groups: IG and CG. | CG: They were offered conventional follow-up with a CRP consisting of two sessions per week for twelve weeks. IG: They took part in a home-based Telerehabilitation program that included an additional physical exercise plan to be performed three times a week, plus education through a video call platform that favored two-way communication. | 24 weeks |
| V | 83 patients randomly allocated to two groups: IG and CG. | CG: They were offered habitual care, planned education before discharge and periodic follow-up visits. IG: They took part in a Telemedicine training program that consisted of a two-month intervention based on 32 physical training sessions with prior structured education on physical exercise, self-care and lifestyles, as well as on relevant aspects of coronary disease. | 16 weeks |
| VI | 260 inpatients randomly allocated to two groups: IG and CG. | CG: They were offered conventional follow-up with a CRP. IG: They had a device to receive and evaluate additional information about the prevention of CNCDs and coronary heart disease, their treatments, risk factors and lifestyles. After each session (8 in total), all made a brief assessment. | 3 weeks |
| VII | 162 patients that were CRP candidates in three health centers. | The participants were offered weekly classes of supervised physical exercises for 12-24 weeks, in addition to physical activity prescriptions for the other days of the week. Asynchronous classes were also taught via a website and a standardized guide for patients, although adapted to meet the participants’ needs regarding eating habits, risk factors and treatments for cardiac diseases. | 24 weeks |
| VIII | 20 participants with heart diseases, angina pectoris, acute myocardial infarction and hypertensive heart disease. | They attended a program in three phases. In the first phase, the learning needs were identified and the questionnaire was applied to assess the knowledge level before the intervention. The following variables were considered and categorized as adequate or inadequate: the concept of cardiovascular rehabilitation; risk factors; most frequent cardiovascular diseases; the influence of physical exercise on these pathologies, and treatment. | 16 weeks |
| IX | 63 patients randomly allocated to two groups: IG and CG. | CG: They were only offered habitual education before discharge. IG: They received an educational intervention targeted at Nursing care in cardiac rehabilitation. | 9 weeks |
| X | 200 patients with heart failure. | CG: They took part in a conventional CRP. IG: They took part in a structured educational program in charge of nurses, whose components included recommendations on diet, medication, physical exercise, weight control, smoking cessation, sodium restriction; and lifestyle changes. They were also shown an educational video for 5 days and subjected to telephone follow-up every 15 days for 6 months. | 24 weeks |
Source: Prepared by the authors based on the articles reviewed.
Impact of the Educational Intervention on the Patients’ Health after Rehabilitation
The effects or consequences after implementing the interventions targeted at the participants’ health evidenced a reduction in the number of rehospitalizations due to cardiac reasons, as well as a reduction in the days lost due to hospitalization related to these events; in addition, another favorable finding was the change in the cardiovascular risk factors (control regarding overweight, alcohol consumption, blood pressure, consumption of fats and sugars and smoking habit). Thus, the positive impact is not only denoted in the physical aspect; mental health was also favored, as the interventions contribute to strengthening it in aspects such as anxiety and depression reduction and management, as social and emotional support is found in CRPs.
However, these interventions fail to achieve changes in the New York Heart Association (NYHA) classification in the short-term 46. It is deemed relevant to note that, in the medium-term, the intervened patients achieve statistically significant improvements in the assessment corresponding to the Framingham criteria (Table 5).
Table 5 Synthesis Regarding the Impact of the Educational Interventions during Cardiac Rehabilitation
| Article | Effect |
|---|---|
| I | One year after participating in the intervention, the number of rehospitalizations due to cardiovascular reasons was reduced in the Intervention Group when compared to the Control Group (7:13); likewise, improvements in the number of days until the first rehospitalization were found (502:445), as well as in the hospitalization times. The mean hospital care cost was lower in the Intervention Group; in addition, significant improvements were found in this group. Finally, the profitability analysis showed that adding Telerehabilitation to the CRP in the centers (Intervention Group) was both more economical and effective than cardiac rehabilitation based on the center alone (Control Group). |
| II | The result corresponding to the perception of the health status between the groups was not statistically significant at baseline (when initiating the intervention); however, once the intervention was concluded, the Intervention Group presented improvements in the social functioning domain and the role of emotions. Referring to self-efficacy, no statistically significant differences were found. In terms of anxiety, a reduction was found over time in the Intervention Group when compared to the Control Group. Both groups presented high adherence to medication. A statistically significant group-by-time interaction effect was observed for anxiety (p=0.04), which was reduced over time in the Intervention Group but was increased in the Control Group. |
| III | When the patients’ participation in the Intervention Group was ended, a 1.7-point reduction was evidenced in cardiovascular risk, as well as a 1.2-point increase in the Control Group, both calculated according to Framingham’s risk score. As secondary results in the Intervention Group, improvements were found in the laboratory parameters (lipid profile, glycated hemoglobin and glycemia), as well as in the anthropometric measures, especially weight. Both groups presented high adherence to medication, although it was more predominant in the Intervention Group. |
| IV | At the cutoff moments of the evaluations made, it was found that there were no statistically significant differences between the groups at weeks 0 and 24 in relation to aerobic exercises, as well as for other functional measures, such as balance, strength, quality of life and urinary incontinence. However, during the evaluation at week 12, a difference in favor of the Intervention Group was evidenced in physical exercises. |
| V | Statistically significant differences were found between the groups: the quality of life score assessed increased over time, achieving a sustained improvement after four months of the intervention; likewise, the functional physical exercise capacity increased in the Intervention Group, with no adverse events. Referring to anxiety and depression, no interactions or significant changes were found between the intervention and control groups, as was the case of heart rate, of the New York Heart Association classification, and of the left ventricular ejection fraction, where no significant changes were detected. Finally, it was concluded that the educational intervention is a feasible and effective method that improved the quality of life and functional capacity for physical exercise in the patients intervened. |
| VI | A significant short-term effect on learning about the disease was observed in the Intervention Group. In the long-term, no relevant statistical significance was found regarding learning ability in the groups. Finally, it was concluded that, although no statistical significance was found in any of the observations, a positive short-term effect was in fact identified on the learning ability, as well as positive trends in physical and mental health after the patients’ discharge, post-intervention. |
| VII | Regarding physical activity, the mean number of steps walked per day increased significantly over time (p<0.001). In turn, regarding food intake, there were important differences in the scores over time (p<0.001), with more participants adhering to the Mediterranean diet; in addition, a significant improvement was recorded in the physical exercise self-efficacy score (p<0.001). Once the intervention was concluded, a significant improvement was found in the patient’s general knowledge in relation to food intake, self-efficacy and physical exercise; in addition, the results showed a significant and positive correlation between knowledge after the intervention, food intake and self-efficacy. On the other hand, schooling level and prior knowledge exerted an influence on the subsequent changes. |
| VIII | The participants significantly improved their knowledge about cardiac rehabilitation, modification of risk factors and the importance of physical exercises. In general, before applying the educational program there was predominance of inadequate knowledge about the treatment among the patients with CVDs (14, 70.0 %); however, after the program, it was corroborated that 17 patients (85.0 %) had properly acquired such knowledge. |
| IX | In this research it was possible to evidence that, followed by an evaluation at one and three months, the educational intervention generated changes in the modifiable risk factors, which were associated with better lifestyles. Significant differences were found between the intervention and control groups in weight, waist circumference, BMI and systolic blood pressure among the female patients, whereas these differences were only observed for weight, BMI and waist circumference among the male patients. Referring to the smoking habit, alcohol consumption and physical activity, statistically significant differences were found for tobacco and physical exercises. |
| X | When evaluating adherence efficacy, it was found that the mean difference between the intervention and control groups before the test was 0.680 (p<0.002). Post-test 1 and post-test 2 presented a high mean difference (0.830 [p<0.001] and 0.876 [p<0.000], respectively) between the intervention and control groups. The mean scores in the pre-test (y=3.01±1.381), post-test 1 (y=3.89±1.83) and post-test 2 (y=4.18±1.041) were statistically significant for the Intervention Group (p<0.004) when compared to the Control Group (y=2.39, y=3.1 and y=3.3). In the Intervention Group, adherence to cardiac rehabilitation showed a statistically significant increase after the educational program interventions, as well as improvements in terms of health actions and behaviors. |
Source: Prepared by the authors based on the articles reviewed.
Discussion
Through this systematic review, it was possible to identify the effect of educational interventions on patients with ischemic cardiac disease undergoing rehabilitation, considering that this program is targeted at reducing morbidity and mortality with this type of intervention.
After the review that was conducted, it was possible to find the necessary documentation in the updated scientific literature to fully meet the objective proposed, which was defining the impact of educational interventions on fostering the health of cardiac rehabilitation candidates or patients undergoing it, thus identifying how favorable it is to early address this type of patients, due to the positive changes reflected in their health.
The heterogeneity of the studies selected stands out among their characteristics, implying significant demographic and social changes in the study populations, which can have significance in the results, mainly when characterizing the populations. Eventually, the studies that contributed to documenting the systematic review came from various countries, with Brazil, Spain, Australia, China, Germany and Canada among them, which present different population typologies implying heterogeneous habits and lifestyles across the populations; however, all conclude on the effectiveness of the interventions and the benefits they reflect on the health of the patients addressed.
In their study, Roldan et al. pointed out similar results referring to the psychological, emotional and attitudinal changes described in the current systematic review. Regarding the knowledge about and behavior of the patient’s cardiovascular risk factors, mild levels were found in the first measurement and considerable improvements were shown after the educational intervention. The patients’ healthy lifestyles also improved after the intervention 47. These findings emphasize the importance of educational interventions in reducing CVD modifiable risk factors.
In opposition to what has been mentioned in this article, Mora et al. describe that 26 % of the study population intervened on presented some angina episode in the initial assessment to enter the cardiovascular rehabilitation program and that 15% of them did not require any type of treatment, whereas 5% had rehospitalizations 48.
Regarding the effect of the interventions, Brevis et al. 49 concluded that, despite the good results of the educational interventions, the basic principle that continuous contact is required to achieve lifestyle changes is confirmed, which is similar to what was found in this study; in addition, it allowed establishing that there is no need for a specialized center to apply rehabilitation programs to coronary patients, arguing the need to incorporate them already in Primary Care.
Among the aspects to note, the support offered by the new technologies (Telemedicine, Tele-education, and Telemonitoring) turns out to be beneficial in the patients’ follow-up and, for Ibáñez et al. 50, they contribute to improving healthcare processes. In turn, Stanberry 51 argues that Telemedicine offers unique opportunities both for patients and for health professionals, which is evidenced in the results of applying this care method while the educational interventions are developed; however, it is noted that this occurs when the method is implemented as a direct response to clear clinical needs.
The strengths of this systematic review lie first and foremost in recognizing the effect of educational interventions on improving the health of patients with ischemic coronary disease undergoing cardiac rehabilitation, considering that no research studies of this type referring to the theme addressed were found in the literature.
Likewise, knowing the educational interventions, their design towards cardiac rehabilitation and their effectiveness allows for improving Nursing performance when managing these patients; in addition, it represents a reference point to continue implementing strategies and new effective interventions in the treatment of these ever-increasing pathologies.
The literature review yielded a limited number of studies; however, the methodological quality assessment allowed for selecting the most adequate materials in terms of methodological design to reduce biases. According to this, this research becomes an input for the Nursing discipline and the scientific community in general, so that decision-making in the management of people with cardiovascular diseases can be improved.
Even if the results of this research meet the objective proposed, it is important for future surveys not to limit the search to the English and Portuguese languages but that more languages can be added; in addition, it is recommended to conduct a scoping review that allows including other types of designs, especially around the users’ perceptions and experiences.
Conclusions
Based on the systematic review of the scientific articles about the effect of educational interventions for cardiac rehabilitation on patients with ischemic coronary disease, it is concluded that such interventions improve quality of life, reducing morbidity and rehospitalizations in people with this background; however, in terms of anxiety and depression symptoms and self-efficacy, there is no significant statistical evidence showing how educational interventions can modify these aspects in the short-term.
The most outstanding effect exerted no impact on the participants’ health conditions but it was framed on the improvement of the patients’ general knowledge about ischemic coronary disease, cardiac rehabilitation and lifestyle changes, showing that the patients’ rehabilitation process is fundamental when it comes to fostering cognitive strengthening that favors the behavioral approach required to correct the risk factors.
It is important to note that, although statistically significant changes were evidenced in all the studies in terms of the knowledge acquired after the intervention, they would only be in the short-term and the initial effect is lost in subsequent evaluations without new interventions; the exact opposite occurs concerning adherence to medication, which is maintained over time.
There is scientific evidence of high methodological quality around the effectiveness of the educational interventions in this review, which allows health professionals to propose actions since the cardiac rehabilitation initial phases that contribute to empowering patients in their recovery and in changing unhealthy habits.
Although it was shown that educational interventions improve the health of people who have suffered ischemic coronary disease, it is necessary to continue conducting research studies in this line, as the number of papers found was limited. This strategy will allow for strengthening Nursing professionals’ work, as they will have scientific evidence for decision-making.
















