Introduction
Type 2 diabetes mellitus (T2DM) represents a public health problem due to its high prevalence, mortality, and morbidity rates, with a resulting increase in costs for the healthcare system. All these negative health outcomes, both at the individual and collective levels, prompt the development of innovative strategies to promote effective self-management (1).
Thus, certain decisions in therapeutic management have an impact on the quality of life of people with T2DM since many of the complications progress to disability. Furthermore, the treatment of complications leads to higher costs, both for the individual and the healthcare system (2). For this reason, the guidelines of scientific organizations dedicated to the study of T2DM recommend that people should participate in education programs for diabetes mellitus self-care (EPDMS). These programs train individuals so that they become knowledgeable enough to make decisions and, simultaneously, induce self-management (3). EPDMS thus benefit and improve this population’s health conditions (4).
Self-management is defined as the individual’s ability, alongside their families, community, and healthcare professionals, to manage the symptoms, treatment, and psychosocial, cultural, and spiritual changes resulting from chronic conditions. For this purpose, the processes related to self-management include goal setting and self-monitoring, reflective thinking, decision-making, planning and engaging in specific health behaviors, self-assessment, and management of physical, emotional, and cognitive responses regarding health behavior changes (5).
One of the ways to support self-management is by adopting the perspective of social support. Social support is a care network provided by people who are close to an individual or professionals, regardless of where they receive treatment. This form of support provides knowledge and affection, which enables learning, security, and improved self-esteem. These feelings contribute to the continuity of activities regularly, leading to the individual refraining from quitting treatment or withdrawing from society (6).
Those who receive and, especially, perceive the social support provided by their support network can face these adversities with more commitment since they know who to resort to and from whom to receive the necessary help. This helps them to self-manage a pathology’s treatment, emphasizing that this is a delicate period, with individual adaptations and resignations (7). From this perspective, interventions based on social support are capable of modifying health conditions, because they reduce the individual’s mental and physical stress, as well as reducing behaviors that are harmful to their health (8).
According to the literature, nursing stands out as the profession best suited to provide self-management support, since its importance lies in the fact that it strengthens the bond for treatment, with knowledge and planning of routines to manage a chronic condition (9). In this sense, specific programs led by nurses that offer social support to teach self-management skills stand out (9). Thus, it is necessary to learn more about nurse-led programs that aim to promote self-management through social support in the field of T2DM, since there is currently a lack of information available on their characteristics. Furthermore, understanding these programs’ current state of the art would be useful for informing future research.
Additionally, nursing interventions focused on social support to help the self-management of patients with T2DM contribute to the health-disease process in a way that enables them to manage their health condition. Consequently, it is necessary to carry out this scoping review to synthesize the current scientific evidence on the subject.
The main objective of this review is to map the nature and extent of published scientific production and grey literature related to nurse-led programs aimed at supporting self-management of care of people with T2DM through social support. It has the following specific objectives: To list the programs focusing on social support for people with T2DM led by nurses; to describe the contents of these programs; and to identify the results related to them.
Materials and Methods
This is a scoping review, whose purpose is to map, explore, and describe the literature in the research field and the conceptual limits of the theme addressed. It was done by observing the methodological guidelines of the Joanna Briggs Institute (JBI). Thus, the following steps were followed, according to the Preferred Reporting Items for Systematic Review and Meta-Analyses extension for Scoping Reviews (Prisma-ScR) version 2020: defining and aligning the objectives and questions; developing and aligning the inclusion criteria with the objective and guiding question; describing the planned approach for searching for evidence, selecting and extracting data, and presenting the evidence; searching for the evidence; selecting the evidence; extracting the evidence; evaluating the evidence; presenting the results; summarizing the evidence about the review’s purpose, establishing conclusions, and noting any implications arising from the findings (10).
Registration Protocol
The protocol for the preparation of this review is registered on the Open Science Framework (OSF) platform and can be accessed via the following link: https://osf.io/4wvt6.
Identification of the Guiding Question
The guiding question formulated was the following: What nurse-led programs exist to support self-management in people with T2DM through social support, and what are their characteristics?
Furthermore, the PCC (population, concept, and context) mnemonic strategy was used to integrate the studies in this review. Therefore, the population consists of adults with T2DM; the concept of nurseled social support programs; and the context is primary healthcare or the community.
Eligibility Criteria
The eligibility criteria adopted were: studies published with the proposed theme in English, Spanish, and Portuguese; complete articles, theses, and dissertations available online; any study, regardless of methodological design (qualitative, quantitative, or mixed), that explores the participant’s experience in programs aimed at supporting the self-management of DM through social support and led by nurses; studies with participants aged 18 or over, diagnosed with T2DM, conducted in the primary health care setting, and with program interventions led by nurses.
Search Strategy
The search for studies was performed in the following databases: Web of Science, Medline (PubMed), Cinahl (EBSCO), Capes Catalog of Theses and Dissertations, Scopus, JBI Evidence Synthesis, PsycINFO (APA), and Open Access Scientific Repositories in Portugal between February 23 and March 17, 2022. Afterward, the reference lists of the included studies were manually searched to identify any relevant studies. The search strategies used for each database are shown in Table 1 and were devised with the assistance of two librarians with expertise in the health field and systematized reviews.
Table 1 Search Strategies Used in the Explored Databases. Brazil, 2022
| Database | Search Strategy | Search Date | Retrieved Articles |
|---|---|---|---|
| Cinahl (EBSCO) | ((MM “Self Care”) OR (MM “Self-Management”)) AND (MM “Support, Social/UT”) AND (MM “Community Programs”) AND (MM “Nurses”) AND (MM “Diabetes Mellitus, Type 2”). | 17/03/2022 | 11 |
| Open Access Scientific Repositories of Portugal (RCAAP) | “Social support” AND diabetes | 17/03/2022 | 181 |
| Web of Science | (“Self Care” OR “self management”) AND (“Social Support” OR “Social Care” OR “Online Social Support” OR “Perceived Social Support” OR “Perceived Social Supports”) AND (“nurse-led education” OR “nurse- delivered intervention” OR “nurse-led intervention” OR “program development” OR “nurse-led program”) AND (“diabetes” OR “diabetes mellitus” OR “diabetes mellitus, Type 2” OR “Diabetes Mellitus, Type II” OR “Type 2 Diabetes Mellitus” OR “Type 2 Diabetes” OR “Diabetes, Type 2”) | 23/02/2022 | 3 |
| Scopus | (“Self Care” OR “self management”) AND (“Social Support” OR “Social Care” OR “Online Social Support” OR “Perceived Social Support” OR “Perceived Social Supports”) AND (“nurse-led education” OR “nurse- delivered intervention” OR “nurse-led intervention” OR “program development” OR “nurse-led program”) AND (“diabetes” OR “diabetes mellitus” OR “diabetes mellitus, Type 2” OR “Diabetes Mellitus, Type II” OR “Type 2 Diabetes Mellitus” OR “Type 2 Diabetes” OR “Diabetes, Type 2”). | 23/02/2022 | 24 |
| PsycINFO | (“Self Care” OR “self management”) AND (“Social Support” OR “Social Care” OR “Online Social Support” OR “Perceived Social Support” OR “Perceived Social Supports”) AND (“nurse-led education” OR “nurse- delivered intervention” OR “nurse-led intervention” OR “program development” OR “nurse-led program”) AND (“diabetes” OR “diabetes mellitus” OR “diabetes mellitus, Type 2” OR “Diabetes Mellitus, Type II” OR “Type 2 Diabetes Mellitus” OR “Type 2 Diabetes” OR “Diabetes, Type 2”). | 23/02/2022 | 14 |
| JBI Evidence Synthesis | Self Care AND Social Support AND nurse led AND diabetes Type 2. | 09/03/2022 | 62 |
| Capes Catalog of Theses and Dissertations | “Suporte social” AND “Diabetes” | 17/03/2022 | 1429 |
| PubMed | (“Self Care” [MeSH Terms] OR “Self Care” [Text Word] OR “self management” [Text Word]) AND (“Social Support” [MeSH Terms] OR “Social Care” [Text Word] OR “Online Social Support” [Text Word] OR “Perceived Social Support” [Text Word] OR “Perceived Social Supports” [Text Word]) AND (“nurse-led education” [Text Word] OR “nurse-delivered intervention” [All Fields] OR “nurse-led intervention” OR “program development” [All Fields] OR “nurse-led program” [All Fields]) AND (“diabetes” OR “diabetes mellitus” OR “diabetes mellitus, Type 2” OR “Diabetes Mellitus, Type II” OR “Type 2 Diabetes Mellitus” OR “Type 2 Diabetes” OR “Diabetes, Type 2”) | 09/03/2022 | 19 |
Source: Search data (2022).
Study Selection
After searching the databases, all the studies were exported to a reference manager (EndNote). Duplicate articles were removed both manually and using an automation tool. It should be noted that the descriptors were adapted for each database, by using synonyms to find the greatest number of studies.
Next, the titles and abstracts were screened based on the inclusion criteria with the help of the Rayyan Systematic Reviews web/mobile app, so that two authors could independently and blindly screen the title/abstract and full text. In the event of any doubts, a third author would read the manuscript and decide whether or not to include it. Publications that met the eligibility criteria were retrieved in full.
Data Mapping
A form was designed by the author to extract the data. A pretest was then carried out to assess the need for adjustments. The data extracted included author, title, publication year, study country, journal name, document type, language, study objective, study setting, methods, population/sample size, inclusion criteria, exclusion criteria, collection instrument/technique, program results/impacts, conclusions, participants’ social characteristics, participants’ clinical characteristics, program/intervention duration, core theoretical model, resources used, program implementation, and user satisfaction assessment.
Compiling, Summarizing, and Reporting the Results
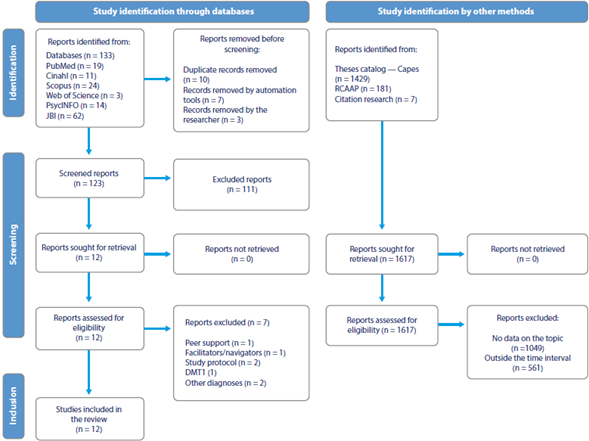
A descriptive analysis of the information related to nurse-led programs and their characteristics was carried out. The evidence was synthesized based on the research questions. A table was prepared with data allocated to the studies included in the review and another table with existing programs. Additionally, a figure was prepared with the basic theoretical model of the interventions. The search steps are represented in the flow diagram of the Preferred Reporting Items for Systematic Reviews and Meta-analyses (Prisma-ScR), which is an extension of the scoping review.
Results
Literature Search
Initially, 1,743 publications were identified, as shown in Figure 1. After removing 10 duplicate studies, the titles and abstracts were then screened, resulting in a sample containing 12 documents for full reading. Subsequently, seven publications were excluded for failing to meet the eligibility criteria, which left five publications eligible for analysis. During the review of the references in the included studies, it was found that it was necessary to incorporate seven additional documents. As a result, this review consisted of 12 studies after the inclusion of the relevant documents.
Most of the selected studies were frequently carried out more than five years ago (n = 8) in developed countries such as the United States, England, and Iran (n = 6), as shown in Table 2, which presents the main characteristics of the studies included in this review.
Table 2 Studies included in the scoping review by author, type of study, title, country, and year of publication. Brazil, 2022
| Author | Type of Study | Title | Country | Year of Publication |
|---|---|---|---|---|
| Klein HA, Jackson SM, Street K, Whitacre JC, Klein G | Article: systematic review + meta- analysis | Diabetes self-management education: Miles to go | United States | 2012 |
| Pereira DA, Costa NMSC, Sousa ALL, Jardim PCBV, Zanini CRO | Article: randomized controlled clinical trial | Efeito de intervenção educativa sobre o conhecimento da doença em pacientes com diabetes mellitus | Brazil | 2012 |
| Parker D, Clifton K, Shams R, Young J | Article: systematic review | The effectiveness of nurse-led care in general practice on clinical outcomes in adults with type 2 diabetes | Australia | 2012 |
| Mahdizadeh M, Peyman N, Thagipour A, Esmaily H | Article: randomized controlled clinical trial | Effect of health education program on promoting physical activity among diabetic women in Mashhad, Iran: Applying social cognitive theory | Iran | 2013 |
| Bertolin DC | Thesis: randomized controlled clinical trial | Estresse, modos de enfrentamento e aceitação da doença de pessoas com diabetes mellitus tipo 2 participantes de um programa educativo como envolvimento de um familiar: ensaio clínico randomizado | Brazil | 2013 |
| Tang PC, Overhag JM, Chan AS, Brown NL, Aghighi B, Entwistle MP et al. | Article: clinical trial controlado e randomizado | Online disease management of diabetes: Engaging and motivating patients online with enhanced resources-diabetes (EMPOWER-D), a randomized controlled trial | The United States | 2013 |
| Villas Boas LCG, Pace AE | Thesis: randomized controlled clinical trial | Contribuição do apoio social familiar nos resultados das intervenções educativas junto às pessoas com diabetes mellitus tipo 2: ensaio clínico controlado randomizado | Brazil | 2014 |
| Gomides DS | Dissertation: longitudinal observational study | Resultados de intervenções para o cuidado do diabetes mellitus com foco no apoio social: estudo longitudinal | Brazil | 2016 |
| Murray E, Sweeting M, Dack C, Pal K, Modrow K, Hudda M et al. | Article: randomized controlled clinical trial | Web-based self-management support for people with type 2 diabetes (HeLP- Diabetes): Randomised controlled trial in English primary care | England | 2017 |
| Golnaz A, Kim LS, Shariff GS, Said S, Sanaz A, Mosayeb M et al. | Article: double-blind randomized clinical trial | Effect of a nurse-led diabetes self- management education program on glycosylated hemoglobin among adults with type 2 diabetes | Iran | 2018 |
| Hadjiconstantinou M | Thesis: systematic review and meta- analysis + focus groups | The development of an online emotional support programme, to improve diabetes related distress and well-being in type 2 diabetes | England | 2018 |
| Van Puffelen AL, Rijken M, Heijmans MJWM, Nijpels G, Schellevis | Article: randomized clinical trial | Effectiveness of a self-management support program for type 2 diabetes patients in the first years of illness: Results from a randomized controlled trial | The Netherlands | 2019 |
Source: Research data (2022).
Regarding the study designs, there was a prevalence of randomized clinical trials (n = 8). The others were systematic reviews plus meta-analysis (n = 2), a systematic review (n = 1), and a longitudinal observational study (n = 1). As for document type, eight were articles, three were theses, and one was a dissertation.
Study Characteristics
Nurse-led programs were implemented in the following locations: general care clinics (n = 6), specialized care services for people with chronic illnesses (n = 3), and university hospitals (n = 3), as shown in Table 3. It is noted that the programs are designed to improve glycemic control and, simultaneously, achieve significant results in terms of lipid profile, blood pressure, regular physical activity, adequate nutrition, emotional stability, social interaction and, consequently, self-management.
Table 3 Nurse-led programs focusing on social support for people with type 2 diabetes by author, intervention site, results achieved, and population assisted.
| Author | Intervention Site | Intervention Results | Population Assisted |
| Klein HA, Jackson SM, Street K, Whitacre JC, Klein G | Randomly assigned | A significant reduction in blood glycated hemoglobin levels. | Age (mean): ND Sex: ND Education: ND |
| Pereira DA, Costa NMSC, Sousa ALL, Jardim PCBV, Zanini CRO | Referral service for hypertension treatment | Increased knowledge of diabetes mellitus. | Age (mean): 65.8 years Sex: Female Education: 8 years of education |
| Parker D, Clifton K, Shams R, Young J | General/family practice environment | Improvement in clinical parameters: Changes in systolic and diastolic blood pressure (BP), body mass index (BMI), cholesterol levels, HbA1c (glycated hemoglobin), and fasting glycemia. | Age: >18y Sex: ND Education: ND |
| Mahdizadeh M, Peyman N, Thagipour A, Esmaily H | Healthcare centers in Mashhad City, eastern Iran | In the intervention group (IG), light physical activity and sedentary behavior decreased from 56.1 % (23 individuals) to 14.6 % (6 individuals) in the next stage. There was a significant improvement over time in terms of physical activity (increase in the mean number of minutes practiced per week). Adherence to physical activity was higher in the groups due to the social support received, mainly from family, friends, and exercise partners. | Age (mean): 48.37 years Sex: Female Education: ND |
| Bertolin DC | Diabetes outpatient clinic at a tertiary level healthcare university hospital unit | The most commonly mentioned coping methods are cognitive restructuring, information-seeking, medium acceptance of the disease, low perception of stress, and some level of stress (in the resistance stage of the disease). | Age (mean): 60.4 years Sex: Female Education: A minimum of 0 and maximum of 17 years of education |
| Tang PC, Overhag JM, Chan AS, Brown NL, Aghighi B, Entwistle MP et al. | Palo Alto Medical Foundation, a non-profit health organization | The IG had significantly better diabetes management than the control group (CG) in the first 6 months. There was no significant difference after 12 months. The IG had significantly better management of LDL cholesterol at 12 months. There was no statistically significant difference in BP management, weight, and Framingham risk at 12 months. | Idade: > 18 years Sex: Male Education: >12 years of education |
| Villas Boas LCG, Pace AE | Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (HCFMRP-USP) | There were no statistically significant differences after carrying out the interventions for perceived self-efhcacy, knowledge about diabetes, medication adherence, and perceived social support. For the self-care variable, the CG performed better than the IG in one behavior related to eating and in two related to physical activity. Regarding the clinical variables, the CG had a lower body mass index and lower abdominal circumference in women. Metabolic management: there were no statistically significant differences, but there was a reduction in glycated hemoglobin in favor of the intervention group. | Age (mean): 60.43 years Sex: Female Education: < 9 years |
| Gomides DS | Outpatient clinic for diabetes treatment at a tertiary care hospital | There were no differences between the groups for the variables BP, waist circumference, BMI, glycated hemoglobin, fasting plasma glucose, self-care activities, knowledge about the disease, and self-efhcacy. The timeframe was defined as baseline, the end of the interventions, and 24 months after the interventions. When comparing the times, there was a reduction in BP and glycated hemoglobin and an increase in BMI and abdominal circumference in both groups. Self-care knowledge and activities increased immediately after the interventions had been carried out and decreased after two years in both groups. Self-efhcacy was maintained in the IG and reduced in the CG after two years and at the end of the interventions. Interventions including social support had no difference between the groups and over time, through descriptive analysis, there was an improvement in self- efhcacy, which was sustained after two years in the IG. Group educational interventions were effective in improving glycemic control and BP two years after the interventions had been carried out. For the knowledge variables about the disease and self-care, the results suggest the need for educational reinforcement over time. | Age: from 45 to 84 years Sex: Female Education: From 0 to 17 years of education |
| Murray E, Sweeting M, Dack C, Pal K, Modrow K, Hudda M et al. | 21 general practices in England combining urban, suburban, and rural practices | The IG participants had lower glycated hemoglobin (HbA1c) than those in the CG. There were no significant overall differences between the groups in the diabetes-related stress score, measured by the problem areas in diabetes (PAID) scale. However, for participants who had been diagnosed with diabetes more recently, it indicated a beneficial impact of the intervention on this group. | Age: 65 years Sex: Male Education: ND |
| Golnaz A, Kim LS, Shariff GS, Said S, Sanaz A, Mosayeb M et al. | Urban primary and secondary endocrine outpatient clinic located in a university hospital in the city of Ilam, Iran | The IG patients had a significant improvement in glycated hemoglobin, BP, body weight, efhcacy expectancy, outcome expectancy, and diabetes self- management behaviors. | Age (mean): 54.2 ± 11.8 years (ranging from 22 to 69 years) Sex: Female Education: 9 years of education |
| Hadjiconstantinou M | Leicester Diabetes Centre | Online support led by healthcare professionals was associated with positive well-being outcomes compared to those with non-professional support. Individually, several studies found significant improvements in well-being measurements. This was not supported by the meta-analysis for the outcome measurements of depression and distress. | Age (mean): 53.4 years Sex: Female Education: ND |
| Van Puffelen AL, Rijken M, Heijmans MJWM, Nijpels G, Schellevis | General practice clinics in the Netherlands. | Immediately after the program, the IG presented a significantly greater increase in physical activity and fruit and vegetable intake. Six months after the intervention, these effects had disappeared. Regarding diabetes-related suffering, no immediate or six-month effects were found. The baseline levels of self-care seemed to be slightly higher in the IG, but not significantly higher. Six months after the intervention, the differences in empowerment were still present, even though healthy behaviors had decreased. Considering distress, there were no significant changes, as levels of distress were low even before the intervention had been carried out. | Age (mean): 63.5 years Sex: Male Education: 12 years of education |
Source: Research data (2022).
Key: ND - not defined.
The participants’ characteristics indicate a mean age of 54.2} 11.8 years (between 22 and 69 years), with a prevalence of women (n = 7), with a low level of education, having studied for a total of nine years (n = 8).
The studies found on emotional support covered programs consisting of individual, face-to-face counseling, followed by a collective approach and dynamics with family/friends. To consolidate learning, phone calls were made (Table 4). Therefore, the programs converged on an educational basis -with instructions in face-to-face appointments and via phone calls- with a strong influence of affective aspects, since the person with diabetes would need to be the protagonist of their decisions, but there was also family interaction. On average, the interventions lasted 12 months, with a maximum of 36 months and a minimum of 1 month.
Table 4 Programs by Author, Type of Intervention, and Duration
| Author | Type of Intervention | Duration |
|---|---|---|
| Klein HA, Jackson SM, Street K, Whitacre JC, Klein G | Rules and procedures: Rules concerning diet and exercise. Rules for procedures, such as using a diary to record daily glucose levels. Affective: Encouragement and motivation to build trust. Social and situational: Approach focused on managing social and situational factors. Strategies that encompass planning meals on vacation and in restaurants. Complex cognition: Use of mental models or other cognitive strategies to support the understanding of diabetes, which are used to moderate blood glucose levels. | Three categories: 13 weeks or less, 14-26 weeks, 27 weeks or more. |
| Pereira DA, Costa NMSC, Sousa ALL, Jardim PCBV, Zanini CRO | The IG participated in 12 educational meetings over six months, held every two weeks and lasting an average of two hours. The first two educational meetings were held to identify the learning needs and previous knowledge about the disease among the research participants. A pre-established script was used for the discussion, which aimed to identify the patients’ knowledge of diabetes, the difhculties caused by the disease, and their perception of what could help with treatment. Organization of educational activities: a teaching plan was devised. Each plan used distinctive resources, such as pictures, phrases written by the patients themselves, posters, songs, walks, questions, and verbal expressions of meaningful experiences. | 6 months |
| Parker D, Clifton K, Shams R, Young J | Care is guided by nurses who are recognized as having a leadership role in the care of patients with T2DM compared to care provided by general practitioners. | Not defined. |
| Mahdizadeh M, Peyman N, Thagipour A, Esmaily H | The training program has been introduced. Introductory session: The rules have been announced. First session: Discussion regarding a healthy lifestyle. Second session: Discussion about problems and the search for alternatives to overcome barriers. Third session: Assigning objectives and their importance in achieving favorable results. Fourth session: Dialogue about having a regular program and planning physical activity. Fifth, sixth, and seventh sessions: Walking program and practical training course in physical activity. | 7 sessions (4 theoretical and 3 practical) in 1 month (each session ≈ 60 min) |
| Bertolin DC | Intervention with people with diabetes: performed in groups, using conversation maps. It is a tool that aims to empower people to make decisions. It provides discussions and dynamics in groups of up to 10 people. Maps were used, focusing on how the body and diabetes work (map 1), healthy eating and physical activity (map 2), monitoring blood glucose (map 3), and achieving insulin-related goals (map 4). A total of four meetings were held. Intervention with family members of people with diabetes: Through phone calls. Weekly calls were made, using the motivational interviewing technique. In this technique, the professional establishes an empathetic and collaborative relationship with the person. It follows pre-established protocols and uses the social cognitive theory. The topic of the conversation maps from the group meetings is addressed. A total of 17 calls were made. | 23 months |
| Tang PC, Overhag JM, Chan AS, Brown NL, Aghighi B, Entwistle MP et al. | 1st) Home glucose meter readings with graphical feedback; 2nd) Comprehensive report of the patient’s specific diabetes status; 3rd) Nutritional and workout records; 4th) Insulin record; 5th) Online messaging with the patient’s healthcare team; 6th) Nursing care manager and nutritionist providing advice and medication management, and 7th) Short personalized texts and educational videos provided electronically by the healthcare team. | 12 months |
| Villas Boas LCG, Pace AE | IG: Educational intervention with the participation of the family caregiver through phone calls. Returns occur every three months. A second assessment was done at 12 months. CG: No family member participation. Group educational interventions for people with T2DM: A maximum of eight participants. Approach carried out based on diabetes mellitus conversation maps. This tool aims to empower the individual to self-manage. The topics covered followed those available in Portuguese (how the body and diabetes work; healthy eating and physical activity; medication treatment; blood glucose monitoring; and achieving insulin-related goals). Educational interventions for family caregivers of people with T2DM: Phone calls following motivational interviews with a technique designed to generate collaborative empathy. Topics previously established by the diabetes conversation maps were discussed. A total of 17 calls lasting an average of eight minutes each have been made. | Approximately 12 months |
| Gomides DS | Educational interventions that provide information related to the disease and the self-care activities required for treatment, using visual and interactive tools based on the social cognitive theory, whose key concept is personal belief in one’s ability to perform certain tasks (self-efhcacy). | The study times were baseline (T0), end of interventions (T12), and 24 months after completion (T36). |
| Murray E, Sweeting M, Dack C, Pal K, Modrow K, Hudda M et | It is an application developed specifically for people with T2DM. The contents present in this application include information about diabetes, how diabetes is treated, possible complications from diabetes, possible impacts of diabetes on relationships at home and work, dealing with unusual situations such as parties, holidays, travel, or shift work, and what lifestyle changes will improve health, skills, and behavior change. Special modules cover behavior change, healthy eating, weight loss, being more physically active, quitting smoking, moderating alcohol consumption, managing medication, glycemic management, and BP management. In addition, content on emotional well-being and sharing experiences between users is available. Possibility of receiving monthly notifications with relevant news about diabetes. | 12 months |
| Golnaz A, Kim LS, Shariff GS, Said S, Sanaz A, Mosayeb M et al. | The participants in the intervention group received a booklet at the beginning of the program, whose content was used throughout the intervention to guide learning, development, and discussion or it was used to create resources for self-guided learning. Within the first four weeks of the intervention, participants were invited to watch four weekly 10-minute films on the prevention of short- and long-term complications (session 1), physical activity, daily foot care (session 2), healthy eating (session 3), and healthy living with diabetes (session 4). Four group discussion sessions were held at weekly intervals, but the schedule was flexible, and attendance was limited to 10 participants for each session. These sessions were held weekly during the first four weeks of the intervention. Each session lasted 120 minutes. All group members were encouraged to attend each session. Group members who missed a session received a follow-up from the moderator before the next session. At the last meeting of the group session, all group members were handed a list of home phone numbers and encouraged to ask for help if necessary. Two months following the end of the group discussion sessions, the intervention participants received a phone call once a week. Each follow-up call lasted approximately 15 to 20 minutes. At the end of the intervention, the CG participants were handed an educational booklet and films. | 3 months |
| Hadjiconstantinou M | Techniques for behavior change: To provide information; tracking/self-monitoring; to provide motivation; to provide feedback; goal setting; problem-solving; action planning; social support; emotional regulation training, and immediate review of behavioral goals. | A minimum of 6 months and a maximum of 18 months. |
| Van Puffelen AL, Rijken M, Heijmans MJWM, Nijpels G, Schellevis | It consists of three monthly two-hour interactive sessions and a follow-up session three months after the last session. The sessions were led by two nurses specializing in diabetes or nurses who received four hours of training and a detailed manual describing the content of the program and its underlying theories to be used during the sessions. The participating patients and their partners received a booklet containing basic information on diabetes, (homework) assignments, and theoretical and practical information on the topics discussed throughout the course (both books are available in Dutch from the author). The CG participants were invited to a single two-hour educational lecture, in which they received information about living with diabetes from a medical perspective. A professor of general practice and diabetes care provided information about the course of diabetes (including treatment options and possible complications) and the latest developments in diabetes research, according to the classic didactic method. | 8 months |
Source: Research data (2022).
Regarding the basic theoretical model used by the programs, most followed the social cognitive theory (n = 3), conversation maps (n = 2), the common sense self-regulation theory (n = 2), the self-efficacy theory (n = 1), and motivational interviewing (n = 1). It is worth noting that the studies that were not mentioned correspond to the fact that they did not present their respective basic models and/or clarified the theoretical framework.
Analysis and Discussion
Evidence Summary
The present study found studies conducted in England, the United States, Iran, Australia, and the Netherlands on programs focused on social support for the self-management of people with T2DM, which were led by nurses and centered on care facilities for people with chronic diseases (9, 11-15).
It is worth noting that in these countries, care for people with diabetes is performed in a unique way and with a holistic approach (16). In developing countries such as Brazil, this approach is still in its infancy, despite efforts to improve care for this population, which has increased significantly over the years (17). Factors such as adequate spending of financial resources on healthcare services, continued training processes and engagement of professionals, as well as technological support and priority on conflict management may be associated with the differences mentioned between these regions (18-20).
In addition, strategies for patients’ attendance and commitment to the treatment of chronic diseases are related to family engagement and effective professional intervention, which highlights the importance of social support in achieving these goals. Such support is an essential tool for promoting improvements in health and interpersonal relationships, which leads to improved cognitive performance, and negative emotional reactions management -e.g., anxiety, and offers behavioral analysis (21, 22). The literature highlights the key role played by nursing professionals in primary care in health education activities and self-management through evidence-based practices (23).
In the present study, the findings regarding the theoretical framework that integrates social support into the main strategic interventions were the social cognitive theory (an active pedagogical strategy that determines that individuals influence and are influenced by observational learning [13, 24-26]); conversation maps (a tool subdivided into four stages, delivered to patients via images and metaphors reproduced on a card table with specific topics [27]); the self-efficacy theory (which determines that commitment, depending on personal will and ability, is decisive in preventing or managing the disease [28]); motivational interviewing (evidence-based counseling, in which healthcare professionals help people adopt targeted treatment recommendations [29]); and the common sense self-regulation theory (which provides strategies aimed at finding out how people feel and think about the disease [30]).
These theories can lead to several benefits for patients, such as a reduction in sedentary lifestyles, which has an impact on BMI control and abdominal circumference in women, a better understandingand acceptance of the disease, as well as stress reduction and increased consumption of fruit and vegetables (13, 24, 25). Thus, knowledge of these theoretical models can enable them to be implemented through low-cost programs and favor care processes with a reduction of risks and problems (31, 32).
A study published in the Revista de Medicina da Universidade de São Paulo showed that the perception of social support and family functionality were positive and there was a significant relationship between glycemic levels and information on the adequate management of T2DM in elderly males, which highlights the importance of family support in the therapeutic management of the disease. Nurse-led programs focused on promoting social support and family integration can promote better engagement between patients and their families and, consequently, contribute to improved self-care, healthy eating habits, and physical activity (33- 35). In addition, it is worth highlighting the inclusion of people with T2DM in support groups and educational activities, as this allows for joint interaction, and sharing experiences and feelings (36).
Regarding the multidisciplinary approach, nutritional interventions focused on fruit and vegetable intake and physical exercise programs were noted (15, 25, 37). In the field of nursing, the use of online tools was the main form of intervention and satisfactory results were achieved in terms of glycated hemoglobin values, fasting glycemia, BP levels, and anthropometric data (9, 14, 24, 31, 37-39, 44). It is worth pointing out that, in the field of primary care, nutritional monitoring associated with an adequate diet has led to the best short-term results with a balanced diet specific to each individual (40).
Regarding physical training programs for people with T2DM, these provided greater benefits by improving insulin sensitivity and glycated hemoglobin, which resulted in lower postprandial hyperglycemic peaks. The recommendation to practice physical exercise between 150 and 300 minutes (light to moderate) or 75 to 150 minutes (intense) has an impact on muscle strength and greater endurance capacity in these individuals, which can improve functional capacity and body maintenance (41). In addition, the professional support provided to recently diagnosed patients has benefits, such as reducing stress levels, especially in those who have been diagnosed within less than five years, and who are more resistant to accepting the disease (13, 15, 31, 44).
However, it is worth noting that, although self-management is effective in changing the cognition of people with T2DM, contributing to behavioral change and emotional perception, the maintenance of these behaviors still seems to be insufficient in the long term; therefore, an approach with individuals who have been diagnosed for longer is also essential, as it ensures continuity of care, reduces the possibility of chronic complications such as neuropathy, retinopathy, renal and neurological damage (25, 42).
The present review found that online programs and phone-based approaches under the guidance and leadership of a nurse were more likely to lead to adherence by participants. This can be justified by the fact that technological resources make communication easier, although access to these devices must be considered (9, 12- 15, 24, 25, 31, 39, 43, 44).
Thus, due to the complexity of the treatment, effective adherence by patients becomes a challenge not only for them but also for the healthcare team and family members. Consequently, comprehensive support and reframing of these individuals’ lifestyle habits must have an impact to promote the practice of effective self-care, as well as conscious decision-making with empowerment through cognitive restructuring (25, 44-47).
As such, the social importance of nurse-led programs for individuals with T2DM is materialized as an important alternative in the follow-up of these individuals in terms of risk reduction, adequate self-care management, and satisfactory family support, which contributes to personal satisfaction and lower demand for healthcare services (9, 48-50).
Limitations and Strengths
Although the methodological evaluation of studies is not a stage covered by the scoping review methodology, this can influence the results. The study was limited to the English, Portuguese, and Spanish languages, which may represent a selection bias. Thus, programs from other languages/cultures are not represented in this study. In addition, the studies did not clarify the follow-up and monitoring of the participants included in them, which hinders identifying and characterizing them in the medium and long term.
The strengths of the review include the rigorous and transparent approach adopted to select relevant studies, conducted in line with the Prisma-ScR guidelines. The strengths also lie in the collaboration of a multidisciplinary team of reviewers and the collaboration of librarians with expertise in systematic and scoping reviews to devise the search string.
Conclusions
Based on the results presented, it was found that nurse-led social support programs for self-management are patient- and family- centered and also use playful and educational auditory or visual strategies and can be based on collective and face-to-face sessions and phone calls. The main results of these programs were improved glycemic control, hemodynamics, and lipid profile. In addition, there has been an improvement in emotional and behavioral parameters, especially in the perception of stress and self-management.
Although there is a tendency for an increase in the number of these programs, there are still gaps that warrant attention; there is a need for future studies focused on emotional levels, such as depression and anxiety, as there was no unanimity on these findings. These psycho-emotional aspects can negatively influence the physiological and metabolic parameters of patients with T2DM. Furthermore, there is a need to conduct studies with individuals who have been diagnosed for longer, as there was a prevalence of individuals who had been diagnosed less than five years ago.
Nurse-led programs focusing on social support seem to be an intervention that can lead to more effective self-management, meeting people’s real needs and, consequently, achieving positive health outcomes in the T2DM setting. The relevance of this type of study in following up with participants in the medium and long term is emphasized to highlight the benefits of the proposed interventions.











 text in
text in