Remark
| 1) Why was this study conducted? |
| This study was conducted to measure the level of evidence-based practice specifically among respiratory health professionals in Latin America. Recognizing the strengths and weaknesses of this practice is necessary to establish a diagnosis and subsequently make informed decisions. |
| 2) What were the most relevant results of the study? |
| Most professionals in the respiratory field in the region have attained postgraduate qualifications and demonstrate high to medium-high levels of evidence-based practice. Principal strengths arise from their level of education and engagement in scientific literature, while deficiencies primarily revolve around institutional support. |
| 3) What do these results contribute? |
| The findings underscore the necessity for educational emphasis and institutional support concerning evidence-based practice, addressing both undergraduate and postgraduate education, as well as ongoing professional development for practitioners. |
Introduction
Evidence-based practice is a systematic and rigorous approach to medical practice based on using the best available evidence to make informed clinical decisions 1. Evidence-based practice emerged as a response to the growing amount of medical information available and the need to find an effective way to evaluate and apply this information in daily practice. Evidence-based practice has become a gold standard for medical practice and has been incorporated into the training of professionals worldwide 2.
Evidence-based practice has its roots in the 1970s when Cochrane, a Scottish medical epidemiologist, conceived the concept of best practice. As the amount of medical information available grew exponentially in the following decades, it became increasingly evident that a more systematic approach was needed to evaluate and apply this information in medical practice 3.
In 1992, a group of physicians and epidemiologists at McMaster University in Canada developed the first Evidence-based practice course, which became a model for teaching worldwide. The Evidence-based practice approach was quickly adopted by many leaders in medical research and clinical practice, and in 1996 the Cochrane Collaboration was created, an international network of researchers dedicated to producing and disseminating systematic reviews of the medical literature 4.
Since then, Evidence-based practice has significantly impacted medical practice worldwide and has become an integral part of medical training in many universities and residency programs 5. However, despite its importance, there are still significant barriers to the effective implementation of Evidence-based practice in clinical practice 6.
Teaching about Evidence-based practice is associated with significantly increasing healthcare professionals' knowledge and application 7 and significantly improving physicians' ability to search for and apply evidence in their clinical practice 8. It has also been reported that despite physicians being familiar with Evidence-based practice, only a minority apply it systematically in their clinical practice 9.
Additionally, teaching Evidence-based practice from the medical school curriculum significantly improves students' knowledge and application of Evidence-based practice 10.
Evidence-based practice measurement has been conducted and analyzed in various settings across regions like North America 11, Europe 12, and Asia 13. These assessments have targeted a range of health professions, in which it has been identified that one of the most impacting factors are scientific skills such as the writing of scientific articles 14,15 and other disciplines 16, each implementing specific measurement criteria.
Meanwhile, related data for respiratory health personnel in Latin America are scarce, so the findings of this study could provide relevant information to compare different contextual settings and health services to manage better even health systems and the care of respiratory patients in the region.
In this context, the present study evaluates the knowledge of Evidence-based practice by Health-Sciences Evidence-Based Practice Questionnaire (HS-EBP) in healthcare professionals such as physicians, physical therapists, nurses, respiratory therapists, speech-language therapists, and occupational therapists in Latin America.
Materials and Methods
Design
A cross-sectional study was conducted between December 1 2022 and March 31 2023, developed with a questionnaire distributed through Google Forms® applied in several Latin American countries. The Health-Sciences Evidence-Based Practice Questionnaire (HS-EBP) was administered to respiratory health professionals in the region. The survey consisted of 60 questions on 11 pages (screens); the first page included general data on the study, the link for informed consent, and the duration of completion. The second page included general information about the participants (sociodemographic data and their organization), and the following pages included the five dimensions of the HS-EBP questionnaire. The study was approved by the ethics committee of the Clínica de Occidente S.A. in Colombia (IYECCDO-1299) and approved by the institutional board of the Respiratory Care Department of the Latin American Thoracic Association (ALAT). It was designed based on the Consensus-Based Checklist for Reporting of Survey Studies (CROSS) 17.
Public involvement
The population associated with this study was not involved in setting the research question or the outcome measures. The target population will be central in the dissemination of the results through presentations at congresses or webinars.
Recruitment
From December 1 2022, to March 31, 2023, the questionnaire was distributed by the ALAT communications team to its associates via email and also on the official webpage of the association, and the researchers also disseminated the survey through social networks in their personal and professional networks, seeking a snowball effect to reach the highest level of participants. Prior to completing the questionnaire, participants had to accept the terms of the written informed consent form, which was available in a link inserted in the questionnaire. Then, the questionnaire was completed, and personal data was handled with the appropriate confidentiality. No sensitive data or I.P. addresses were stored. Participation was voluntary, and no monetary compensation was offered. Participants were recruited by convenience and met inclusion criteria such as: legal age, having a degree as a health professional in the country where he/she resided at the time of completing the questionnaire, practicing as a qualified professional in the country where he/she completed the questionnaire, professionals who have been working in the respiratory area for at least one year. Respiratory health professionals who did not complete the questionnaire in Google Forms and those who completed the survey after March 31, 2023, were excluded.
Questionnaire
For Spanish-speaking countries, the original Spanish version of the questionnaire was applied 18; for Brazil, the Portuguese version was used 19. The HS-EBP is a self-administered questionnaire composed of 60 items in which each response ranges from 1 to 10, has a Likert format in which one responds to strongly disagree to 10 strongly agree, with five factors: "Beliefs and attitudes" (F1) with 12 items, "Results from literature" (F2) with 14 items, "Professional practice" (F3) 10 items, "Assessment of results" (F4) 12 items and "Barriers and facilitators" (F5) 12 items. Because each factor has a different number of questions, their maximum and minimum scores are different. F1 ranges from 12 to 120, F2 from 14 to 140, F3 from 10 to 100, F4 from 12 to 120 and f5 from 12 to 120 18.
The instrument has demonstrated reliability and validity in health personnel with high Cronbach's Alpha coefficients 20. It has also shown evidence of validity about variables such as dispositional resistance to change, burnout, and professionals' quality of life, as well as other evidence-based practice questionnaires such as the Evidence-Based Practice Questionnaire (EBPQ).
In addition to the HS-EBP questionnaire, variables such as gender, age, profession, degree of training, country of origin, the work environment of greatest dedication, training in Evidence-based practice, time of experience in the respiratory health area, and specific work areas were included. Similarly, questions were asked about the location of their main activity, the habit of reading scientific articles, training in evidence-based practice, continuing education activities, and self-evaluation of their performance.
Statistical analysis
The data were organized and administered confidentially, and a descriptive univariate analysis was performed for the general characteristics of the population in which frequencies and percentages were obtained for qualitative variables; quantitative variables were processed with basic descriptive statistics (Mean) (S.D.) (95% mean CI). The Kolmogorov-Smirnov test was applied for distribution analysis, In the case of abnormal distribution, a nonparametric test was used.
According to the normative data of the HS-EBP factors, the percentiles of all data were distributed, and quantitative variables were contrasted with t-tests in the case of dichotomous variables. For comparing the results of the scale domains with patient characterization variables in which more than two groups were obtained, one-way ANOVA was applied with a Bonferroni post hoc test for multiple comparisons. This analysis was performed with SPSS software, version 25 (IBM Corp., Armonk, NY, USA). Fisher's exact test identified the statistical association between the questionnaire scores and the other variables of interest, with a significance level of 5%. Subsequently, a factor analysis was performed in a multiple correspondence analysis combined with the hierarchical clustering technique. Cluster analysis was performed to observe the associations between categories and individuals better using all the Multiple Correspondence Analysis (MCA) factorial axes. The R Studio software (version 4.3.0) implemented the analysis using the factoextra packages for factor analysis and FactoMineR for cluster development.
Results
Only those who completed the survey were considered for collecting questionnaire data. A total of 472 responses were received, of which 18 participants who did not live in Latin American countries (United States, Canada, Sweden, Spain, among others) were excluded. Also excluded were 4 participants who, although they answered the survey in its entirety and lived in the region, did not accept the terms of the informed consent, and 2 participants were excluded because they reported never having worked in the respiratory area. For these reasons, 448 participants were finally admitted to the study, and the respective analyses were conducted.
Most participants were female (51.2%) with a mean age of 42 ±12. Regarding the professions, most responses were obtained from medical professionals, followed by physiotherapy, nursing, and respiratory therapy; responses were also received from occupational and speech therapists, but none of these two professions exceeded five responses. Finally, regarding the level of training, almost 50% of the participants had a specialization level, while 22.1% had a bachelor's degree.
The questionnaire was distributed in all Latin American countries, with responses from 17 countries, the largest proportion coming from Colombia, followed by Mexico, Argentina, Brazil, Chile, Peru, Ecuador, and Venezuela. Also, to a lesser extent, responses were obtained from Bolivia, Costa Rica, Cuba, El Salvador, Guatemala, Honduras, Paraguay, the Dominican Republic, and Uruguay (Table 1).
Table 1 Demographic characteristics of participants in Health Sciences - Evidence-Based Practice
| Gender n (%) | Female | 229 (51.2) |
|---|---|---|
| Age mean (SD) | 42 (12) | |
| Profession n (%) | Medicine | 220 (49.1) |
| Physical Therapy | 177 (39.5) | |
| Nursing | 26 (5.8) | |
| Respiratory Therapy Other | 20 (4.5) 5 (1.1) | |
| Academic level n (%) | Doctorate | 34 (7.6) |
| Master | 93 (20.8) | |
| Specialization | 221 (49.4) | |
| Bachelor | 99 (22.1) | |
| Country of residence n (%) | Colombia | 103 (23.04) |
| Mexico | 67 (14.98) | |
| Argentina | 65 (14.5) | |
| Brazil | 55 (12.30) | |
| Chile | 47 (10.5) | |
| Peru | 36 (8.05) | |
| Ecuador | 33 (7.3) | |
| Venezuela Other* | 10 (2.2) 32 (7.1) | |
| Management functions n (%) | Yes | 183 (40.9) |
| Continuing education courses n (%) | Yes | 415 (92.8) |
| Training in Evidence-based practice n (%) | Yes | 229 (51.3) |
| Read of scientific articles n (%) | Frequently | 300 (67.1) |
| Sometimes | 142 (31.8) | |
| Almost never | 5 (1.1) | |
| Years working in the respiratory area mean (SD) | 13 (10) |
SD: Standard deviation.
*. In alphabetical order: Bolivia, Costa Rica, Cuba, Dominican Republic, El Salvador, Guatemala, Honduras, Paraguay, and Uruguay
The mean of the beliefs and attitudes domain was 109 ±12, of the results from the literature domain 115 ±20, of professional practice 84 ±11, assessment of results 96 ±19.and Of barriers/facilitators 76 ±27, having an abnormal distribution secondary to applying the K-S test; the median values were 112, 118, 86, 99 and 79 for each of the five domains (Table 2).
Table 2 Descriptive statistics of factor scores of the Health Sciences Evidence Based Practice questionnaire
| Beliefs and attitudes F1 | Results from literature F2 | Professional practice F3 | Assessment of results F4 | Barriers/Facilitators F5 | |
|---|---|---|---|---|---|
| Mean (SD) 95% CI | 109 (12) 108 - 110 | 115 (20) 113 - 117 | 84 (11) 83 - 85 | 96 (19) 94 - 98 | 76 (27) 73 - 78 |
| Median | 112 | 118 | 86 | 99 | 79 |
| p25-75 | 103 - 119 | 106 - 130 | 78 - 92 | 94 - 98 | 56 - 97 |
| Range | 55 - 120 | 37 - 140 | 41 - 100 | 12 - 120 | 12 - 120 |
SD: Standard deviation, CI: Confidence interval
Table 3 presents the normative data of the five questionnaire factors according to percentiles; the results are presented in total score and average in the range of 1 to 10 to facilitate interpretation.
Table 3 Normative data for the five factors of the Health Sciences - Evidence Based Practice questionnaire
| Data for the five factors of the HS-EBP questionnaire (total score and mean score of item response scale). | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| F1 | F2 | F3 | F4 | F5 | ||||||
| Total | Mean | Total | Mean | Total | Mean | Total | Mean | Total | Mean | |
| Percentiles | 12-120 | 1-10 | 14-140 | 1-10 | 10-100 | 1-10 | 12-120 | 1-10 | 12-120 | 1-10 |
| 1 | 70 | 5.83 | 53.9 | 3.84 | 52 | 5.2 | 41.4 | 3.45 | 16.44 | 1.37 |
| 5 | 84 | 7 | 75.2 | 5.37 | 64.4 | 6.44 | 60 | 5 | 27 | 2.25 |
| 10 | 94 | 7.83 | 87.8 | 6.27 | 70 | 7 | 69 | 5.8 | 37 | 3.08 |
| 15 | 97 | 8.08 | 95 | 6.79 | 74 | 7.4 | 76 | 6.30 | 45 | 3.75 |
| 20 | 100 | 8.33 | 101 | 7.21 | 76 | 7.6 | 81 | 6.78 | 49 | 4.08 |
| 25 | 103 | 8.58 | 106 | 7.57 | 78 | 7.8 | 86 | 7.17 | 56 | 4.67 |
| 30 | 105 | 8.75 | 109 | 7.79 | 80 | 8 | 88 | 7.33 | 61.4 | 5.1 |
| 35 | 107 | 8.92 | 112 | 8 | 81 | 8.1 | 91.8 | 7.65 | 67 | 5.58 |
| 40 | 108 | 9 | 113 | 8.07 | 82.2 | 8.22 | 94 | 7.83 | 72.2 | 6.01 |
| 45 | 110 | 9.17 | 116 | 8.29 | 85 | 8.5 | 96 | 8 | 75 | 6.25 |
| 50 | 112 | 9.33 | 118 | 8.43 | 86 | 8.6 | 99 | 8.25 | 79 | 6.58 |
| 55 | 114 | 9.5 | 120 | 8.57 | 87 | 8.7 | 100 | 8.33 | 83 | 6.92 |
| 60 | 116 | 9.67 | 123 | 8.79 | 88 | 8.8 | 103 | 8.58 | 86 | 7.17 |
| 65 | 117 | 9.75 | 125 | 8.93 | 90 | 9 | 106 | 8.8 | 90 | 7.5 |
| 70 | 118 | 9.83 | 127 | 9.07 | 91 | 9.1 | 108 | 9 | 93 | 7.75 |
| 75 | 119 | 9.92 | 130 | 9.29 | 92 | 9.2 | 111 | 9.25 | 97 | 8.08 |
| 80 | 120 | 10 | 132 | 9.43 | 94 | 9.4 | 114 | 9.5 | 101 | 8.42 |
| 85 | 120 | 10 | 136 | 9.71 | 95 | 9.5 | 117 | 9.75 | 104 | 8.67 |
| 90 | 120 | 10 | 138 | 9.86 | 98 | 9.8 | 120 | 10 | 109.2 | 9.09 |
| 95 | 120 | 10 | 140 | 10 | 100 | 10 | 120 | 10 | 116 | 9.67 |
| 99 | 120 | 10 | 140 | 10 | 100 | 10 | 120 | 10 | 120 | 10 |
HS-EBP: Health Sciences - Evidence-Based Practice
The results of the variables are compared in Table 4, and a comparison is made between the congeners, academic level, training in evidence-based practice, type of bachelor's degree, professional activity, sector, and country. In factor 3, differences were found between people with and without training in PBS, which is repeated in all the questionnaire domains. In professional activity, people involved in primary care had lower levels in the questionnaire compared to the other activities (clinic/hospital, university, and private practice). Regarding the countries, differences were identified in the F2 in countries such as Argentina and Chile compared with the results of Mexico and in the F3 in Ecuador compared with Colombia; however, the behavior between countries is very similar in the survey results.
Table 4 Differential analyses on the Health Sciences - Evidence Based Practice dimension scores
| F1 | F2 | F3 | F4 | F5 | |
|---|---|---|---|---|---|
| Gender | |||||
| a. Female | 111 (108-114) | 118 (116-120) | 85 (83-87) | 98 (95-101) | 76 (71-81) |
| b. Male | 112 (111-116) | 122 (118-125) | 87 (85-89) | 99 (96-103) | 85 (76-86) |
| Academic Level | |||||
| a. Bachelor | 109 (107-114) | 113 (106-117) b*cd** | 85 (82-87) | 93 (87-97) c**d* | 66 (58-76) b*cd** |
| b. Specialist | 111 (109-112) | 118 (116-120) c*d** | 86 (83-88) | 97 (95-100) c* | 79 (75-85) |
| c. Master | 116 (112-118) | 127 (124-131) | 87 (84-89) | 106 (99-110) | 85 (99-110) |
| d. Doctorate | 113 (107-119) | 129 (122-134) | 87 (84-92) | 103 (96-113) | 91 (76-102) |
| Training in Evidence Based Practice | |||||
| a. No | 108 (107-110) b** | 113 (110-116) b** | 85 (82-86) b** | 93 (89-96) b** | 69 (63-74) b** |
| b. Yes | 115 (113-117) | 125 (124-128) | 88 (85-89) | 102 (99-106) | 86 (83-91) |
| Bachelor | |||||
| a. Nursing | 107.5 (98-117) | 117.5 (100-124) | 79.5 (73-85) | 88.5 (69-102) | 66 (49-95) |
| b. Physical Therapy | 112 (111-116) | 118 (115-120) | 85 (82-87) | 99 (96-101) | 76 (70-83) |
| c. Medicine | 111 (109-114) | 122 (119-125) | 86.5 (85-88) | 98.5 (95-102) | 82 (76-86) |
| d. Respiratory Therapy | 112 (103-118) | 120 (115-124) | 84.5 (76-94) | 97 (87-113) | 77 (49-104) |
| Professional activity | |||||
| a. Primary Care | 109 (94-112) c** | 114 (108-125) c** | 80 (75-91) | 86 (66-105) c** | 45 (34-60) bcd** |
| b. Clinic/Hospital | 111 (109-113) c* | 119 (109-113) c** | 85 (83-87) | 97 (95-100) c* | 77 (72-82) cd** |
| c. University | 118 (112-120) | 131 (125-136) | 89.5 (84-96) | 109.5 (99-117) | 99 (86-109) |
| d. Private Consultation | 114 (108-118) | 115 (110-130) c** | 88.5 (83-91) | 100 (87-107) | 78.5 (73-87) |
| Sector | |||||
| a. Public | 111.5 (109-114) | 120 (118-123) | 86 (84-87) | 99 (96-102) | 70 (65-79) b** |
| b. Private | 112 (109-116) | 119 (116-122) | 86 (83-88) | 99 (95-103) | 85 (81-89) |
| c. Mixed | 111 (120-65) | 122 (117-126) | 86 (83-89) | 97 (94-100) | 75 (71-84) |
| Years working in the respiratory area | |||||
| a. 1-10 | 113 (108.1-111.1) | 117 (111-116.2) | 85 (82-85) | 96 (90.8-96)c* | 75 (70-77.3) |
| b. 11-20 | 112 (107.3-111.4) | 120 (112.9-119.7) | 86 (83.4-86.8) | 101 (95-101) | 83 (72.8-81.9) |
| c. > 20 | 109 (104.4-109.5) | 121 (114-6-121.8) | 88 (84.2-87.7) | 101 (96.8-103.6) | 84 (73.9-84.1) |
| Country | |||||
| a. Argentina | 108 (103-110) | 117 (112-119) f* | 87 (82-89) | 98 (94-102) | 76 (66-86) |
| b. Brazil | 115 (108-119) | 122 (115-128) | 84 (80-86) | 100 (90-107) | 84 (76-96) |
| c. Chile | 109 (107-115) | 115 (109-120) f* | 85 (81-88) | 94 (86-98) | 67 (61-76) |
| d. Colombia | 116 (115-118) | 123 (115-131) | 89 (87-90) | 102 (97-110) | 84 (77-92) |
| e. Ecuador | 108 (98-116) | 115 (112-122) | 80 (73-87) d* | 93 (77-103) | 83 (65-88) |
| f. Mexico | 118 (112-120) | 127 (122-129) | 89 (85-92) | 105 (98-109) | 84 (75-90) |
| g. Peru | 107 (100-113) df* | 120 (116-126) | 82 (77-88) | 95 (85-102) | 76 (59-83) |
Subsequently, the main variables of the study were categorized proportionally for the conformation of these clusters, considering the factors of the questionnaire and variables such as age, gender, country of residence, highest academic level, profession, training in Evidence-based practice, and professional activity. The proportion between the dimensions and the other variables of the questionnaire according to the high, medium-high, medium, medium-low, and low scores, obtaining that all dimensions (except for the dimension of barriers and facilitators) have a high score is shown in Table 5. It is also possible to identify that the low score is almost null, except for F5, where almost 9% of the participants are located.
Table 5 Dimensions of the questionnaire according to the scores of Health Sciences - Evidence-Based Practice Questionnaire
| Health Sciences - Evidence Based Practice | High score (%) | Medium-High Score (%) | Medium Score (%) | Medium-Low Score (%) | Low Score (%) |
|---|---|---|---|---|---|
| F1. Beliefs and attitudes | 82.1 | 15.4 | 2.2 | 0.2 | 0.0 |
| F2. Results from literature | 55.4 | 33.3 | 9.4 | 1.6 | 0.5 |
| F3. Professional practice | 60.0 | 35.0 | 4.7 | 0.2 | 0.0 |
| F4. Assessment of results | 50.0 | 33.7 | 13.6 | 2.2 | 0.5 |
| F5. Evidence Based Practice Barriers/Facilitators | 21.9 | 28.8 | 25.0 | 15.4 | 8.9 |
Based on the analysis of the variables' correlation with the obtained scores, a statistical association was identified between the five dimensions of the questionnaire and factors such as participation in Evidence-Based Practice training and the habit of reading scientific articles. Characteristics like educational degree and completed courses demonstrated a statistical association with three dimensions (F2, F4 and F5). Country of residence correlated with F1 and F4; professional activity with F2 and F5, and gender with F1 and F2, while profession correlated with only one dimension, specifically the second. Notably, categorized age did not show any statistical association with any dimension of the questionnaire (Table 6).
Table 6 Association between the scores of the dimensions and other variables of the questionnaire
| HS-EBP questionnaire | Country of residence | Academic Level | Profession | Professional Activity | Training in EBP | Reading scientific articles | Gender | Age |
|---|---|---|---|---|---|---|---|---|
| F1. Beliefs and attitudes | 0.02199* | 0.1434 | 0.3618 | 0.2269 | 0.0004998* | 0.0004998* | 0.02099* | 0.2389 |
| F2. Results from literature | 0.2234 | 0.0004998* | 0.0004998* | 0.0009995* | 0.0004998* | 0.0004998* | 0.01699* | 0.3498 |
| F3. Professional practice | 0.1324 | 0.2814 | 0.4763 | 0.2859 | 0.006497* | 0.0004998* | 0.7581 | 0.2499 |
| F4. Assessment of results | 0.04648* | 0.004498* | 0.05897 | 0.08646 | 0.0004998* | 0.0004998* | 0.5112 | 0.3858 |
| F5. EBP Barriers/Facilitators | 0.1104 | 0.001499* | 0.2379 | 0.0004998* | 0.0004998* | 0.0004998* | 0.4683 | 0.2869 |
Fisher's exact test to evaluate association between two categorical variables in a contingency table. P-values less than the established, in this case 5%, suggest that the association between the variables. *Level of significance 5%
Figure 1 shows the classification of individuals into five classes or clusters according to the optimal cut of the dendrogram according to Ward's Criterion. According to the multiple correspondence analysis, it can be generally deduced that the first cluster contains those individuals who present high scores in all dimensions, have Evidence-based practice training, attend university environments, and have a doctorate or master's degree. The second cluster has medium-high scores in the dimensions and average characteristics, and the third, fourth, and fifth cluster has individuals with medium-low and low scores in the dimensions. To define the clusters more precisely, the absolute values of the test values were observed to establish which variables characterized each cluster.
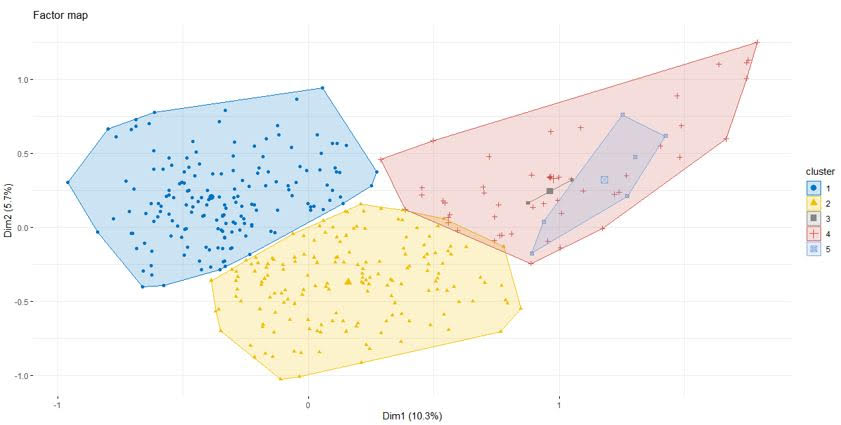
Figure 1 Clusters are formed by the hierarchical method and projected in the first factorial plane. The first cluster comprises individuals with high scores across all dimensions, EBP training, university attendance, and advanced degrees. The second cluster shows medium-high scores and average characteristics. Clusters three, four, and five consist of individuals with medium-low to low scores across the dimensions.
Discussion
The use of the HS-EBP questionnaire in previous studies has shown good reliability, including evidence of content, structural and criterion validity (18,20). However, its use in Latin American respiratory health professionals has not yet been implemented, so the objective of this study was to assess the degree of familiarity with EBM, the frequency with which it is used in clinical practice, the barriers to its implementation, and the most effective strategies for promoting its adoption.
Regarding the sociodemographic characteristics of the health professionals, a more significant number of women were involved, with an average age of 42 years, which clearly shows the increase of women in the high-impact workforce in healthcare organizations, hospitals, and universities. This situation implies essential challenges in the organization of health services 21. These challenges involve ensuring gender equity in leadership positions within the respiratory health field, addressing potential gender biases in recruitment, promotion processes, and recognition and establishing policies that support work-life balance for respiratory health professionals. Therefore, while the increased participation of women in the respiratory health workforce represents progress toward gender equality, it underscores the need for proactive measures to address the multifaceted challenges (e.g., work-life balance) associated with gender diversity in this sector.
Most health professionals have postgraduate studies, which implies an additional interest in additional training in topics related to scientific research and related subjects, facilitating and critiquing scientific articles and making decisions based on evidence 22. However, it is necessary to state that the higher proportion of postgraduate training is particular to the population studied (respiratory health professionals) and may not reflect what happens in all professionals in the region, where postgraduate training remains a development challenge 23.
With the normative data of the HS-EBP at the 50th percentile, factor 1 (9.33), factor 3 (8.6), factor 2 (8.43), factor 4 (8.25), and factor 5 (6. 58), show that the population of Latin American health professionals presents strong positive attitudes and beliefs towards Evidence-based practice (Factor 1), implementation of evidence in daily practice (Factor 3), search for bibliographic evidence (Factor 2), evaluation of the results (Factor 4); at the same time, the lowest values were presented in the perception of organizational factors as barriers or facilitators for the implementation of evidence-based practice (Factor 5). These values are very similar to those reported in other studies conducted on rehabilitation professionals such as physiotherapists in Spain and occupational therapy professionals, speech therapists and physical therapists in Germany 24,25 where health professionals perceive that organizational factors are the main barrier to implementing evidence-based practice 6. It has been described that there are barriers to implementing evidence-based practice when there is no administrative support and it is not visible in the organizational culture, in addition to the deficiencies in the infrastructure and limited resources that added to the educational strategies implemented for learning considerably affect the implementation of the same 26. Based on these results, it could be inferred that if evidence-based practice among Latin American and European professionals involved in our study and other referenced studies is hindered by organizational barriers, addressing these barriers could serve as an initial focal point for improvement initiatives.
Notably, health professionals who do not have postgraduate training and who have not been trained in evidence-based practice have lower scores in all factors, especially in factors 2, 4, and 5, a situation that has been mentioned by other authors who state that health professionals with less training occasionally work in primary care 27 and have more significant limitations in reading and critiquing scientific articles, which affects evidence-based decision making 28. This finding holds for individuals with specialized postgraduate training and those with specific education in evidence-based practice. Even when considering linear regression relationships, it has been demonstrated that their training significantly influences all questionnaire dimensions. This observation underscores the importance of decision-makers within institutions where respiratory health professionals provide services to prioritize access to such training. It's important to clarify that this training isn't always integrated into a formal educational program; however, its inclusion in an institutional educational plan would significantly enhance professional competencies and practices.
The findings of this study allow comparing the scores of each health professional in all dimensions of the HS-EPB, since the percentile distribution of the reference professional can be a point of comparison and in turn, allows obtaining differences in patterns and deficiencies in evidence-based practice according to the health professional or the geographic region of the health professionals 25,29.
In the cluster analysis, a total of 5 clusters were identified in the population of respiratory health professionals. It was found that in almost all the questionnaire dimensions, the results are located in a high score, except for barriers and facilitators, in which the highest proportion is in the medium-high score. This could have several interpretations, and one is that most of the professionals who are dedicated to respiratory health have postgraduate training, which has a strong influence on practice. This situation differs partially from a study conducted in Spain with the same Evidence-based practice questionnaire in physiotherapists. In that study, the results obtained led to the organization of six clusters, one with low scores on all factors, others with low and medium or medium-high scores on the factors and another with high scores on all factors. The difference is that there was no cluster with low scores on all factors in our study, which could be due to the high postgraduate level of the population studied, higher than that of the study here contrasted 25.
It has been identified that there is a positive correlation between postgraduate education and evidence-based practice in different professional areas, including engineering, health, and social sciences. In engineering, for example, studies have found that professionals with graduate degrees are more likely to apply evidence-based practice in their work than those with only undergraduate degrees 30. Similarly, in other professional areas, such as health and social sciences, professionals with graduate education have been shown to have a greater ability to apply evidence-based practice in their work than those with only undergraduate degrees.
These results suggest that postgraduate education may be an important factor in improving Evidence-based practice in different professional areas. Therefore, professionals in different areas need to consider obtaining postgraduate education to improve their ability to apply more rigorous, data-informed approaches 31,32. However, experts in the field suggest that the fundamentals of Evidence-based practice could be taught from the beginning of education similarly, regardless of whether the student is an undergraduate or graduate student, using the concept of "milestones developmental" with a gradual teaching-learning approach that could be achieved throughout the study 33.
In the high-scoring clusters, it stands out that evidence-based practice training transcends the quality of professional practice. Studies have shown that professionals who have received specific training in evidence-based practice are more likely to apply it in their work than those who have not 15,34.
For example, in the field of engineering, it was found that professionals who had received specific training in Evidence-based practice had a greater ability to apply it in their work than those who had not 35. Similarly, in the healthcare field, specific training in Evidence-based practice has been shown to improve the ability of healthcare professionals to apply more rigorous, data-driven approaches in their work 36. It is important to note that specific training not only refers to formal education but also includes on-the-job training and continuing education.
The present study found no relevant differences in Evidence-based practice in the countries with the most responses. In Latin America, Evidence-based practice has gained ground in recent decades, although there is still a long way to go in effective implementation in clinical practice and health decision-making. An increase in the use of guides (GRADE methodology) has been identified in countries such as Colombia, Peru, and Chile 37.
Some initiatives seek to promote the implementation of evidence-based practice in Latin America, such as creating health research networks that seek to strengthen institutional capacity for equity in health research. These networks serve as collaborative platforms, bringing together researchers, healthcare professionals, policymakers, and other stakeholders to exchange knowledge, expertise, and resources. By fostering collaboration and coordination among diverse actors within the healthcare landscape, these networks play a crucial role in advancing Evidence-based practice initiatives 38. However, it is necessary to promote Evidence-based practice in rural and remote areas where access to technology and other sociodemographic conditions affect the institutional capacity of health systems, considerably affecting respiratory health professionals.
As limitations of this study, it is clear that the linkage by the convenience of the participants considerably affects the external validity of this study; however, the strategy of linking the population from the ALAT communication team to its associates, in addition to the dissemination of the questionnaire by different tools such as social, personal and professional networks generated a snowball effect that allowed greater participation of health professionals and that there was a representation of professions such as medicine, physiotherapy, respiratory therapy and nursing located in 8 different countries in Latin America.
Conclusion
This study provides information on the knowledge and application of Evidence-based practice among respiratory healthcare professionals in Latin America. While overall levels of knowledge and application of Evidence-based practice were moderate to high, there is room for improvement, especially in addressing barriers to implementation. The findings highlight the need for specific interventions, such as increased Evidence-based practice training and the promotion of evidence-based practices in clinical settings. These efforts can improve the integration of Evidence-based practice into healthcare practice and improve patient outcomes in the region.











 text in
text in 



