1. Introduction
The human immunodeficiency virus (HIV) produces a progressive deterioration of the immune system in the human body causing immunodeficiency, which causes a deficiency in the fight against diseases, while acquired immunodeficiency syndrome (AIDS) is a term applied to the most advanced stages of HIV infection (WHO, 2022). Globally, AIDS in 2016 alone was the cause of 55.000 deaths in young people, and it has been quantified that every hour, thirty new HIV infections are registered (United Nations International Children’s Emergency Fund [Unicef], 2017). In Mexico, one out of every three people with HIV is unaware they have it, according to the National Center for HIV/AIDS Prevention and Control of Mexico (Centro Nacional para la Prevención y Control del VIH/SIDA [CENSIDA], 2014b). Young people between 18 and 24 years of age are especially vulnerable because HIV is acquired mainly in youth, with a proportion of 33.5% of cases in this age group, as well as 95.1% of registered cases in which sexual transmission is the main route of transmission.
One of the most evident risk behaviors adopted by young people in the exposure to HIV is the lack of correct and consistent use of condoms during sexual intercourse (Hernández-Torres et al., 2019). The National Health and Nutrition Survey of Mexico refers that Mexicans begin sexual life at 17 years of age; 32.4% of those who began sexual life mentioned not using any type of contraceptive method, of which 46.1% of males said they do not like to use them, while 32.8% of females mentioned that they do not agree to use any contraceptive method (Encuesta Nacional de Salud y Nutrición [ENSANUT], 2012). It is important to mention that condoms are currently the main effective strategy to prevent HIV infection (Programa Conjunto de las Naciones Unidas sobre el VIH/SIDA [ONUSIDA], 2015).
Not only condom use is important to review in the sexual behavior of young people, as the literature reports cognitive and behavioral variables involved in sexual risk behavior (SRB), which is defined as the exposure of the individual to a situation that may cause harm to their health or the health of another person especially through the possibility of acquiring a sexually transmitted infection (STI), or generate a situation of unwanted pregnancy (García et al., 2012). Theoretically, there are variables related to SRB, such as those that can be explained through the Integrative Behavioral Model (Eggers et al., 2016; Fishbein, 2000). This theoretical proposal mentions that not feeling susceptible to HIV encourages sexual risk behavior (Fishbein & Ajzen, 2011; Glanz et al., 2008). Attitudes towards safe sex is another variable that is related to SRB: here young people are not able to avoid sexual risks and tend to promiscuity by engaging in sexual encounters without using barrier methods (Bleakley et al., 2011; Eggers et al., 2016). In this sense, the partner support norm for safe sex refers to the influence of friends or family; usually in such influences the first knowledge about sexuality is acquired (Fishbein & Ajzen, 2011). Lack of self-efficacy to negotiate and practice safe sex affects young people because they are usually not able to acquire or purchase condoms and bring them with them for sexual intercourse (Bandura, 1990; Devine-Wright et al., 2015).
On the other hand, knowledge affects young people, as they have problems and errors to use condoms correctly and thus avoid being exposed to HIV infection (Chandran et al., 2012; Coyle et al., 2012; Glanz et al., 2008). The other variable related to SRB is the lack of safe sex intentions; if young people are not likely or disposed to use condoms, they are unlikely to change their risk behavior (Eggers et al., 2016; Espada et al., 2016). It is known that many young people avoid using condoms because they identify barriers to condom use; most notably that when they use condoms they perceive a loss or change in pleasure, sensation or orgasm (Bernard et al., 2013; Geter & Crosby, 2014; Song et al., 2009). Ultimately, the main factor for young people to remain infected with HIV is sexual risk behavior and that is when they do not consistently use condoms in every sexual relationship (Yzer, 2012).
According to international organizations and the National Guide for HIV/AIDS Prevention in Mexico, it has been recommended to address the problem of SRB through effective interventions (Babor et al., 2001; CENSIDA, 2014a; UNAIDS, 2016). An intervention refers to a treatment, therapy, procedure or actions, implemented by health professionals to individuals or clients in a particular situation to bring the person to achieve a desired state of wellness (Sidani & Braden, 2011). Currently, there are interventions of proven effectiveness, such as face-to-face interventions with the use of traditional teaching methods, which have proven effective in reducing sexual risk behavior in young people (Muessig et al., 2013; Rhodes et al., 2007; Schnall et al., 2015; Yzer, 2012).
However, some of the most effective interventions do not have interactive or technological resources (CENSIDA, 2014b; WHO, 2011; Schnall et al., 2015). Based on the Internet Association of Mexico, the internet is particularly well suited for making sexual health promotion accessible to young people, as internet and smartphone use is part of young people’s everyday lives, and there is no other age group today with greater use of these communication platforms than young people (Asociación de Internet [AIMX], 2020). Due to this need, the following study question was posed: What is the effect of Respect M-Health (RMH), a randomized controlled trial, with the use of smartphones to increase safe sexual behavior in youths at risk for HIV? Therefore, we proceeded to postulate the following study hypothesis: young people who participated in RMH reported higher safe sex intentions and safe sexual behavior compared to the control group.
2. Methods
A randomized controlled clinical trial was conducted to evaluate the effect of a smartphone intervention to increase safer sex intentions and safer sexual behavior in youth at risk for HIV, using systematic probability sampling calculated in the nQuery Advisor 7. 0, with a significance of .5, a median effect d = .50, a power of 90% and a non-response rate of 10%, to finally obtain a sample of 154 young people at risk of HIV randomly assigned to two groups, the control and experimental. The estimated effect size was medium because the variables contemplated in the study have previously been reported to have explained variance of the phenomenon of interest with predictive interrelationships (Espada et al., 2016); the participants were recruited in a non-governmental organization (NGO) in the city of Monterrey, Nuevo Leon, Mexico (Cohen, 1988; Grove et al., 2013). Inclusion criteria for the study included young people aged 18 to 25 years, single marital status, having vaginal, oral or anal sexual experience, not having used a condom on any occasion in the last three months, having voluntarily requested a rapid HIV test with a negative result, not living with a sexual partner, and knowing how to open web pages with a mobile device. The exclusion criteria included having participated in a similar study in the last 12 months, being under medical treatment with antidepressants, being a pregnant women, having a positive result to the rapid HIV test, and having plans to have children in the next three months at the time of data collection. Adolescents were not included because in Mexico HIV is mainly acquired in young people, since it is at this age when they acquire greater risks in sexual behavior (CENSIDA, 2014a). A battery of 8 self-administered pencil-and-paper instruments with sufficient reliability and relevance for the purpose of the study was used (see Table 1).
2.1 Procedure
The study was conducted from November 2017 to March 2018. We had the approval of the ethics committee with protocol number 19CEI024201141127, as well as the permission of the NGO for data collection. The Epidat 3.1 program was used to assign the groups to treatment with the random number tool; using a list of appointments, participants were recruited based on the numbers obtained. Facilitators were trained to avoid the principal investigator knowing the group assignment, and they were also trained separately to deliver a counseling model, one using mobile devices (Respect M-Health) and the other without the use of technology. In addition, the facilitators, as well as the participants, did not know in which group they were assigned. This was notified to the participants in the consent form, where it was stated that they could be in any of the groups, experimental or control. Different shifts were managed to avoid contamination among participants and the manuals of the intervention helped to maintain the fidelity of the study and reduce selection bias.
The participants were approached upon arrival at the NGO in the privacy of an office and they were individually invited to participate in the study, a procedure adhered to the General Law on Research on Human Beings (SSA, 1987). Therefore, they were informed verbally and in writing of their right to participate voluntarily and to withdraw from the study at any time without any type of consequence.
The experimental group was given the Respect MHealth intervention with the following measurements: a pre-test at the first contact with the NGO users, a posttest measurement was used at 15 days with respect to the pre-test measurement, and a follow-up measurement was made at 30 days. The control group was given a model of individual face-to-face HIV educational counseling with measurements that were similar to that of the experimental group. The treatment groups were scheduled at different times to avoid contamination between them.
2.2. Development of the Intervention
Respect M-Health is based on an intervention called “Respect”, which is from the Centers for Disease Control and Prevention (Metsch et al., 2013). “Respect” was classified as an effective intervention that was shown to greatly reduce risky sexual behavior in young people attending a sexually transmitted infections diagnostic clinic; a linguistic and cultural adaptation was made to adapt it to the Mexican context, which it was a finalized version of RMH (Hernández-Torres et al., 2018, 2019). It is worth mentioning that the NGO was selected because it had the necessary infrastructure to maintain the control and blinding of the study, and the most important characteristic is that it served 1500 people on average per month, whose visit was mainly to request the rapid HIV test, so it was considered that it contained the target population. RMH is an intervention of two sessions of approximately 30 minutes each with the use of theory and the use of smartphones as a support tool for the development of the intervention (Hernández-Torres et al., 2018). RMH uses the postulates of the Integrative Behavioral Model (IBM) as a basis (Fishbein, 2000; Glanz et al., 2008). As well, it is claimed that a reduced set of variables can explain and predict the safe sexual behavior of young people. The facilitator used manuals to maintain the fidelity of the intervention, including digital cards as a counseling guide (see Figure 1), which allowed to keep track of where all participants were. Based on the last risky sexual encounter of the young person, they were helped to identify through reasoned action aspects of perceived susceptibility to HIV, attitudes towards safe sex, partner support norm for safe sex, self-efficacy to negotiate and practice safer sex, knowledge about errors and problems in condom use, safe sex intentions, and perceived barriers to condom use and safe sexual behavior (Bandura, 1978; Bandura & Bandura, 1994). The counseling was carried out individually, taking advantage of any learning moment where the facilitator helped the young people to resolve cognitive dissonance; to put in order the ideas with the behavior, through the last sexual risk event, The facilitator and participant, common agreement, carried out a risk reduction plan to finally implement it with the help of the prototype mobile application.
Table 1 Measurements
| Factor | Instrument (items) | Cronbach's reliability |
|---|---|---|
| Perceived Susceptibility to HIV | Condom Use Perception Scale (10) | a = .88 |
| Attitudes towards safe sex | Brief Sexual Attitude Scale (20) | a = .95 |
| Partner support norm for safe sex | HIV Social Provision Scale (48) | a = . 94 |
| Self-efficacy to negotiate and practice safe sex | Self-efficacy Scale for AIDS Prevention (23) | a = . 91 |
| Knowledge about errors and problems in condom use | Scale of errors and problems in the condom use (16) | a = . 83 |
| Safe sex intentions | Condom Use Intentions Scale (4) | a = . 88 |
| Barriers to condom use | Sub-scale of perceived barriers to condom use (7) | a = . 86 |
| Safe sexual behavior | Safer sex behavior Questionnaire (16) | a = . 82 |
Note. n = 143.
2.3. Smartphone use
RMH through a prototype mobile application developed focused content for the young person to achieve safe sexual behavior (Hernández-Torres et al., 2019), which is understood as when the young person has a planned behavior of condom use and therefore avoids exposure to bodily fluids, such as vaginal, oral, and anal sex (García et al., 2012). The use of the smartphone was controlled by the facilitator within the counseling, using a manual of the prototype mobile application; the facilitator chronometer the time of use for each participant, and the use of the smartphone was programmed in the digital cards (see Figure 1).
The prototype mobile application was designed and developed in HTML version based theory, where the young person was encouraged to acquire self-efficacy with small successes in behavior modification, because that is how it is built and acquired (Hernández-Torres et al., 2019). At the time of viewing each content and carrying out the risk reduction plan, the participant did not have to download any mobile application. They were also provided with a smartphone only while in counseling to ensure that everyone could access the prototype mobile application contents, which were male condom use, female condom use, how to negotiate condoms, types of condoms, HIV/AIDS information, youth experiences, and the risk reduction plan (one step at a time), as it can be seen in Figure 2 and 3). Each user registered with a personal email address and a unique password for each participant given by the facilitator, which was sent to their email address. The prototype mobile application was monitored by Google Analytics to verify that the young person had actually seen the contents of the prototype mobile application; for the risk reduction plan, a copy was sent to the participant’s email address and the plan was automatically sent to the facilitator’s email address as a follow-up control measure for the second session through the Google Forms platform. The security used in the HTML page was by means of hash encryption and Secure Sockets Layer (SSL).
2. 4 Data Analysis
The statistical analysis was performed by an external expert who had no knowledge of the group assignment, which guaranteed the blinding of the study. The Statistical Package for the Social Sciences (SPSS) Version 20 was used to analyze the data (SPSS 2011). The reliability measure used was 95%, with an acceptable error of 5% and values of p = .05 or lower to determine the significance of the statistics performed. The Kolmogorov Sminrnov Test for Normality with Lillefors correction was used to corroborate the normality of the data analyzed. Descriptive statistics were run for the sociodemographic data and for the study hypothesis, analysis of variance models was performed to compare multiple means (ANOVA), and the differences of the groups were tested using Mauchly’s test of sphericity. It was decided to use the Bootstrap technique for the validation of the repeated measures models, since it is the most appropriate technique, due to the fact that a number of subsamples or resampling by replacement of the original sample is performed obtaining multiple theoretical samples of the population. Therefore, it is ensured that based on a purely mathematical and random method the best estimated coefficients can be obtained, including the expected variability. This technique is useful to make parametric statistical inferences when the assumption of normality has not been obtained. For this reason, it can be said that it is used of robust statistics (Hamaker, 1962). Thus, it is possible to use parametric statistics for the statistical treatment of the study.
3. Results
3.1 Demographics
The average age was 22 years (SD=2.21; min=18, max= 25); 30.1% were female and 69.9% were male. The average formal education was 14 years (SD=3.05; min=6; max=20). The 46.2% were dedicated to work as their main occupation. The majority identified with homosexual orientation (51.7%), as it can be seen in Table 2). On average, the participants initiated an active sexual life at 17 years of age (SD=2.28; min=10; max=23), indicated the mean number of sexual partners in their lifetime (SD=19.96; min=1; max=150), and 25.9% reported having had a previous sexually transmitted infection (STI). The non-response rate was 7.1%, so the final sample was 143 participants.
The Kolmogorov Smirnov Test for Normality reported that there was no normality of the data obtained in most of the study variables (p < .001). The ANOVA test showed evidence of a significant relationship between the intervention type factor Respect M-Health and the factor perceived susceptibility to HIV F (2, 140)= 39.99, (p <.001). There is a main effect due to the difference in the means in the comparison between treatments in the experimental group in the pre-test M=54.93 (SD=1.78), in the post-test M=74.12 (SD=1.60), and at 30 days of followup M=78.0 (SD=1.39), contrary to what was observed in the control group (see Table 3). It is worth mentioning that the differences in the group factor were positively confirmed with Mauchly’s Test of Sphericity (p < .001).
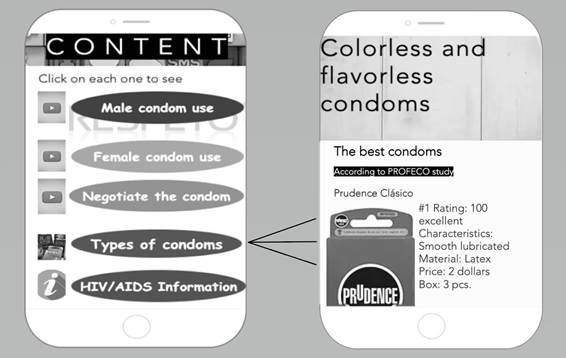
Note. Mobile application prototype interfaces.
Figure 2 Interfaces of the prototype mobile application
Table 2 Sociodemographic Characteristics of the Participants
| Sociodemographic variable | Experimental group | Control group | ||
|---|---|---|---|---|
| Gender | f | % | f | % |
| Female | 23 | 32.0 | 20 | 28.2 |
| Male | 49 | 68.0 | 51 | 71.8 |
| Studying | 22 | 30.6 | 22 | 31.0 |
| Works | 31 | 43.1 | 12 | 16.9 |
| Studying and working Other Heterosexual | 16 3 27 | 22.2 4.1 37.5 | 35 2 20 | 49.3 2.8 28.2 |
| Homosexual | 35 | 48.6 | 39 | 54.9 |
| Bisexual | 8 | 11.1 | 11 | 15.5 |
| Other | 2 | 2.8 | 1 | 1.4 |
Note. f =frequency, %= percentage, n = 143.
The factor type of intervention RMH and the factor attitudes towards safe sex in the ANOVA were statistically significant in the group in which RMH was delivered F (2, 140)=18.74, (p < .001). This experimental group showed a superior effect corroborated by the difference in the means in the pre-test M=46.70 (SD=2.22), post-test M=60.50 (SD=2.15) and at 30 days M=61.05 (SD=2.03), which indicated a greater attitude towards safe sex. The opposite was true for the control group (see Table 3). The group differences were significantly contrasted by Mauchly’s Test of Sphericity (p < .001).
There was also a significant interaction between the type factor intervention RMH and the factor partner support norm for safe sex, as confirmed by the factor model for the young people who received RMH F (2, 140)=16.86, (p < .001). The results indicated a positive effect in those who received RMH, where lower mean scores were observed at pre-test M=23.30 (SD=2.45), post-test M=5.83 (SD=2.18), and at 30 days M=2.63 (SD=1.85). This meant that the lower the score, the higher the perception of partner support for safe sex. No significant changes were observed in the control group (see Table 3). The differences between the treatment groups were confirmed by Mauchly’s Test of Sphericity (p < .001). There was interaction in the factor type of intervention RMH and the factor self-efficacy to negotiate and practice safe sex F (2, 140)=39.12 (p < .001): it was found the effect was greater for the experimental group since the difference in means was significant with at pretest M=67.13 (SD=2.54), post-test M=87.84 (SD=2.37), and at 30 days M=89.90 (SD=2.24), which translates into a higher level of perceived self-efficacy. The opposite case was observed in the control group (see Table 4). Mauchly’s Test of Sphericity (p < .001) confirmed the difference between treatment groups.
In the factor type of intervention RMH and the factor knowledge about errors and problems in condom use, a positive interaction was found F (2, 140)=31.48, (p < .001). the effect of the experimental group was consistent in the pre-test M=20.22 (SD=1.47), post-test M=4.10 (SD=1.36), and at 30 days M=2.31 (SD=1.27), which means that the lower the percentage of errors and problems in the use of condoms, the lower the percentage. The opposite case was found in the control group, where no significant differences were reported (see Table 4). The differences were positively contrasted with Mauchly’s sphericity assumption (p < .001), so the hypothesis of differences was adopted.
For the factor type of intervention RMH and the factor perceived barriers to condom use, a significant interaction was also found F (2, 140)=16.57, (p < .001). The effect was quantifiable in the difference of means in the pre-test M=33.00 (SD=2.86), post-test M=10.61 (SD=2.43), and at 30 days M=7.00 (SD=2.20), which meant that the lower the score, the lower the barriers perceived by the young people who participated in the experimental group. The opposite was observed in the control group, where the effect was not positive (see Table 4). Mauchly’s assumption of sphericity was reported to be significant (p < .001), so the hypothesis of differences was assumed.
In the factor type of intervention RMH and the factor safe sex intentions, the ANOVA resulted with significant interaction F (2, 140)=2.52, (p < .001). The effect of the experimental group was greater as we could appreciate the difference in the means in the pre-test M=78. 50 (SD=3.07), post-test M=94.70 (SD=2.46), and at 30 days M=95.74 (SD=2.29), which can be interpreted as a greater predisposition to use condoms in the young people who participated in the experimental group. This was an inverse situation to what was observed in the control group (see Table 5). The group differences were contrasted with the Mauchly Test, which was significant (p < .001), so the hypothesis of differences was assumed. Finally, the ANOVA for the factor type of intervention RMH and the factor safe sexual behavior resulted with significant interaction F (2, 140)=40.49, (p <.001). the effect of the experimental group was greater reflected in the means at pre-test M=64.80 (SD=1.86), post-test M=85.33 (SD=1.54), and at 30 days M=87.40 (SD=1.52), which indicated that the youth increased condom use statistically significant, and thus avoided CSR. In the case of the control group, no significant differences in the measurements were reported (see Table 5). Mauchly’s assumption of sphericity was significant (p < .001), so the hypothesis of differences was adopted.
Table 3 Differences in Group Measurements per Factor
| Perceived Susceptibility to HIV | Measurements | M | CI 95% | |
|---|---|---|---|---|
| Lower Limit | Upper Limit | |||
| Pre-test | 54.93 | 51.41 | 58.45 | |
| Experimental | Post-test | 74.12 | 70.94 | 77.30 |
| 30 days | 78.01 | 75.20 | 80.71 | |
| Pre- test | 55.01 | 51.42 | 58.51 | |
| Control | Post-test | 50.51 | 47.31 | 53.72 |
| 30 days | 51.60 | 48.78 | 54.32 | |
| Attitudes towards safe sex | Measurements | M | CI 95% Lower limit Upper limit | |
| Pre-test | 46.70 | 42.31 | 51.08 | |
| Experimental | Post-test | 60.50 | 56.22 | 64.74 |
| 30 days | 61.05 | 57.43 | 65.47 | |
| Pre-test | 44.70 | 40.24 | 49.08 | |
| Control | Post-test | 43.67 | 39.33 | 47.91 |
| 30 days | 42.41 | 38.36 | 46.46 | |
| Partner support norm for safe sex | Measurements | M | CI Lower limit | 95% Upper limit |
| Pre-test | 23.30 | 18.41 | 28.115 | |
| Experimental | Post-test | 5.83 | 1.51 | 10.15 |
| 30 days | 2.63 | -1.02 | 6.30 | |
| Pre-test | 23.60 | 18.70 | 28.47 | |
| Control | Post-test | 27.40 | 23.04 | 31.74 |
| 30 days | 24.64 | 20.96 | 28.33 | |
Note. n = 143; M=mean. CI=confidence interval.
Table 4 Differences in Group Measurements by Factor
| Self-efficacy to negotiate and practice safe sex | Measurements | CI 95% | ||
|---|---|---|---|---|
| Lower Limit | Upper Limit | |||
| 67.13 | 62.13 | 72.15 | ||
| Experimental | Post-test | 87.84 | 83.15 | 92.54 |
| 30 days | 89.93 | 85.43 | 94.30 | |
| Pre- test | 66.10 | 61.04 | 71.16 | |
| Control | Post-test | 63.93 | 59.20 | 68.65 |
| 30 days | 65.32 | 60.85 | 69.79 | |
| Knowledge about errors and | Measurements | M | CI 95% | |
| problems in condom use | Lower limit | Upper limit | ||
| Pre-test | 20.22 | 17.31 | 23.14 | |
| Experimental | Post-test | 4.10 | 1.36 | 6.74 |
| 30 days | 2.31 | -.21 | 4.84 | |
| Pre-test | 21.00 | 18.01 | 23.88 | |
| Control | Post-test | 23.44 | 20.73 | 26.15 |
| 30 days | 25.40 | 22.83 | 27.92 | |
| Barriers to condom use | Measurements | M | CI 95% | |
| Lower limit | Upper limit | |||
| Pre-test | 33.00 | 27.32 | 38.64 | |
| Experimental | Post-test | 10.61 | 5.79 | 15.43 |
| 30 days | 7.00 | 2.63 | 11.35 | |
| Pre-test | 37.00 | 31.27 | 42.67 | |
| Control | Post-test | 42.20 | 37.30 | 47.00 |
| 30 days | 43.10 | 38.71 | 47.49 | |
Note. n = 143; M=mean. CI=confidence interval.
4. Discussion
The purpose of the study, which it was to evaluate the effect of the intervention Respect M-Health with the use of smartphones, was found highly effective. One of the specific explanations for this effect is perhaps that the population studied really had the risk of HIV, so it can be said that the recruitment of participants in the NGO, where HIV screening was performed, was evidently correct. This situation is recommended in other studies in which interventions have to target populations where the problem of interest is to measure the impact that occur in the subjects studied (Espada et al., 2016; HernándezTorres et al., 2019; Uribe Alvarado et al., 2017).
With respect to the sample studied, the majority of the participants identified with homosexual orientation, which is a coherent orientation because this group is highly vulnerable to HIV, as it has been empirically confirmed in Mexico, where they are usually identified as at-risk populations (Goldenberg et al., 2015; Oppong Asante et al., 2016; Rushing & Gardner, 2016). The integrative behavioral model was adequate to explain safe sexual behavior in young people. It served as a theoretical guide for intervention, since the elements considered were necessary to produce a positive effect on sexual behavior in young people. This same result was found in other studies where it was concluded that the IBM is one of the main theoretical proposals to study sexual behavior in young people (Eggers et al., 2016; Espada et al., 2016).
With respect to the components of the RMH intervention, perceived susceptibility to HIV, attitudes towards safer sex, and self-efficacy to negotiate and practice safer sex were increased in the experimental group, because the facilitator in the counseling helped the young person to recognize his last sexual encounter, which led to an increase in his own perception of risk. This last situation was consistent with another study where participants perceived an increased risk of HIV infection using the last acquired risk methodology (Bélanger Lejars et al., 2020; Valdez-Montero, 2018). The counseling helped to clarify the moments of dissonance of behavior and misconceptions regarding the use of condoms, as well as to increase their own self-efficacy by making one change at a time, because it is through small successes that self-efficacy can be built and increased. This was also reported in other studies with similar results to the present one, where attitudes towards safe sex and selfefficacy to negotiate and practice safe sex could be increased in young people at risk of HIV (Eggers et al., 2016; Fernández Velasco, 2018).
Knowledge about errors and problems in condom use, safe sex intentions, perceived barriers to condom use, and safe sexual behavior also had a higher effect in the experimental group, because face-to-face contact helped as a strategy for more personalized counseling on the needs of the participants. These factors or variables could be significantly supported with the prototype mobile application, as the participants were able to reduce errors and problems in condom use with the resource of watching the videos of male and female condom use, which was considered a great strategy within the RMH counseling. Also, those who participated in the experimental group had fewer perceived barriers to condom use, because the prototype mobile application had a strategy where participants could access a resource that showed them the best condoms by type, color, flavor, and material, as well as price and packaging data, which made them more likely to bring them with them when needed. This was also found in another study, where similar results were found (Hernández-Torres et al., 2019).
Finally, with respect to the study hypothesis, it is assumed that the young people who participated in Respect M-Health had greater safe sex intentions and greater safe sexual behavior, which is explained by the fact that the participants carried out a risk reduction plan, something that led the participants to acquire a written commitment favoring its realization with the two counseling sessions and the use of smartphones as a successful complement in the modification of the behavior of young people at risk of HIV (Hernández-Torres et al., 2018; James et al., 2021). Finally, some limitations of the study should be assumed. The first is that the follow-up at one month is perhaps premature in intervention studies. Despite its effectiveness, it is necessary to consider for future studies or replications of the same measurements to last 6, 9 and 12 months, in order to corroborate its effectiveness. Another limitation is the lack of a formal mobile application, since the prototype mobile application is considered correct, but it is limited in aspects of control. A future mobile application of Respect
Table 5 Differences in the Group Measurements by Factor
| Safe sex intentions | Measurements | CI 95% | ||
|---|---|---|---|---|
| Lower Limit | Upper Limit | |||
| Pre-test | 78.50 | 78.47 | 84.55 | |
| Experimental | Post-test | 94.70 | 89.83 | 99.57 |
| 30 days | 95.74 | 91.21 | 100.27 | |
| Pre- test | 78.82 | 68.69 | 80.95 | |
| Control | Post-test | 67.00 | 62.08 | 71.89 |
| 30 days | 66.10 | 61.54 | 70.67 | |
| Safe sexual behavior | Measurements | M | CI 95% | |
| Lower limit | Upper limit | |||
| Pre-test | 64.80 | 61.09 | 68.48 | |
| Experimental | Post-test | 85.33 | 82.27 | 88.38 |
| 30 days | 87.40 | 84.34 | 90.36 | |
| Pre-test | 64.43 | 60.71 | 68.15 | |
| Control | Post-test | 60.71 | 57.63 | 63.78 |
| 30 days | 59.90 | 56.85 | 62.92 |
Note. n = 143; M=mean. CI=confidence interval.
M-Health could provide greater consistency in control metrics in the technological use aspect.
5. Conclusion
This study provides significant evidence regarding the use of smartphones to modify sexual risk behavior in youth, because there is currently relatively little empirical evidence of the effect of technology on interventions that address safe sex intentions and safe sexual behavior. Further research is needed to investigate the effects of the use of smartphones to support the change of sexual risk behaviors in the population. It is recommended to continue replicating this intervention, including in knowledge transfer processes to verify its effectiveness.