Introduction
Renal transplant is the treatment of choice for patients with end-stage kidney disease, either because of acute renal failure or secondary to a chronic process1,2. Nowadays, according to the High Cost Account of Colombia, which evaluates the transplant situation in the country, by the end of 2015, a total of 6421 people were transplanted and 11.9 transplants were performed per million people3. In 2011 in France, which is one of the leading countries for kidney transplantation, a total of 47.5 transplants were performed per million people4. Even though there are countries with more experience in these types of transplants, it is a procedure that has become more frequent in our region throughout the years5. In fact, in 2016, an Organ Donor Law was implemented in Colombia (Law 1805), which states that every citizen is an organ donor unless they stipulate their refusal to become one while they are still alive.
As any other procedure, kidney transplant has short- and long-term post-operative complications, some of them associated with the procedure and others with post-surgical care. An example of this is infections that can be associated with the post-surgical-induced pharmacological immunosuppression that is necessary6.
In the last few years, new technologies and surgical techniques have been developed aiming to decrease the frequency of post-operative complications7,9. However, especially urological and vascular complications continue to be a challenge and some of them can compromise the surgical outcome leading to loss of the renal graft or even to patient's death10,11. These complications increase the patient's morbidity and represent elevated costs for the health-care system12.
Reports of the incidence of urological complications after a renal transplant are variable through literature ranging from 3% to 12% of the patients13,14. Some studies such as Streeter et al., described a frequency of 6.5% in a sample of 1535 patients in the United Kingdom15. More recent studies like Choi et al. identified a frequency of 7.7% in 835 patients in Korea16. The urological complication most frequently described is ureteral stenosis, which represents more than 50% of the patients, followed by urinary fístula, urolithiasis, and vesicoureteral reflux17,19. All of them are complications that can be treated if they are correctly and promptly identified6.
Regarding the vascular complications, in a French study that included 312 cases, an incidence of 16% was reported, of which 7.4% were major complications20. Meanwhile another study made in Turkey that analyzed 1843 cases found 2.5% of vascular complications21. The main vascular complication reported is the stenosis of the renal artery, followed by renal vein thrombosis, vascular lacerations, and renal vein or artery torsion21.
However, the studies that have described incidence of complications after renal transplant have been made mostly in Europe or in the United States. We do not have information about the frequency of these complications in Colombia. Thus, taking into account the variability of the data presented in the literature and the lack of local studies in the matter, we considered that it was necessary to perform a study that allowed us to describe the frequency of this type of complications after a renal transplant in our region.
Methodology
A cross-sectional and retrospective study was carried out. It was approved by the San Ignacio's University Hospital Ethical Committee and involved all patients who underwent a kidney transplant from 2007 to 2017 in this specialized center in Bogotá, Colombia.
To collect data, we filtered patients according to inclusion criteria and reviewed clinical records registering information in an Excel database. The purpose of the foregoing was to obtain results of demographic variables such as sex, age of the patient at the time it received the transplant, chronic kidney disease (CKD) etiology, history of any genitourinary disease, and date of the procedure. Furthermore, an evaluation of surgical variables was made, such as surgical time, type of ureteral anastomosis, blood loss, and type of donor. Vascular, urological complications, and infections presented during the first post-operative month were registered, including the isolated microorganism in case of urinary tract infections and if the graft was rejected. We checked the last appointment with the transplant group and measured the time of follow-up. Finally, a data analysis was performed using Excel.
Results
A total of 243 were analyzed, most of whom were male (62.9%). The average age of patients at the time of the procedure was 49.3 years and the principal chronic kidney disease (CKD) etiologies were idiopathic (25.5%), glomerulopathies (24.7%), hypertension (23.5%), urological disease (13.2%), and diabetic kidney disease (10.7%). Most of the patients did not have previous genitourinary disease; however, in those who had, the most common was polycystic kidney disease (5.8%), followed by previous kidney transplant (5.3%).
About 93% of patients received a kidney from a deceased donor and 7% had a living-related donor. The average surgical time was 2 h and 55.2 min, with a minimum time registered of 1 h and 18 min and a maximum time of 6 h. The average blood loss was 223 cc, the least being 20 cc, and the maximum 900 cc. An anti-reflux mechanism was used during the ureter anastomosis in 81.9% of the cases (Table 1).
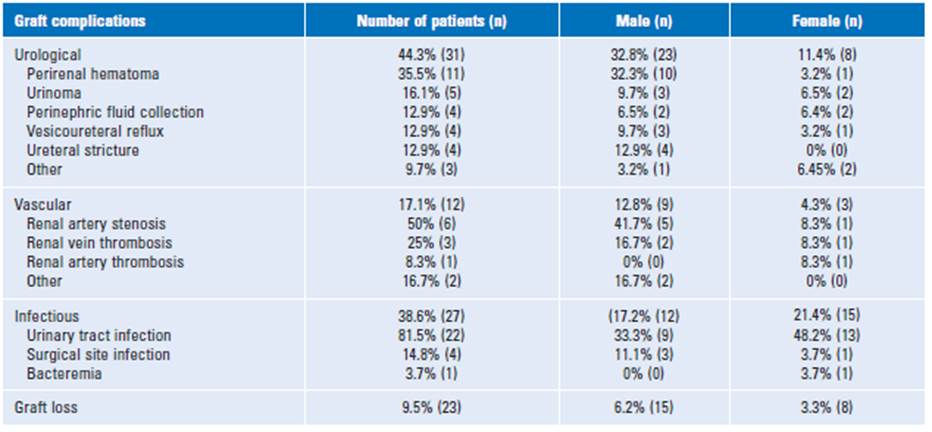
Table 1 Demographic characteristics of the study patients and perioperative outcomes
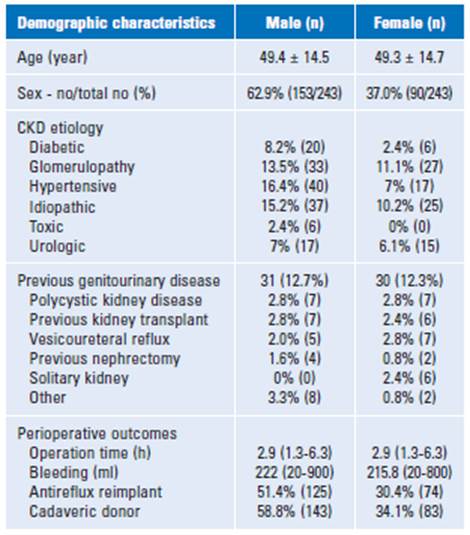
CKD: chronic kidney disease.
Seventy (28.8%) patients presented some type of complication either vascular, urological, or infectious in the 1st month after the renal transplant. Urological complications were identified in 31 (44.3%) patients; being the perirenal hematoma the most common (32.3%), followed by urinoma (16.1%), perinephric fluid collection (12.9%), and vesicoureteral reflux (12.9%). Meanwhile, 12 (17.1%) patients had vascular complications, of which the most frequent was renal artery stenosis (50%).
Infections were identified in 27 (38.6%) cases. The urinary tract infection was the most common (81.5%), followed by surgical site infection (SSI) (14.8%) (Table 2). Of the four cases with SSI, two of them were deep incisional, one of them superficial incisional and only one case had an organ/deep space infection. The most common microorganism isolated in patients with urinary tract infections was Escherichia coli (33%), and other microorganisms found were Enterobacter Cloacae, Citrobacter freundii, Klebsiella Pneumonie, Klebsiella oxytoca, and Morganella morganii. The most frequently found antimicrobial resistance pattern was the extended-spectrum beta-lactamases (ESBL), present in 50% of cases with urinary tract infection (Table 2). About 9.5% lost the renal graft.
Discussion
Over the past few years, studies have shown that urological complications, vascular complications, and infections frequently generate more morbidity and even an increase in mortality in patients with renal transplant22. The prevalence of urological and vascular complications in our sample of 243 patients was 44.3% and 17.1%, respectively, which are similar to the results observed in different studies worldwide that vary between 2.5-30% and 3-15%, respectively12,23.
The main vascular complication in our center was renal artery stenosis, followed by renal vein thrombosis, which has been also reported as the most frequent vascular complications in the literature . Furthermore, some have stated that these patients have a greater risk of graft loss and require more advanced treatment. The most effective diagnostic tool for the detection of vascular complications is the Doppler ultrasound13, and with an opportune diagnosis, interventional radiologists can play a critical role in the rapid percutaneous treatment with a success rate close to 80%23.
Some authors indicate that changes in the surgical technique could decrease the frequency of urological complications23. The main urological complication described in the first 3 months worldwide is ureterovesical junction stenosis and the incidence reports vary between 3% and 8%25. Meanwhile, in our study, the perirenal hematoma was the most common, followed by the urinoma, perinephric fluid collection, and vesicoureteral reflux. The ureteral stricture was only found in three cases, which accounts for 9.2% of the patients with an urological complication and that is considerably lower than the prevalence described worldwide. The diagnosis of this type of complications can be done easily with a urinary tract ultrasound and a percutaneous nephrostomy can maintain an adequate urinary output and avoid graft loss26,27.
In addition, the prevalence of infectious complications was 38.6%, which is higher than the ones reported worldwide that vary between 5% and 12%11. The main infectious complication in our center was urinary tract infection followed by surgical site infection and bacteremia. The most common microorganism isolated in the urinary tract infections was the Escherichia Coli and the antimicrobial resistance pattern identified in 50% of cases was the ESBL12,28. The sonographic appearance of infections and abscesses is variable. On surgical site infection treatment depends on whether the wound infection is superficial or deep, abscesses can be treated with ultrasound-guided or CT-guided percutaneous drainage and usually respond to external drainage and systemic antibiotics 10).
Conclusion
Renal transplant is a frequent surgical procedure worldwide. Colombia has currently seen a significant increase in the number of patients with end-stage CKD, reaching 23,914 in 2014 according to statistics from the National Institute of Health29. In our study, 28.8% of the transplanted patients had a complication in the first month after surgery. The most common complication was perirenal hematoma, followed by urinary tract infection and renal artery stenosis. Although there is great variability in data found in literature, the prevalence of complications found in our center was similar to the reported in several studies.
Advances in percutaneous diagnostic and interven-tional techniques have been constant and, at present, surgical intervention to treat complications can be avoided in many cases10. It is important for medical personnel to be aware of this data to have a high level of suspicion and make an active search, as once these complications occur, the early diagnosis and treatment are crucial to avoid graft loss6.