Introduction
Cancer is considered a multicausal chronic noncommunicable disease and one of the leading causes of morbidity and mortality worldwide. In 2012, the World Health Organization reported that there were 14 million new cases and 8.2 million deaths related to neoplasms. 1,2
In Colombia, the incidence of breast cancer has shown a significant increase, bringing with it social, economic and emotional repercussions. Therefore, this disease requires timely, accurate and coordinated interventions to achieve the expected impact on incidence, disability, quality of life and mortality among the general population and at the individual level. 3,4
Given that the study object of Physical Therapy is "human body movement", this discipline is responsible for the intervention of patients with the conditions described above. Considering that one of the secondary consequences of breast cancer is altered alignment of the shoulder girdle and the surrounding regions -including adoption of antalgic posture patterns due to tumor resection-, it is possible to find a decrease in balance, muscle strength and mobility arches in these patients. 5
This generates a mechanical disadvantage given the changes in the points of support of the respiratory muscle levers that are evident in inadequate posture alignment, impacting global and local stability and mobility, and causing myofascial restrictions, which in turn compromise the respiratory pattern of the patient. In addition, there is central and peripheral fatigue associated with the effects of chemotherapy and radiotherapy treatments, as well as with the muscle catabolism that characterizes this type of patients. 6
Taking into account the conceptual model of mechanical movement dysfunction, it is possible to observe an indirect affectation of the respiratory muscles, especially the diaphragm, which is the main muscle in charge of ventilation: it mobilizes around 70% of the current volume due to its synergic and antagonistic relationship with postural muscles, both at the shoulder girdle and the spine in general. 7 Consequently, these biomechanical adjustments behave as a restrictive pulmonary dysfunction of extrinsic origin. 8
In this regard, it is worth mentioning that any surgical procedure is accompanied by some degree of respiratory dysfunction, even when the lungs are not directly involved; however, pulmonary dysfunction is more common in patients undergoing thoracic surgery. Abreu et al.9 studied the physical, chemical, and functional changes resulting from mastectomy and found that lung function variables and respiratory muscle strength decay are significantly high in the post-operative period. This same study showed a significant difference in maximal inspiratory pressure (MIP) and maximal expiratory pressure (MEP), in forced expiratory volume in 1 second, and in forced vital capacity after surgery. 9
It should be noted that the muscle energy technique (MET) was first implemented by Vladimir Janda in 1989 and formalized by Leon Chaitow in 1991. It is based on the concept of kinetic energy and potential for the patient to perform work with minimal rates of oxygen consumption; professionals seldom use this technique, so it has not been documented in cancer patients.
In this sense, this study aimed to describe the effects on MIP and MEP after using the MET in the quadratus lumborum of patients with stage I and II breast cancer.
Materials and methods
Type of study
Pilot, quasi-experimental study with a pretest-posttest design. The research was carried out in Bogotá D.C., Colombia, in a highly specialized healthcare center, which is a reference center for the management of oncological patients in the city and the country.
Participants
A final sample of 10 patients with stage I and II breast cancer was obtained from an intentional, non-probability sample of patients undergoing treatment at the healthcare center under study.
Inclusion criteria
Patients between the ages of 45 and 75 with preserved and hemodynamically stable higher mental functions, who agreed to participate and signed an informed consent were included.
Exclusion criteria
Recent post-operative patients (1-2 days) who underwent surgery for tumor resection or other condition in the shoulder girdle, and patients with some physical or surgical limitation that prevented the application of the technique were excluded.
Procedures
Physical therapy interventions using the MET in the bilateral quadratus lumborum muscle were developed in three sessions distributed over a week. During the first session, socio-demographic and clinical information was obtained by means of anamnesis and review of clinical history, followed by a physical therapy assessment conducted according to the review by systems and categories proposed by the American Physical Therapy Association. 10 Said categories included: axillary thoracic and xiphoid flow cytometry in sitting position, from residual volume to maximal inspiration, and evaluation of inspiration symmetry by inspection; respiratory rate using a pulse oximeter in resting position; Piper Fatigue Scale for aerobic capacity; pain perception; anthropometric characteristics with weight and height measurement; calculation of body mass index and lymphedema volume; integumentary integrity through skin and adnexa inspection; range of motion with articular goniometry; evaluation of anterior, lateral and posterior postural attitude through observation in bipedal position; and muscle performance with strength test applying Daniels scale. This last category included MIP and MEP measurement.
Lymphedema was measured with a validated and widely used calculator 11, which indirectly calculates the volume in milliliters based on the formula for truncated cones in a macro of Microsoft's Excel program. Estimations were made to find the distance (in centimeters) between the fingers and the wrist, and the wrist and the half of the forearm; arm length and the circumferences of the metacarpophalangeal joints; wrist; half of the forearm; elbow; half of the arm; and 65% of the arm length. It was necessary to measure comparatively the two upper limbs; lymphedema was established when there was a difference in volume of at least 200 mL between the affected arm and the healthy arm.
Aerobic capacity was determined using the Piper Fatigue Scale, a self-report instrument composed of 22 items distributed in three domains (behavioral, affective and sensory/psychological). It has been validated for use in cancer patients from Brazil 12 and in Spanish language. 13
MIP and MEP were measured with a Carefusion MicroRPM® respiratory pressure meter, after calibration and instruction. The procedure followed the steps described by Mora-Romero et al.14, taking the residual volume to obtain the MIP, and pulmonary capacity to determine the MEP. Measurements were made before and after the physical therapy intervention at each session, and the results obtained were recorded in cmH2O, taking the highest of three measurements as the reference value.
The MET was applied to the quadratus lumborum muscles 15; to this end, the patients were positioned on a stretcher in lateral position and with the free arm above the head, reaching the upper edge of the stretcher. The physiotherapist had one hand positioned on the belly of the quadratus lumborum and the other on the lateral edge of the tibia. Patients were asked to perform a hip abduction and adduction movement with the limb extended after hearing the command "bring the hip up and down without bending the knee." This movement was guided by the physiotherapist and ended when the quadratus lumborum was contracted.
Next, with the command "take a breath, raise the leg without bending the knee and keep it up without dropping it," patients, while lying on the stretcher in a lateral decubitus position, were asked to keep the limb elevated for 10 seconds on sustained inspiration; at this point, manual endurance was used at about 20% of muscle strength. After 10 seconds of contraction, the physical therapy specialist, with his fingers intertwined, took the crest of the pelvis and extended it, moving it away from the last ribs and pulling the lower extremity backwards; during this movement the patient made a slow exhalation with pursed lips. During the rest period, the physiotherapist gained amplitude while respecting the patient's physiological limits. This procedure was repeated three times on both sides during each session.
Statistical analysis
Categorical data underwent a descriptive statistical analysis by absolute and relative frequency distribution; quantitative data were analyzed using a numerical analysis of measures of central tendency. With respect to the variable "outcome", the proportional change trend during follow-up was described for the three sessions of physiotherapeutic intervention. Also, the Wilkoxon signed-rank statistical test was performed to determine statistical differences between MIP and MEP measures at the beginning and at the end of the intervention; the level of significance was set at 0.05. Data analysis processing was performed in the statistical program STATA 14.0.
Ethical considerations
This study was conducted according to the agreements of the Declaration of Helsinki 16 and to article 11 of Resolution 8430 of 1993 of the Ministry of Health 17, which establishes the scientific, technical and administrative regulations for health research in Colombia. It was classified as minimal risk research since the data were obtained from secondary sources, i.e., from the clinical history of the healthcare services center, and the intervention also consisted of a common physiotherapeutic assessment and exercise prescription.
Informed consent was required for participation, which was explained and signed prior to taking the study measurements. This research was approved by the ethics committee of the Corporación Universitaria Iberoamericana as stated in Minutes No. 201620D025 of May 31, 2016.
Results
Socio-demographic characteristics showed an average age of 57.5 years with a range between 49 and 71 years, and 90% of the women were under 65 years of age. Most patients were from middle-income households (70%), followed by low-income households; no participants were from high-income households. With respect to the type of health insurance coverage, 9 of the 10 patients were enrolled in the state subsidized health system and 1 paid the treatment in full at her own expense. The type of housing was urban for the entire population.
According to the medical diagnosis, 1 patient was in stage I breast cancer and the right side was the most frequently affected (80%). The evolution time of the medical diagnosis was mostly between 1 and 2 years; only 30% had been diagnosed more than 2 years before the intervention.
Pathological history included conditions such as high blood pressure hypertension (20%), diabetes mellitus (10%) and surgical procedures such as mastectomy (80%). The last dose of cancer treatment was administered mostly less than a year before the intervention. It should be noted that during the study, no patient reported a history of allergic toxicity or was undergoing medical treatments such as chemotherapy, radiation therapy or hormone therapy.
Regarding the clinical laboratory results, the average values of albumin, hemoglobin, leukocytes, platelets and potassium levels were within the normal ranges. However, hemoglobin levels reached values slightly below normal, without reaching critical figures that would influence the intervention described in this study.
The physical therapy assessment found that 20% of the population presented pain in the middle and upper region of the affected breast, with an evolution time of about one month and intensity between 2 and 4 on the Visual Analogue Scale. Moreover, pain increased according to the physical activity levels resulting from the performance of daily activities, and decreased during rest periods. However, the type and origin of pain in one patient was described as localized and muscular, while it was described as irradiated and neurological in another.
In the ventilation and respiration category, all patients had normal chest and oxygen saturation >90% on room air; however, 50% had asymmetric diaphragmatic excursion and 60% had decreased chest expansion (thoracometry <2.5cm). In the aerobic capacity category, according to the Piper Fatigue Scale, half of the patients had fatigue (30% at mild intensity and 20% at moderate; none presented with severe fatigue).
With respect to anthropometric characteristics, a little more than half of the patients were overweight (60%); the majority had grade II lymphedema (70%) in the affected upper limb with an average volume of 2 841.5 mL.
As for posture, an important frequency of alignment alterations was found: hyperlordosis (80%), cervical inclination (90%), protrusion (80%), scapular waist elevation on the affected side (90%), dorsal hyperkyphosis (80%), and scoliosis (70%).
In relation to the ranges of motion of shoulder joints, there was a general decrease, especially on the side affected by breast cancer; however, movements with less impact on the opposite shoulder were extension and internal rotation. Flexion, abduction and external rotation were limited in the entire study population with minimum values close to freezing. The sensation at the end of the movement in the limited ranges was hard (70%) and late (30%) articular end-feel.
The assessment of muscle performance through manual muscle testing using the Daniels-Worthingham scale showed a decrease in muscle strength of the shoulder girdle on the affected side with values of 2-3/5; in contrast, the values were 3-4/5 in the unaffected side, being muscle strength of the contralateral shoulder girdle 1 point higher in all cases. Regarding the quadratus lumborum muscle as the posterior pillar of the diaphragm, it was found that strength before the intervention was rated mostly 2/5, especially on the side compromised by cancer.
After the assessment by categories, the intervention under study was applied to strengthen the quadratus lumborum muscle and to measure the change in MIP and MEP, with an average intensity of 20 minutes and a frequency of 3 sessions. All patients were receiving comprehensive physical therapy intervention focused on aerobic exercise with a frequency of 2-3 times per week and an intensity of 25 minutes on average.
Strength of the quadratus lumborum muscle increased two points in the rating of 50% of the study population; the other half had an increase of one point. It should be noted that the affected side had a lower level of muscle strength in all patients (Figure 1).

Source: Own elaboration.
Figure 1 Quadratus lumborum muscle strength before and after intervention. QL: quadratus lumborum.
The resulting variables showed an increase in their value prior to the intervention. The reference values to determine the percentage of affectation of respiratory muscle strength were taken from the last study developed in Bogotá D.C. by Rodríguez-Medina et al.18 The average MIP was 41% at the beginning of the intervention and 69% at the end, while MEP average was 33% and 51%, respectively.
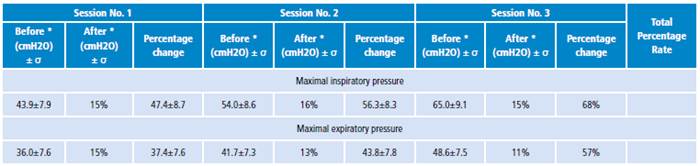
The measurement of MIP and MEP showed positive changes in 30-98% and 24-82% of patients, respectively; the mean change in MIP was 68% and in MEP, 57%. The Wilkoxon signed-rank statistical test was performed, and yielded a statistically significant difference (z= -2.807, p=0.005) between MIP and MEP measures at the beginning and at the end of the physiotherapeutic intervention with MET, specifically in the quadratus lumborum (Table 1).
Discussion
Cancer comprises a group of diseases that have great physical, social, economic and emotional impact. 19 In this sense, and from the perspective of physical therapy, breast cancer patients seek to recover, maintain, potentiate and optimize the functional consequences of local problems (such as pain, lymphedema, scapular dyskinesis, deterioration of respiratory muscle strength) and systemic problems (such as neuropathy, postural alterations and reduction of aerobic capacity and exercise intolerance) that may arise after cancer diagnosis and medical treatment. Different studies have shown that physical therapy can alleviate side effects after treatment, maintain quality of life and improve survival. 20,21
With regard to age, it is known that most cases occur after the age of 40, reaching a plateau in the pre-menopause period-between the ages of 45 and 55-, and with a new peak of incidence between the ages of 75 and 79, being 60 the average age of diagnosis. 22 This information coincides with the results found in this study, where the average age was 57.5 years, with a range between 49 and 71 years; however most of the intervened patients were less than 65 years old.
Pain was a symptom reported in only 20% of the patients included in the research, and it was nociceptive or neuropathic, located in the affected breast with an intensity variation of 2-4/10. This coincides with Smoot et al.21, who describe that pain after surgical and/or medical treatment affects 20-75% of patients and is mainly related to neurological, lymphatic and musculoskeletal damage and infectious and inflammatory processes.
Other relevant findings in the population studied are restrictive pulmonary dysfunctions -caused by musculoskeletal adjustments of the rib cage-, pain in local and underlying regions, and postural changes and effects on the pulmonary parenchyma by pharmacological treatments. Previous studies have shown that in relation to inadequate postural alignment -specifically in the shoulder girdle-, this type of patient and people with cervicalgia present alterations in the mechanics of the thorax, in the capacity for maximal inspiration, and in respiratory muscular strength. 9,23 This work found similar data with an important amount of patients with asymmetric diaphragmatic excursion in the hemitorax of the affected breast, and reduction of expansion with flow cytometry <2.5cm in more than half of the study population; still, there are no recent reference values of this test nor measures in similar populations.
The study by Beleza et al.24 found that the main postural alterations in patients with breast cancer were anteriorization and left rotation of the head, elevation of the affected shoulder, elevation and anteversion of the pelvis, and inclination of the left trunk. 24 This study found comparable results at the level of the pelvic and scapular waist, as well as deviation of the spine in the frontal plane, but results contrary to the increase in dorsal kyphosis and protrusion of the shoulder on the compromised side.
Deficiencies in the ranges of motion of shoulders generated by the alteration of connective tissues and joints as a consequence of cancer treatments were also evident. In this respect, the systematic review of Levangie & Drouin 25 concluded that the main movements affected were flexion, abduction and external rotation, as well as close grip and push-ups movements in the affected upper limb, which has a negative impact on the functionality and quality of life of these patients. The most reduced joint movements were almost the same in this study, with less impact on the extension movement and internal rotation; similarly, the cited research found that studies report limitation in the shoulder contralateral to breast cancer, although with less reduction of the arc of motion. 25
Furthermore, the patients included in this study presented decline in muscle performance with a decrease in the rating of ipsilateral upper limb strength on the side of the affected breast with values 2-3/5 and 3-4/5 on the opposite side. Lee et al.26, in a systematic review, reported muscle weakness in the arms in between 9% and 28% of breast cancer patients, associated with restriction of shoulder movement, presence of pain and lymphedema. With respect to the latter, it was found in the entire population, with a higher incidence of type II lymphedema (70%). According to Smoot et al.21, this has been found in about 10% of patients who had surgical mastectomy treatment alone, of whom 42% also underwent radiation therapy, and in up to 58% of breast cancer survivors. 21
Cancer-related fatigue is described as one of the most common symptoms of these patients before, during or after medical and surgical treatment, with an important impact on functionality, independence and, therefore, quality of life. This condition occurs with a frequency between 15% and 99% 27, range consistent with the prevalence found in the present study (50%), where three patients were classified with mild fatigue and two with moderate fatigue, according to the Piper Fatigue Scale.
About quadratus lumborum muscle and respiratory muscles performance, a decrease in this category was found in the patients evaluated; it was observed in most quadratus lumborum ratings, which were 2/5, denoting muscle weakness and decreased pre-intervention MIP and MEP values with respect to the reference value. Similarly, research by Abreu et al.9, performed on breast cancer patients before and after mastectomy, showed that the previous MIP and MEP were was 43% and 40%, respectively, dropping significantly after surgery. In addition, there was a significant decline in post-operative lung function (forced expiratory volume in 1 second, forced vital capacity and peak expiratory flow).
The present research sought to determine the effects of the use of MET in quadratus lumborum muscle on MIP and MEP in patients with stage I and II breast cancer, finding a statistically significant increase (p<0.05) in respiratory muscle strength. No previous studies have evaluated this topic to date; however, this technique has shown positive effects in other populations and body segments such as increased muscle flexibility 28-30, range of motion 31,32, muscle pain 33,34 and postural alignment. 35 Even so, it should be noted that similar manual therapy techniques applied to the chest, diaphragm muscle, and spine have shown improvements in chest mobility, lung volumes, and respiratory muscle strength. 36-38
This observed improvement has been conceptualized in two fundamental aspects: 1) the actions of the quadratus lumborum muscle in both phases of ventilation, which stabilize the posterior crura of the diaphragm during inspiration, while forced exhalation is assisted given its points of insertion in the lumbar spine and in the last rib 15; and 2) the effects of the technique on muscles and posture, which impacts the segmental and multisegmental movement restriction zones, as explained by the mechanical movement dysfunction model 39, thus improving the mechanical advantage of the breathing muscles and, therefore, their performance.
One of the strengths of this study is that it was carefully applied including data quality control. In addition, the currently accepted international classifications for variable measurement and low percentages of missing data were followed. Moreover, the database was constructed by the researcher, and the measurements and interventions were made by an expert in the area (physical therapy specialist with a master's degree in neuromusculoskeletal physiotherapy), which reduces the probability of information biases.
It should be noted that no research has evaluated the effects of this technique on cancer patients, specifically breast cancer patients, which makes relevant the conceptual contribution of this research to oncologic physical therapy, and opens gaps in knowledge that encourage further research on the matter.
The weaknesses of this work is its small sample size, which made difficult estimating some statistical tests and stratifying the independent variables according to the result variables. Similarly, there was no control group that allowed comparing the results of the treated patients, since few met the inclusion criteria established by the healthcare center during the study period.