Introduction
Professional burnout is a syndrome linked to chronic unresolved workplace stress in professionals who have a constant and direct relationship with other people in their work environment, and is associated with how they perceive and maintain their well-being in times of crisis.1 Likewise, burnout is considered an occupational phenomenon resulting from prolonged exposure to work-related emotional stressors;2,3 it has been widely studied due to its implications both in the workplace and for workers' health condition (in particular in health care working environments).
According to the World Health Organization (WHO),2 burnout, as defined in the ICD-11, is characterized by three dimensions: emotional exhaustion (feelings of energy depletion), depersonalization (increased mental distance from one's job or job-related negativism), and personal accomplishment (reduced professional efficacy).2,4 In this sense, it can be associated, on the one hand, with physical exhaustion, anxiety, depression, and low self-esteem, and, on the other, with reduced job performance, absenteeism, desire to resign, and decreased personal satisfaction.3
Burnout syndrome is more prevalent in individuals with highly demanding jobs or jobs that require caring for other people such as social workers, teachers, and health care personnel.5 Medical residents engage in highly demanding work-related activities during their training time (3 to 5 years), and are subject to great physical and psychological demands resulting from long working hours in health care centers. In addition, they must have an excellent job performance while meeting high academic standards of residency programs. Thus, due to the academic activities they must engage in, the physical exhaustion derived from patient care-related activities, and the high emotional burden caused as a result of performing these activities, residents are considered to have a higher risk of developing burnout syndrome.5
Worldwide, several studies on burnout syndrome in residents from different medical specialties have reported prevalence rates that range from 28 to 74%, and have described multiple factors that may be associated with the occurrence of this phenomenon, including marital status, having children, excessive working hours and general workplace-related dissatisfaction.6-11 In addition, a meta-analysis recently conducted highlights there is a knowledge gap in international literature regarding the influence of socioeconomic factors in burnout syndrome development, as well as regarding its behavior in developing countries and emerging economies.12
In the case of Colombia, several studies addressing burnout in medical residents have been conducted; for example, in 2008, Paredes & Sanabria-Ferrand11 reported a burnout prevalence of 12.6% in 138 residents from different medical residency programs, which was mainly associated with the deterioration of their psychological well-being due to working long hours. It is worth noting that these authors did not find any significant association between burnout occurrence and any sociodemographic and workplace-related variables.11 On the other hand, in 2017, Dominguez et al.,13 in a study conducted in Colombian general surgery residents, reported a nationwide burnout syndrome prevalence of 33.15%; besides, they also found a higher prevalence in residents enrolled in programs offered in the Andean region of the country. In addition, similar to the findings of Paredes & Sanabria-Ferrand,11 no correlations between burnout syndrome occurrence and different variables (age, sex, type of residency program, residency year) were found.13
Medical residency management and financing has been approached differently by Latin American countries.14 In Colombia, Law 100 of 1993 dictates the offer of limited government funded scholarship-loans to finance some medical residents' living expenses.15 Nonetheless, as stated in 2013 in a report by the Ministry of Health, market pressures throughout almost 30 years of implementation have increased training costs, which are ultimately assumed by medical residents as tuition fees.16 This state of affairs has the potential of further widening the extant economic inequality in the country as access is restricted to students hailing from backgrounds without sufficient financial capabilities.17 This situation stands in stark contrast with other countries in the region, where, according to a 2011 Pan American Health Organization (PAHO) study, monthly salaries range from $212 up to $2000 United States Dollars (USD).14
Several studies conducted in the region have highlighted the potential role financial stress may play as an aggravating factor for physician burnout, especially since residents resort to working additional shifts to make ends meet, which adds to the detriment of the quality of care provided by them and their learning capabilities.18-20
No studies on factors that go beyond the residency programs characteristics, and that may be associated with having a higher risk of developing burnout syndrome, such as paying the residency program tuition fees, have been conducted so far. Thus, the present study aims to measure burnout syndrome prevalence in residents enrolled in the residency programs offered by the School of Medicine of a Colombian public university, and to identify a possible association between burnout occurrence and specific socioeconomic factors.
Materials and methods
A cross sectional study was conducted in a population consisting of all residents enrolled for at least 6 months in the clinical and surgical residency programs offered by the School of Medicine of a public university in Colombia, who were, on the one hand, administered the Spanish version of the Maslach Burnout Inventory - Human Services Survey for Medical Personnel (MBI-HSS MP) validated for Colombian population,14 and, on the other, asked to provide their demographic and socioeconomic data through a survey created by the research team. The survey included questions about each resident's age, city of birth, year of specialty, amount of hours worked weekly, how were their studies being financed, whether they had any economic responsibilities, whether they had had to work additional jobs during their training, and if their funding was enough to finance their studies. These questions were preferred over others in order to generally address the financial situation of each resident in relation to their postgraduate studies.
Participants
All residents enrolled for at least 6 months at the time of conducting the study in medical specialty programs offered by the School of Medicine of a Colombian public university were included (n=324). Due to the inapplicability of the depersonalization dimension in medical specialties that don't require physician-patient interactions, residents enrolled in said residency programs were excluded (n=7). In addition, residents who were not available at the moment of survey administration (n=37) and those who submitted incomplete surveys were excluded (n=11), resulting in a total of 55 residents being excluded.
Instrument
The MBI is the leading instrument to measure burnout. The MBI-HSS MP is an MBI variation specifically designed to measure burnout in medical personnel; it is composed of 22 items presented as affirmative statements. The instrument is divided into 3 subscales that asses each of the three dimensions of burnout syndrome (emotional exhaustion, depersonalization, and personal accomplishment). As mentioned above, the Spanish version of the instrument validated in Colombia was administered to participants.21 Having high scores in the depersonalization or emotional exhaustion sub-scales was used as a diagnostic criterion for burnout syndrome, given their capacity to clinically distinguish burnt out from healthy subjects.22 In addition, burnout syndrome prevalence was also estimated by establishing a diagnosis based on the following conditions: 1) having a high score in the emotional exhaustion sub-scale, and 2) having a high score in the depersonalization subscale or a low score in the personal accomplishment subscale. Nevertheless, all correlations were calculated using the burnout syndrome definition widely accepted and mentioned above.
Ethical considerations
The study was granted ethical approval by the Research Ethics Committee of the School of Medicine of the Universidad Nacional de Colombia, as stated in Minutes No. 008-093-19, issued on May 10, 2019. In addition, the ethical principles for medical research involving human subjects established by the Declaration of Helsinki23 and Resolution 8430 of 1993,24 issued by the Colombian Ministry of Health, were followed. Likewise, all participants were asked to sign an informed consent form. Based on the ethics committee recommendations, anonymity was not maintained since it was necessary to continuously interact with the at-risk personnel to give feedback based on the findings and to offer them options.
Procedure
Participants were administered the survey and the instrument in the first semester of 2019 in two stages. In the first stage, members of the research team administered the instrument and the survey to residents attending monthly or biweekly meetings arranged by each medical specialty program. In the second stage, the chiefs of each residency program helped administering the survey and the MBI-HSS (MP) to those residents who did not attend the abovementioned meetings. Surveys with no sociodemographic data were labelled as incomplete and were excluded from the study.
Data analysis
Participants' demographic and socioeconomic data were entered into a Microsoft Excel 2016 spreadsheet. Statistical analysis was performed using Stata v14 software. All data were analyzed using descriptive statistics. Associations between socioeconomic data and the MBI score were determined using the chi-square test. The association between the presence of burnout (defined as having high scores in the depersonalization or emotional exhaustion subscales) and sex, being enrolled in a clinical specialty vs being enrolled in a surgical specialty, and data on the financial situation of residents were analyzed through the calculation of prevalence Odds Ratios (OR). With this in mind, residency programs were classified into two groups: clinical (aerospace medicine, endocrinology, dermatology, forensic medicine, geriatrics, physical and rehabilitation medicine, internal medicine, sports medicine, neuropediatric, ophthalmology, pediatrics, psychiatry, radiology, and neurology) and surgical specialties (urology, otolaryngology, pediatric surgery, plastic surgery, general surgery, orthopedics, neurosurgery, gynecology, and anesthesiology). P-values <0.05 were considered statistically significant.
Results
280 surveys were collected. After incomplete surveys were excluded, the final population included for statistical analysis consisted of 269 residents, that is 83.2% of the total population (N=324). Unfortunately, not all respondents answered all socio demographic questions. Taking this into account, of the total sample, 162 were men (60.22%) and 106, women (39.41%); 1 person did not mark any of the options (n=269). Participants' demographic and socioeconomic data are summarized in Table 1.
Table 1 Main demographic and socioeconomic characteristics of the study population.

x̄: mean.
NR: Non responder; IQR: Interquartile range.
*Several options could be chosen.
† Non responder.
Icetex: Colombian institute responsible for awarding educational scholarship-loans.
Source: own elaboration based on the data obtained in the study.
Figure 1 shows the distribution of residents included in the study per specialty program.
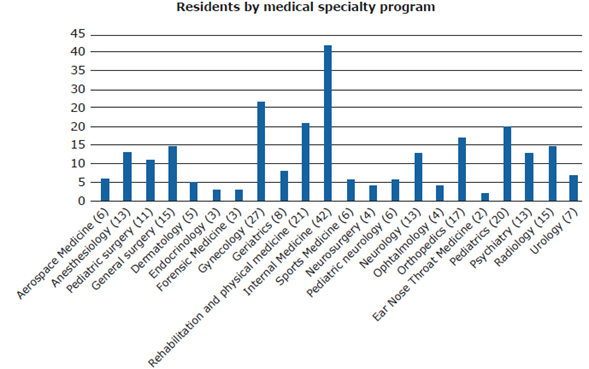
Source: own elaboration based on the data obtained in the study.
Figure 1 Distribution of residents per residency program.
Considering the possible presence of stressors, participants were also asked about important events experienced by them over the last 6 months prior to collecting the data. In this sense, 28.62% (n=77) had recently experienced life changing events, being the most common those involving emotional (relationship) problems and having relatives with health problems.
Another variable assessed was their perception of physical health deterioration over the last 6 months. In this regard, 37.55% (n=101) reported having visited a medical service for consultation or having experienced symptoms related to different diseases; of these, 14 had visited medical services due to having emotional symptoms (anxiety, mood impairment, among others); 12 reported unspecific symptoms (exhaustion, muscle tension); 10 had suffered headaches or experienced a worsening of their migraine symptoms; 10 had acquired infectious diseases; 9 had experienced sleep problems (insomnia, unsatisfying sleep, nightmares); 8 reported having or having had muscle pains (lumbar pain, cervical pain); 1 had weight problems, and 31 reported other unspecified reasons of consultation; 6 did not provide information in this regard.
Regarding the MBI-HSS, the distribution of scores across all the population surveyed and divided by gender is shown in Table 2. Compared to female, male sex was found to be associated with moderate scores in the depersonalization subscale (OR:1.89, CI:1.08-3.3). No other association or difference was observed between sexes.
Table 2 Maslach Burnout Inventory - Human Services Survey subscales scores by sex.

* Chi-squared test.
Source: own elaboration based on the data obtained in the study.
When proportion comparison analysis using the chi-squared test was performed for each subscale of the MBI-HSS, a greater proportion of subjects with a high or moderate score in the depersonalization subscale was found in the surgical specialties group compared to the clinical specialties group. This association was statistically significant, as shown in Table 3. No significant differences were found between surgical and clinical specialties regarding the personal accomplishment or the emotional exhaustion subscales scores (p=0.242 and p=0.323, respectively).
Table 3 Maslach Burnout Inventory-Human Services Survey for Medical Personnel subscales scores per specialty group.

Source: own elaboration based on the data obtained in the study.
Burnout syndrome prevalence in the study population was 39.78%, and no significant differences between men and women were found. It should be noted that this prevalence is obtained when burnout is defined as having high scores in either the emotional exhaustion or the depersonalization dimensions of the MBI-HSS MP; if the more specific burnout criteria stated in the methodology section of this paper is used, burnout prevalence decreases to 15.99%, without significant differences between men and women, as shown in Table 4.
Table 4 Burnout syndrome prevalence in the study population based on the adopted definitions.
| Men (n = 163) n (%) | Women (n = 106) n | Total n(%) | p-value ‡ | |
| Burnout prevalence * | 62 (38.04) | 45 (42.45) | 107 (39.78) | 0.470 |
| Burnout prevalence (alternative definition) † | 27 (16.56) | 16 (15.09) | 43 (15.99) | 0.748 |
*High emotional exhaustion or high depersonalization scores.
† High emotional exhaustion and high depersonalization or low personal accomplishment scores.
‡ Chi-squared test.
Source: own elaboration based on the data obtained in the study.
If the first definition is considered, then burnout syndrome occurrence is positively associated with lacking enough funds to pay medical specialty training associated costs (OR: 3.45, CI:2.04-5.82); having experienced recent life changing events in the last 6 months (OR: 1.84, CI:1.07-3.14); and having had any health issue in the last 6 months (OR: 1.81, CI:1.09-3.01) (Table 5), and negatively associated with having been awarded a scholarship-loan. No significant statistical differences were found regarding age, sex, residency year and participation in artistic or sport activities.
Table 5 Burnout syndrome prevalence according to the selected variables.
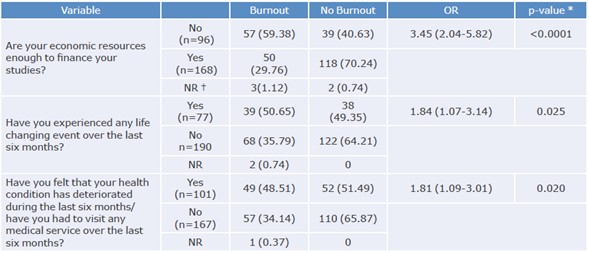
*Chi-squared test.
† Non responder.
Source: own elaboration based on the data obtained in the study.
On the contrary, when using the second definition, burnout prevalence was slightly higher in residents who claimed they had not enough money to pay for their residency training, but this difference was not significant. Finally, a variance analysis was conducted in order to identify whether the scores obtained in each of the three subscales of the MBI-HSS MP were associated with the hours per week that residents devoted to their specialty training or not; however, no significant differences were found.
Discussion
Burnout prevalence among the study population was 39.78%. In residents who stated they did not have enough financial support to fund their tuition fees and residency-related costs, the chance of developing burnout was 3.45 times higher compared to their wealthier counterparts (CI 95%:2.04-5.82, p<0.0001).
The burnout prevalence observed here is similar to the findings of Domínguez et al.,13 who found a prevalence of 33.15% in a nationwide study conducted in Colombian surgical residents, and Rodrigues et al.,25 who conducted a systematic review that included 4664 residents and reported an overall burnout prevalence of 35.7%. On the contrary, Paredes & Sanabria-Ferrand,11 in a study conducted in 2008 in medical residents of Bogotá, Colombia, reported a burnout prevalence of 12.6%, which is significantly lower than the values found in the present study, yet this significant difference could be explained by the fact that several modifications have been made in relation to burnout diagnostic criteria since the publication date of said study.
On the other hand, in a systematic review carried out by Low et al.12 in 2019 and that included 22778 residents from different countries, burnout prevalence was 51%, which is significantly higher than the prevalence reported here or in the study by Rodrigues et al.25 This difference could be attributed to using different burnout diagnostic criteria, as the criteria used by Low et al.12 differ from those used here, which in turn are similar to those considered by Rodrigues et al.,25 which might explain why the burnout prevalence reported by the latter is similar to that found in our study.
In the present study, burnout prevalence was greater in residents enrolled in surgical specialties, as high scores in the depersonalization subscale were more frequent in this group, which differs from the findings by Low et al.,12 who reported that burnout prevalence was similar in clinical and surgical specialties. However, no significant differences were found between both studies regarding the scores reported for the other two subscales. On the contrary, in the systematic review conducted by Rodrigues et al.,25 although medical specialties were not classified as clinical or surgical, when residency programs were divided into three groups according to burnout syndrome prevalence levels, the high prevalence group (42.5%) was composed mainly of surgical specialties (general surgery, anesthesiology, gynecology and orthopedics). Similar to what has been reported in other studies,11 a higher prevalence of burnout syndrome was not associated with sex or age.
Financial pressures have been previously described as being correlated with physician burnout by studies conducted in USA and Canada, where physicians in training are likely to accrue significant debts.17,26-28 In Latin America, two studies conducted on medical students in Brazil highlighted the association between access to scholarships-loans and psychological stress.29,30 Despite this evidence, burnout syndrome and its association with financial concerns of residents in other countries of the region remain mostly unexplored.
In the present study, burnout occurrence was positively associated with having insufficient funds to pay residency training associated costs. Nonetheless, the fact that burnout was still found in 29% of residents stating they had enough resources to finance their studies, highlights the multifactorial nature of this syndrome.
The association between lacking enough funds and high burnout prevalence27 is of great importance in the case of Colombia, since, despite the passing of Law 1917 of 2018,31 which stablishes that physicians enrolled in residency programs offered in the country must be paid no less than three minimum wages per month (as of December 2020, the minimum wage in Colombia was COP 877 803, approximately USD 252.99) for their work, currently most of them are not paid as said obligation will be fully in force until the second semester of 2021.
One of the limitations of the present study was the current lack of universal diagnostic criteria for burnout. This syndrome is best described as a multidimensional continuum in which emotional exhaustion, depersonalization or cynicism, and a perception of reduced professional inefficiency or lack of personal accomplishment are present.4,32,33 Thus, the MBI creators have recommended to approach it from these three dimensions, however up to 47 diagnostic criteria have been proposed for studying burnout syndrome.21 Due to this situation, in the present study burnout diagnosis was made based on two diagnostic criteria proposals, both suggested by Maslach et al.,33 as described in the methodology section: having a high score in the emotional exhaustion or depersonalization subscales, or having a high score in the emotional exhaustion subscale plus a high score in the depersonalization dimension or a low score in the personal accomplishment subscale. This way, burnout prevalence in the study population varied depending on the criteria used for diagnosing it, as its prevalence was 39% when the first criteria proposal was used, and 15.99% when the second one was used.
On a separate note, it should be noted that this study was carried out only in residents enrolled in programs offered by a public university. This could limit the external validity of our findings as residents enrolled in private universities, which usually charge considerably costlier tuition fees, may be subject to different financial pressures, and consequently burnout prevalence may also differ, so further research is required.34
Another limitation was the study design, besides the usual biases to which survey-based studies are subject to. Given that this was a cross-sectional study, establishing a causal relationship between the observed events was not possible, yet the findings reported here can be used as a basis to formulate new hypotheses on burnout syndrome occurrence in medical residents that may guide future studies conducted in this population.
Conclusions
Burnout is a prevalent condition in the residents who took part in the present study. However, the criteria for diagnosing burnout syndrome have not been clearly defined so far, and therefore its prevalence varies depending on said criteria; in fact, in the present study burnout prevalence varied significantly when using two different diagnostic criteria proposals.
Residency programs should be alert to the widespread problem of burnout in residents and undergo appropriate modifications aimed at ensuring the safety and well-being of residents and, thus, their patients. Reducing the cost of tuition fees or providing residents with salaries may be adequate initial measures, although they may not prove themselves cure-all solutions in the long run. The answer to the problem of how to achieve an adequate balance between working hours, learning opportunities, residents' health and patients' safety remains elusive.
















