What do we know about this topic?
• Suicide among anesthesiologists has been thoroughly described and is a relevant issue in terms of the quality of life of these practitioners.
• Mental health of healthcare practitioners tends to be disregarded, notwithstanding the existing awareness of the ongoing stress to which healthcare professionals are subject to.
What is the contribution of this study?
• An indirect characterization of suicide among the Colombian anesthesiologists has been conducted, a determination of the characteristics of the victims and the support offered following the event.
• This study illustrates the opinion of the colleagues who witnessed this situation.
• Recognizing the problem is the first step to acknowledge its significance in order to generate the support mechanisms that many anesthesiologists require on a daily basis.
INTRODUCTION
Suicide represents an important cause of mortality among physicians, with a higher risk of death as compared with the general population. 1 In contrast to other professions there are different factors involved, including access to certain drugs, knowledge about their doses and use, in addition to the exposure to highly stressing situations that represent and additional risk factor. 2. This group comprises the anesthesiologists in whom an incidence of chemical substance abuse of around 1% 3 has been identified, and a risk of suicide of up to 50 % or higher, in contrast other specialties, such as internists. 4
There is a growing interest on the impact of stress and work overload on the mental health of anesthesiologists and the suicide issue is one of the most concerning situations. In contrast to the general population and other medical specialties, the risk of suicide among anesthesiologists seems to be higher, probably due to the high level of stress associated with the specialty, including the care of high risk patients in work environments with complex and highly demanding situations 5; other risk factors mentioned in the literature include the high prevalence of Burnout syndrome among anesthesiologists, and the relative isolation inherent to their daily practice. 6) A systematic review conducted by Plunkett et al. 7, indicates that suicidal ideation among anesthesiologists ranges between 3.2 % and 25 %, and suicide attempts range from 0.5 % to 2 % in various studies. The authors further state that the risk of an anesthesiologist dying as a consequence of suicide is consistently high as compared to other groups.
Data from the Latin American Confederation of Anesthesiology Societies (CLASA) published in 2013, indicate that in around 10 years, 141 deaths of anesthesiologists have been reported in Latin America, associated with suicide or overdose. (8 A more recent study considered the frequency of suicidal ideation among anesthesiologists in a Brazilian State, and found that 14.59 % of the respondents had experienced suicidal ideation associated with stress, depression, and use of anxiolytics or antidepressants. 9 In Colombia there is still limited evidence about suicide among anesthesiologists and the impact of the suicide of a colleague on the department of anesthesia; the resources available to deal with the situation are unknown.
Recently, the Association of Anaesthetists of Great Britain and Ireland organized a work group to review the problem and provide guidance to anesthesiologists, their anesthesia departments and their employers. To support this work, they administered a survey to anesthesiologists in the United Kingdom and Ireland on the support that their institutions provided in case of mental illness, addiction and suicide; additionally, the survey asked associated anesthesiologists working anywhere around the world, about their experiences regarding suicide of colleagues, including the support available at that moment and any changes introduced as a result of such event. 4
The Colombian Society of Anesthesiology and Resuscitation (S.C.A.R.E), through the Occupational Health, Wellbeing and Safety Committee, aware of the significance of this problem and with the authorization of the authors, decided to administer the same survey in Colombia, in order to indirectly learn about the frequency of suicide among Colombian anesthesiologists and the experiences related with the suicide of a colleague.
METHODS
A survey-based cross-sectional observational study was conducted. This survey was sent by e-mail to the members and those interested in participating expressed their agreement in the informed consent attached at the beginning of the survey. The participants included were the Colombian anesthesiologists members of S.C.A.R.E. that agreed to participate in the study; the answers of the participants expressing their wish to be removed from the study were excluded. The total membership was 2,936, so the calculated sample size was based on a 50% frequency with 80% power and a 95% confidence level. The estimated sample size was 340 anesthesiologists.
The instrument used was the same instrument used by Yentis et al. in the United Kingdom, with the authorization of the original authors. Such instrument is a questionnaire of 19 questions about the knowledge of the participant regarding the available support in the workplace with regards to mental health, addiction and/ or suicide, the experience with the suicide of a colleague, and the assistance provided during the event. 10 The instrument is not validated in Spanish and the validation process of the English version is not formally reported. However, the decision was made to use this questionnaire since no other instruments with the same objective and validated were identified. The rationale was that the results could then be compared at least with the results obtained in the UK. The validity of this questionnaire is still being discussed.
The survey was forwarded via e-mail on September 26, 2020 to all the anesthesiologists using the QuestionPro platform; the survey was sent a second time on October 3, 2020 to those that had not yet completed the survey, with the intent of gathering the largest possible number of respondents. Only one response was allowed per participant. The information obtained from the platform was exported in an Excel format which was then uploaded to STATA V13 for analysis. A descriptive analysis was conducted and the qualitative variables were expressed as proportions.
The development of the project was supported by a psychiatrist who made suggestions and advised the work team while the project was underway. This study was reviewed and approved by the Bioethics Committee of the School of Health Sciences of Universidad de Caldas, on June 11, 2020, under reference CBCS-043. An informed consent was attached at the beginning of the questionnaire explaining to the participants the nature of the survey; they were told that they could refuse to participate with no consequences. A contact person was provided in case any further information about the project was needed, or to ask for guidance in case any of the participants felt they needed assistance for themselves or for another colleague. The personal data of the participants has been kept anonymous at all times.
RESULTS
The survey was distributed to 2,868 anesthesiologist affiliated to S.C.A.R.E. and 403 completed the survey; this is an appropriate sample size according to the calculations done. No answers of the analysis were excluded.
Most of the participants (n = 210; 52,1 %) stated that their institutions did not have any policies to provide guidance to the staff with regards to suicide, mental illness or addiction. With regards to the Anesthesiology services or departments, the answers were quite similar; in a significant proportion (n = 311; 77,1 %) there is no guidance in situations such as suicide, addictions or mental illnesses, and when such guidance is available, it is primarily for mental illnesses (Table 1).
Table 1 Availability of policy guidelines for access to wellbeing services and experiences with a colleague's suicide.
| Questions | Answers of the Participants | Yes % (n) | No % (n) | Don't know % (n) |
|---|---|---|---|---|
| About Policy Guidelines | ||||
| Does you hospital have policy guidelines to assist the staff with the following? | Mental illness | 16.1 (65) | 55.8 (225) | 28.04 (113) |
| Suicide | 5.96 (24) | 63.2 (255) | 30.7 (124) | |
| Addiction | 5.71 (23) | 64.7 (261) | 29.5 (119) | |
| Does your anesthesiology service have any policies to provide guidance to the staff with regards to the following issues? | Mental Illness | 9.18 (37) | 79.6 (321) | 11.1 (45) |
| Suicide | 4.22 (17) | 82.3 (332) | 13.4 (54) | |
| Addiction | 4.47 (18) | 81.3 (328) | 14.1 (57) | |
| With regards to access to care and wellbeing services | ||||
| Is there someone in charge of employee wellbeing in your hospital? | 46.4 (187) | 25.5 (103) | 28 (113) | |
| Is anyone in charge of staff wellbeing in your anesthesiology service? | 14.8 (60) | 77.4 (312) | 7.6 (31) | |
| Would you know how to get assistance for yourself or a colleague in case someone becomes anxious or experiences suicidal ideation? | 20.1 (81) | 66 (266) | 13.9 (56) | |
| Experiences involving the suicide of a colleague | ||||
| Have you experienced the death of a colleague anesthesiologist or intensivist working in your same service who committed suicide, regardless of how long ago the incident happened? | 19.8 (80) | 73.9 (298) | 6.2 (25) | |
Source: Authors
Although the support provided in case of suicide, addiction and mental illness seems to be limited, 46 % of the participants said that their institution has someone in charge of personnel wellbeing. 14.8 % of the participants said they had a similar position in their anesthesiology service.
The participants were asked whether they knew how to access help in case they personally or a colleague experienced anxiety or suicidal ideation; however, only 20 % (n = 81) was aware of how to seek such assistance.
19%(n = 80) of the participants were aware of a suicide involving an anesthesiologist or intensivist; 6.2 % were not sure that the reason for such deaths was suicide. Among the 80 participants who were aware of a colleague who committed suicide, 65 (81,2 %) mentioned the death of at least one colleague and 4 (5 %) of up to three colleagues. 99 reports were identified, but it is impossible to determine whether there are any duplicate reports since no names were required or any other variable to identify the individual involved with each particular report.
Most of the reports correspond to male anesthesiologists or intensivists (n = 65; 65.6 %); the mean age was 40.5 years (SD: 8.37), but 4 of the 99 reports failed to indicate the age so these cases were excluded from the age groups. Six reports (6.32 %) correspond to anesthesiologists or intensivists less than 30 years old, 37 (38.9 %) were colleagues between 30 to 39 years old, 33 (34.7 %) were between 40 to 49 years, 18 (18.9) were between 50 to 59 years, and 1 (1.05 %) was a 60-year old colleague.
In terms of the date of the event, only 40 (40.4 %) of the reports included the approximate year of occurrence of the event. Considering these reports only, most of them occurred after 2017 (Figure 1). Likewise, the information about the place of occurrence is incomplete since it is only reported in 39 cases: 46.1 % (n = 18) of the events took place at home; 43.5 % (n = 17) at the workplace and in 10.6 % (n = 4) there is no information about the place of occurrence.
The information about the causal mechanisms is even more limited - it was only reported in 29 cases. The primary cause was opioid overdose (Table 2).
Table 2 Classification of the event according to the causal mechanism.
| Causal mechanism (n = 29) | n (%) |
|---|---|
| Poisoning | |
| Opioids | 17 (58.5) |
| Propofol | 2 (6.90) |
| Mix of anesthetic agents * | 2 (6.90) |
| Non-identified IV medication | 2 (6.90) |
| Other | |
| Firearm | 2 (6.0) |
| Jumping from height | 2 (6.0) |
| Unknown | 2 (6.0) |
*Propofol, fentanyl and rocuronium in one case, other not specified but if was a mix of agents. Source: Authors
Only 5.05 % (n = 5) of the colleagues reported were in leave of absence at the time of the event. With regards to this question, 4 reports fail to inform whether they were in leave of absence; in 7 cases there is no information about any leave of absence and in 83 cases (83.8 %) the colleague was not in leave of absence, 4 were suspended and one was in leave of absence because of general illness.
With regards to the information about whether the colleagues received any assistance after the event, only 4 (8.89 %) out of the 99 cases reported having received any assistance. The assistance included individual psychotherapy in 3 cases; group psychotherapy in 1 case and spiritual assistance in 1 case.
Further questions were asked about the factors that could have contributed to the occurrence of the event, but the predominant answer was a lack of knowledge about the actual situation, followed by mental health issues (Figure 2).
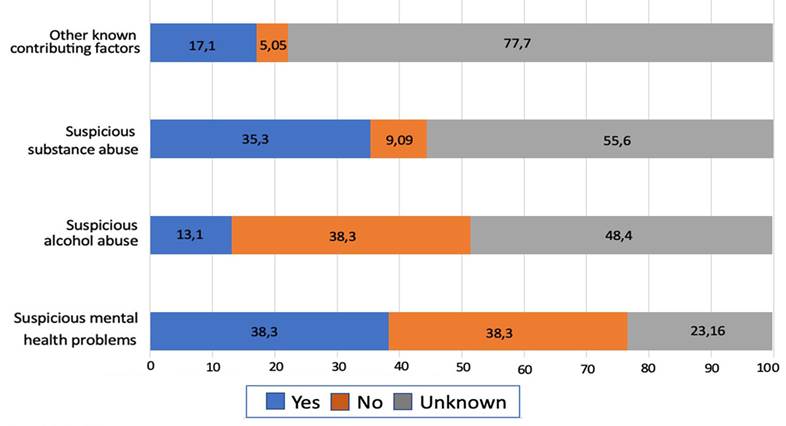
* The Unknown category has blank answers or marked as "Do not know". Source: Authors
Figura 2 Suspicious factors that may have contributed to the event (%)*
Finally, there was some enquiry about the suicide of other colleagues and friends who failed to meet the primary inclusion criteria; the participants informed about 70 additional cases (Figure 3). No additional information was required about these cases since they were beyond the scope of the survey.
DISCUSSION
Several Colombian anesthesiologists remember having experienced the suicide of a colleague. The topic is a tabu among the members of the anesthesiology services where these events have occurred, which reflects a combination of fear, powerlessness, failure to take action and a concerning lack of assistance for the individuals at risk.
Based on the answers given by these participants, some hospitals apparently offer guidance mostly in the area of mental health; however, it is a very small proportion.
This investigation suggests that there is limited availability of resources - or poor knowledge among the anesthesiologists - to assist in such relevant areas such as suicide, mental health or addictions in the anesthesiology services surveyed.
46 % of the respondents said that there is someone in charge of employee wellbeing in their hospital; however, the work conducted by these people responsible for wellbeing in hospitals is questionable since there is a mismatch between the activities conducted and the perception by the anesthesiologists with regards to the support provided and an effective assistance in times of crisis.
The results of the study with regards to the actual number of suicide cases are limited, since failure to collect the names or baseline characteristics of the cases, may result in duplication of reports from the respondents. This study fails to provide information about the actual incidence of suicide among the Colombian anesthesiologists.
Suicide reports among Colombian anesthesiologists over the last 28 years -since 1993 - were reviewed and there was evidence that 72 % of the suicides in our study occurred over the past 12 years. This is in contrast with the literature that reports a reduction in the number of suicides among anesthesiologists between 2014 and 2017. 10 This may be due to a recall bias of the respondents, or to a duplication of the same case by the participants. Whichever the reason, the assumption is that the support resources and wellbeing of the anesthesiologists have improved over the last few years, after the identification and description of the Burnout syndrome and its clear association with addictions and suicide.
In terms of gender, our study is consistent with the literature which shows that male anesthesiologists commit more suicides. (11 With regards to age, our study differs from the reports in the literature: the most frequently involved age group according to the literature is between 30 and 40 years old, while in our study the most frequently affected age group is between 25 and 29 years which corresponds mostly to residents or young specialists, which is second most affected age group according to worldwide reports.
The place where the suicide was committed is also important; in our study, 43.4 % of the anesthesiologists committed suicide at the workplace, which is consistent with the published data 12 that argue that physicians decide to commit suicide in places in which they have been emotionally involved or where an emotional wound has been inflicted in their lives.
The causal mechanisms of the deaths is consistent with the literature on suicide of anesthesiologists, which generally involve anesthetic agents 13 used in daily practice. Specifically, in suicides with propofol and/ or opiates - drugs used in the context of drug abuse or addiction - these events may have been due to accidental overdose, rather than an actual attempt to commit suicide. This is consistent with the fact that most of the cases described (83.8 %) were not in leave of absence, but were actively working with access to this type of drugs.
The study also shows that most of the respondents were not aware of the factors that contributed to the event; however, the primary factors reported included alcohol abuse, drug abuse, and mental health problems, which is consistent with the literature. 14
The UK Guidelines on Suicide among anesthesiologists 14 recommend the availability of a continuous education program on the stigmatization associated with mental illnesses and to provide assistance to colleagues who experience a situation of crisis in their financial, personal or professional life; additionally, support should be provided to peers following the suicide of a colleague. According to our study, this type of assistance was only indicated in 9% of the cases, whether as individual or group psychotherapy, and in the form of spiritual support in one case. This illustrates the lack of preparedness in our anesthesiology services and the prioritization of healthcare work over the human being. Time is a significant barrier to proper treatment; some studies reveal that many physicians fail to seek timely assistance because of the stigmatization or because of the potential professional consequences if they discuss the issue with their peers or superiors. 15
In the last section of the study we tried to measure the experiences of a non-anesthesiologist colleague, or even a relative, friend or acquaintance in the job and the results were alarming, with 70 additional cases identified. Over 800.000 people commit suicide among the general population per year worldwide 16, which represents one death every 40 seconds. One fourth of the world population experiences mental disorders at some point in their lives, and physicians and anesthesiologists are no exception. Anesthesiology is the medical specialty with the highest rates of suicide documented in the literature 17, in addition to the poor motivation of the physician to seek psychological or psychiatric help for fear of stigmatization.
A percentage of the respondents commented on the circumstances surrounding the suicide - this involves a feeling of guilt or the lack of emotional support by the institutional colleagues. Figure 4 illustrates some of the most relevant factors attesting to the painful nature of these situations.

Source: Authors
Figure 4 Cloud of words describing suicide by colleagues participating in the survey.
In conclusion, according to the information contributed by the respondents, most of the institutions in which they work do not have a policy to provide staff orientation with regards to suicide, mental illness or addiction. 19 % of the respondents said they were aware of the suicide of a colleague, representing a total of 99 cases. Due to the methodology used it is impossible to establish absence of duplication, but the results indicate that there is a problem with potential subsequent consequences.
The experiences described in the study emphasize the need to continue developing awareness by the institutions, the anesthesiologists themselves and the residents, of the need to design a support plan for colleagues in need because of occupational stress, drug dependence, depression, suicide, and other disorders that may be adequately treated if identified early.
Suicide is preventable when stigmatization, punishment and secrecy are removed from the equation. The anesthesia departments that have lost a colleague due to suicide must allow themselves to experience the pain, to discuss the issue, to mourn, to recover.
ETHICAL RESPONSIBILITIES
Endorsement by the ethics committee
This study was reviewed and approved by the Bioethics Committee of the School of Health Sciences of Universidad de Caldas, on June 11, 2020, under registry number CBCS-043.
Protection of persons and animals
The authors hereby declare that no experiments in humans or animals were conducted in this research. The authors state that the procedures followed were consistent with the ethical standards of the responsible human experimentation committee and pursuant to the World Medical Association and the Declaration of Helsinki.
ACKNOWLEDGEMENTS
Contributions by the authors
ACV, JCBR: Conception of the project, study planning, development of the research protocol, discussion of the results collected, drafting, review and approval of the final manuscript.
LMGB: Conception of the project, study planning, discussion of the results collected, drafting, review and approval of the final manuscript.
NFSB: Planning of the study, development of the research protocol, data collection, statistical analysis of the results, drafting, review and approval of the final manuscript.











 text in
text in 





