Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista de Salud Pública
Print version ISSN 0124-0064
Rev. salud pública vol.18 no.4 Bogotá July/Aug. 2016
https://doi.org/10.15446/rsap.v18n4.47517
http://dx.doi.org/10.15446/rsap.v18n4.47517
Epidemiological surveillance of herpes viral encephalitis in Cordoba, Colombia
Vigilancia epidemiológica de encefalitis por herpes virus en Córdoba, Colombia
Vaneza Tique1, Salim Mattar1, María Freire2, Eduardo Illian2, Francisco Camargo3, Oscar Vergara1 y Luiz T. Moraes-Figueiredo4
1 Universidad de Cordoba, Institute for Tropical Biological Research, School of Veterinary Medicine and Zootechnics. Monteria, Colombia. vtiquesalleg@yahoo.com; mattarsalim@hotmail.com; overgara@correo.unicordoba.edu.co
2 Neurovirosis Service. National Institute of Infectious Diseases, National Administration of Laboratories and Health Institutes "Dr. Carlos Malbran". Buenos Aires, Argentina. mcfreire@anlis.gov.ar; eillian@anlis.gov.ar
3 Institute for Advanced Medical Technology, Oncomédica. Monteria, Colombia. pcamassis@gmail.com
4 Virus Research Unit, School of Medicine of Ribeirão Preto, University of São Paulo, Brazil. ltmfigue@fmrp.usp.br
Received 8th March 2014 /Send for Modification 16th September 2015/Accepted 7th November 2015
ABSTRACT
Objective To establish an epidemiological surveillance of viral herpes encephalitis in major hospitals of Monteria, Cordoba.
Methods From September 2009 to December 2011, a descriptive study of cases of viral encephalitis was made in three hospitals in the city of Monteria. Cerebrospinal fluid (CSF) samples from 118 patients were included in the study. Clinical aspects, as well as cytochemical and microbiological analysis (Gram stain and culture) of CSF, were used for selecting the patients. Virus detection was performed by using multiplex nested PCR for Herpes simplex virus 1 and 2, Epstein Barr virus, Cytomegalovirus and Varicella zoster virus.
Results Viral DNA of herpesvirus was detected in the CSFs of 30 (25.4 %) participants, as follows: 22 (18.6 %) Herpes simplex 1 and 2 viruses, 4 (3.3 %) Cytomegalovirus and 1 (0.8 %) Varicella zoster virus. Co-infections were observed in 3 patients (2.5 %), 1 case by HSV-VZV and 2 cases by CMV/HSV. The clinical manifestations of the patients included: headache (18.6 %), fever (14.4 %), asthenia (10.1 %), seizures (9.3 %), vomiting (8.4 %), and stiff neck (5.9 %). Thirty percent of the patients also had HIV-AIDS. A case fatality rate of 20 % was observed for the patients.
Conclusions This paper shows that herpesvirus is a cause of infection of the CNS in patients from Cordoba. This study contributes to the epidemiology of encephalitis, as well as to patient management.
Key Words: Herpesviridae, simplexvirus, cerebrospinal fluid, HIV (source: MeSH, NLM).
RESUMEN
Objetivo Establecer una vigilancia epidemiológica de la encefalitis viral herpética en los principales hospitales de Montería, Córdoba.
Materiales y Métodos Se realizó un estudio descriptivo de los casos de encefalitis viral entre septiembre de 2009 diciembre de 2011 en tres hospitales en la ciudad de Montería. Las muestras líquido cefalorraquídeo (LCR) de 118 pacientes fueron incluidos en el estudio. Los aspectos clínicos como el análisis citoquímico y microbiológico (tinción de Gram y cultivo) de LCR fueron utilizados para la selección de los pacientes. La detección de virus se realizó por PCR anidada multiplex para Herpes simplex virus 1 y 2, virus de Epstein Barr, virus zoster de la varicela y el citomegalovirus.
Resultados Se detectó ADN viral del virus del herpes en 30 (25,4 %) muestras de LCR en los pacientes de la siguiente manera: 22 (18,6 %) Herpes simplex virus 1 y 2, 4 (3,3 %) Citomegalovirus y 1 (0,8 %) del virus de la varicela zóster. Se observaron Co-infecciones en 3 pacientes (2,5 %), 1 caso por el VHS-VZV y 2 casos por CMV / HSV. Las manifestaciones clínicas de los pacientes fueron: cefalea (18,6 %), fiebre (14,4 %), astenia (10,1 %), convulsiones (9,3 %), vómitos (8,4 %), y rigidez de nuca (5,9 %). El treinta por ciento de los pacientes también tenía VIH-SIDA. Se observó una tasa de letalidad del 20 % de los pacientes.
Conclusiones Se demuestra que el herpesvirus es causa de infección del SNC en pacientes en Córdoba. Este estudio contribuye a la caracterización serológica viral epidemiológica de la encefalitis viral, así como en el manejo del paciente ya que se describen hallazgos clínicos importante en la población adulta estudiada.
Palabras Clave: Herpesviridae, simplexvirus, liquido cefalorraquideo, VIH (source: DeCS, BIREME).
Viral infections are a major cause of infection in the central nervous system (CNS) worldwide, surpassing the frequency of bacterial, fungal and protozoan agents (1). Enteroviruses, herpesviruses and some arboviruses have been recognized as common etiologic agents of meningitis and encephalitis. It is estimated that 39 % of infections caused by these viruses produce severe neurological symptoms (1).
Reports on the incidence of viral encephalitis vary depending on the study population, differences in case definition and diagnostic methods. However, the incidence of viral encephalitis in Europe is 0.7-13.8 per 100 000 (0.7-12.6 per 100 000 for adults and 10.5-13.8 per 100 000 for children.) Encephalitis by herpes simplex virus (HSV) has an annual incidence of 1 in 250 000 to 500 000 cases in industrialized nations (2-4).
HSV-1 is the most common cause of encephalitis, representing 5 to 35 % of cases, while enteroviruses are a leading cause of meningitis in 85 % of cases (1,3). An increasing number of cases of meningoencephalitis related to herpesviruses has been reported in Latin America. In Brazil, herpesviruses, enteroviruses and dengue viruses that produce meningoencephalitis have been reported in the cities of Ribeirao Preto and Rio de Janeiro (1,5). In Argentina, outbreaks of meningitis by enterovirus and cases of encephalitis by adenovirus have both been reported (4,6,7). In Chile, clinical manifestations of CNS infections by HSV-1 and 2 have been studied (8).
In Colombia, the frequency of herpetic infections in school-age children from the Department of Antioquia was determined by establishing a seroprevalence of 78 % for HSV-1, 44.5 % for VZV, 98 % for CMV, 94 % for EBV, 100 % for HHV6 and 0 % for HSV-2 (9). The circulation of enteroviruses, which caused 263 cases of aseptic meningitis, was also reported in 2004 (10). Considering that little is known in Colombia about viruses producing meningitis and/or encephalitis, a surveillance study on herpesviruses causing these diseases in the city of Monteria, Department of Cordoba, Colombia, has been conducted.
MATERIALS AND METHODS
This longitudinal descriptive study on meningoencephalitis cases was performed from 2009 to 2011 in three hospitals of Monteria City. The study was approved by the ethics committee of the Institute for Tropical Biological Research (Resolution 01-2009), taking into account the procedures, management and conservation of samples, and the technical-administrative procedures for health research included in the resolution N°8430 of the Ministry of Health of Colombia, in 1993 (11).
Patients and CSF samples
Clinical and epidemiological data of adult patients (over 19 years of age), obtained from hospital medical records were used for participant selection. Patients with fever, headache, seizures and signs of brain damage, such as altered consciousness and/or personality and/or focal neurological signs, were included in the study. Most of the participant patients had an increased cell count and/or an increased protein level in CSF (1,3,12). Patients with microorganisms detected by direct examination (bacteria and/or fungi), KOH, China ink, Gram stain, Ziehl Neelsen and culture of CSF were excluded from the study.
CSF samples were collected through lumbar puncture, accessing the subarachnoid space. Lumbar punctures followed biosafety standards and CSFs were collected in two sterile screw cap tubes, for chemical and bacteriologic studies (13). The samples were stored at -20°C until they were delivered to the Institute for Tropical Biological Research at University of Cordoba, under strict biosafety conditions.
DNA extraction and multiplex nested PCR
DNA extraction of CSF was performed in a class II biological safety cabinet with the DNA mini kit (Qiagen, USA) following the manufacturer's instructions and stored at -90° C until processing.
The M-Nested PCR for herpesvirus was performed based on the procedure of Cassas et al. (14), with some modifications. The PCR reaction mixture, containing a final volume of 50 µl, was added: 20 mM Tris-HCl (pH 8.4), 50 mM KCl, 4 mM MgCl2, 0.2 mM dNTP mix, 10 pmol of each sense and antisense herpesvirus primers (VZV, HSV1-2, CMV and EBV), five units of Taq DNA Polymerase (Invitrogen) and 5 µl of the DNA sample. Positive controls, negative controls and clinical samples were tested. PCR mixtures were subjected to a first cycle at 94°C for 2 min, followed by 35 cycles of 1 min at 94°C, 1 min at 55°C and 1 min at 72°C. After the last cycle, samples were incubated for 4 min at 72°C to allow complete extension of amplicons.
The amplification mixture for nested-PCR contained 5 µl of the PCR reaction mixture and the same reagents, but including 10 pmol of each herpesvirus sense and antisense internal primers (VZV, HSV1-2, CMV and EBV). Nested-PCR mixtures were subjected to the same thermal cycles used for PCR.
Upon completion of the nested amplification, 15 µl of the reaction mixture were analyzed through electrophoresis in a 3.0 % agarose gel. After electrophoresis, the gel was stained with ethidium bromide and the size of the amplicons was determined by comparison against DNA size markers of 100, 50 and 25 bp (Promega, USA). Each test included a negative control (ultrapure water DNAse and RNAse free).
Commercial positive controls including OptiQual AcroMetrix Brand High Positive Control for CMV (Strain AD169 Ref. 951702), EBV (propagated in peripheral blood mononuclear cells; Ref 951307), HSV-1 (Ref. 951301), HSV-2 (HSV-1 and 2 were propagated in tissue culture, Ref 951302) and VZV DNA extracted from lesions of a patient with chickenpox were used.
Sequencing PCR products
For nucleotide sequencing, amplicons of positive samples of EBV, CMV and VZV were obtained using a PCR described by Mendoza et al. (5). For HSV-1 and-2, amplicons obtained by the method of Casas et al.(14) were used directly. The amplicons were purified with PureLink ™ quick Gel extraction kit (Cat K2100-12) and sequenced in ABI 3730 XL automated sequencers by Macrogen (Korea). Nucleotide sequences were edited and aligned with MEGA program version 5.22 (15) and compared with those of viruses available in GenBank (16).
Statistical analysis
Statistical System Analysys SAS® version 9.1 was used for descriptive statistics, chi-square tests for gender variables, Fisher exact test for age variables and confidence intervals of 95 % to establish virus frequencies. A p value of <0.05 was considered statistically significant.
RESULTS
The multiplex nested PCR for herpesviruses was performed successfully as shown in Figure 1. The genome of a herpesvirus was detected in 30 (25.4 %) of the 118 CSF samples as follows: 22 (18.6 %) Herpes simplex 1 and 2, 4 (3.3 %) Cytomegalovirus, 1 (0.8 %) Varicella zoster virus; Esptein Barr virus was not detected. Co-infection was observed in three patients (2.5 %): CMV/VHS (2 cases) and VZV/HSV (1 case). The confidence interval (CI) of 95 % for HSV was 13.7 -28.6 for Cytomegalovirus 1.0 – 9.1 and for varicella zoster virus 0.6-4.0.
9.3 % (11/30) of the patients with herpesvirus in CSF were females and 16.1 % (19/30), males. There was no statistical significance between gender and positivity (p>0.05). 30 % of the patients had HIV-AIDS.
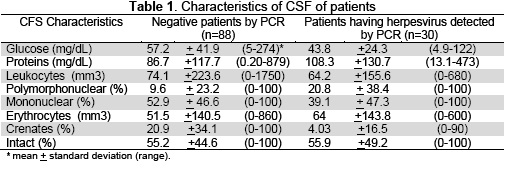
Clinical manifestations observed among the patients with herpesvirus in CSF included: headache (18.6 %), fever (14.4 %), decrease in muscle strength (10.1 %), seizures (9.3 %), vomiting (8.4 %), stiff neck (5.9 %), mental confusion and hypoesthesia (2.5 %), dysarthia (1.6 %) and irritability (0.8 %). CSF of the patients presented pleocytosis >5 cells/mm3 (average value 64.2/mm3) in 50 % of the cases, with predominance of mononuclear cells in 30 % (mean 39.1 %) and of polymorphonuclear cells in 20 %. Erythrocytes were also found in CSFs of 50 % of the cases (average value 64 mm3) and increased protein levels in 70 % (>30 mg/dL) (mean 108,3), as shown in Table 1.
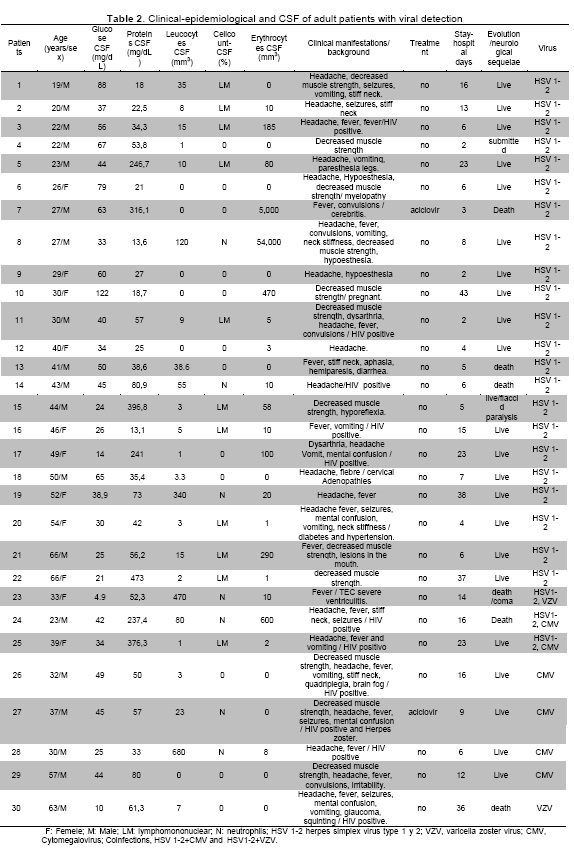
The patients with herpesvirus in CSF remained hospitalized for 13.5 ± 11.7 days (range: 2-43). 60 % of the patients received antibiotic treatment, 20 % received corticosteroids and only 6 % received antiviral drugs. The case fatality rate was 20 % (Table 2).
DISCUSSION
The results obtained in this study are similar to those reported in Brazil, where herpesviruses were identified as causative agents of meningitis or encephalitis in adults (n=17); 176 % HSV1, HSV1 and 2, CMV and enterovirus each in one patient; the most common agent was dengue virus in 47 % of cases (1).
In Brazil (5), 200 patients with CNS infections were analyzed. Herpesvirus DNA was detected in 12 % of CSF, distributed as follows: 6 % CMV; 5 % HSV-1; 05 % EBV and VZV one each; 113 % enterovirus; two coinfections of enterovirus/CMV and one of HSV1/CMV. Alphavirus and flavivirus were absent. Similar data were obtained in this study, although, enterovirus, alphavirus or flavivirus were not sought.
A study conducted in Taiwan, with different molecular techniques, detected simultaneously 29 pathogens, including 21 viruses, 5 bacteria, 2 fungi, and 1 parasite. Herpesviruses were identified in 23 out of 131 cases of encephalitis and meningitis: HSV1 (n=2), HSV2 (n=1), VZV (n=3), EBV (n=16) and CMV (n=1); in adult patients with encephalitis, 6 HSV-1 (n=2), VZV (n=3) and CMV (n=3) were identified (17). Despite the use of more sensitive techniques, viral encephalitis results were similar to those shown here.
In a report made in Rome, the genome of herpesvirus was detected using a highly sensitive real-time PCR technique in 335 % (52/155) of patients with acute meningitis, meningoencephalitis and other neurological disorders. VZV (309 %) was detected followed by HSV-1 (279 %), EBV (139 %), HSV-2 (93 %), HHV-6 (93 %) and coinfection (HSV-1/VVZ, HSV-1/HSV-2, EBV/HSV-2). The Italian results are similar to those of this study, where co-infections were observed by HSV1-2/VVZ and HSV1-2/CMV and positivity was 254 % (30/118) (18).
In recent years, VZV has been increasingly identified as a cause of meningitis and meningoencephalitis or un-associated rash illness (19). VZV, with a frequency ranging from 5 to 29%, is considered the third most common causative agent of viral meningitis after enterovirus and HSV-2. In this study two (17%) cases of VZV were detected, which is similar to the results reported by Lozano et al.(20), who found 11 out of 519 (21 %) VZV-positive adult patients.
In Israel (21) several cases of meningoencephalitis caused by VZV (n=20), HSV-1 (n=13) and HSV-2 (n=4) were compared, and it was found that cases of VZV and herpes zoster had similar clinical manifestations, with the exception of focal neurologic findings and seizures that occurred only in the group in which VHS was identified. It has been reported that up to 42 % of cases of infection by VZV have no herpes zoster dermatological manifestations. In this study, the two cases of VZV did not present herpes zoster and both were fatal cases with underlying diseases (either HIV, TEC-severe and ventriculitis or coinfection with HSV1-2).
In Chile (8), a series of 15 cases of herpes encephalitis described the main clinical features of the disease. The average age was 41, similar to the average age of in adults studied here (range 19-66). Fica et al. stated that the main clinical manifestations were fever, headache and impairment of consciousness and, less frequently, focalizations or seizures. Other symptoms included vomiting, aphasia, hallucinations, abdominal pain or silence. In this study, the main clinical manifestations were fever, headache, seizures, vomiting, decreased muscle strength and stiff neck. Moreover, the Chilean study used acyclovir in all patients; in contrast, for this study, acyclovir was used in only 6 % of patients (8).
A case report of HSV-2 encephalitis in an immunocompetent patient conducted by (22) in the UK, showed the importance of this agent in severe cases of encephalitis in adults, which are often underestimated by the mild classic appearance of HSV2 compared to HSV1. Regarding the cases of herpetic encephalitis in adults in this study, it was not possible to differentiate the subtype of herpes simplex virus since fatal cases were 20 % and only two patients were treated with acyclovir.
In the UK (23), viral agents in 12 % of 787 CSF samples, including enterovirus, HHV-6, EBV, HSV-1, CMV, JCV and coinfection (VHS-1/VEB, VHS2/enterovirus, VEB/VHH-6, EBV/CMV) were detected. A normal CSF WCC was found in 53 % PCR positive CSF samples, and 34 % of CSF samples had both normal WCC and protein levels when CSF white cell count was abnormal, although a normal CSF did not exclude a viral infection. In this study 491 % of leukocyte counts and 192 % of protein levels were normal.
This study found that the main viruses detected in the immunosuppressed population (20 %) were HSV1-2 (7/11), CMV (6/11), VZV (1/11) and coinfection with HSV1-2/CMV (2/11) (24). In India, multiplex PCR was used to establish the frequency of 10 opportunistic virus DNA in CSF samples and brain tissue of HIV-infected patients. Virus DNA was detected in the CSF of 45/55 cases as follows: 62 % JCV, 44 % EBV, 25 % CMV, 36 % VZV, 18 % HSV-1 and 18 % HHV6. A single virus was detectable in 20 cases, 19 cases were coinfected with two viruses, and 6 cases were positive for the three viruses. JCV in CSF was detectable 62 % of cases and 42 % of brain tissue. These differences could be explained by the inclusion of patients with other CNS infections of bacterial, parasitic and/or fungal origin, the large number of needs studied and the technique used.
The high percentage of encephalitis of unknown origin, 745 % (88/118), reported in this study is consistent with other research; some countries have reported 37 %, 65 % and up to 70 %, in which the etiology was not determined (22, 23). Despite this finding, the amount of cases with unknown cause was higher than that for any specific identified cause. Explanations include the failure to identify non-encephalitic syndromic mimics, inadequate case investigation and the presence of novel infectious or non-infectious encephalitis causes. The false negative result of RT-PCR for HSV in a patient with herpes encephalitis can be caused by a sample taken in an early stage if the evolution of the disease, the presence of inhibitors of PCR or improper handling or storage sample (25-27). For example, in this study, agents such as enteroviruses and arboviruses were not studied.
In Argentina, enteroviruses have been associated with 3 % of cases of acute encephalitis, similar to the 2 % frequency reported in other countries 2 % (6). Adenovirus encephalitis often occurs as a complication of severe respiratory disease; (7) described the role of adenovirus in neurological infections, particularly encephalitis, with and incidence of 76 % and possible multiple infection with herpesvirus and polyomavirus, as usual in immunosuppressed patients. However, these agents were not investigated in this study and should be considered along with the arboviruses that are associated with these neurological diseases in other countries.
This study had some limitations; one of them was t-he non-inclusion of other viral agents such as enterovirus, adenovirus and arbovirus that are known to be responsible for similar neurological symptoms. Additionally, herpes simplex virus was not subtyped.
In conclusion, this was the first epidemiological surveillance of herpes encephalitis in Cordoba. The findings contribute to understand the epidemiology of encephalitis and the clinical management of patients. Furthermore, this study described the main clinical manifestations of the disease, its evolution, and the use of antiviral agents in the adult population ♣
Acknowledgments: To the Institute for Tropical Biological Research and the research center of Universidad de Cordoba (Project FMV 0311) for their support and funding.
Conflicts of interest: None.
REFERENCES
1. Soares CN, Cabral-Castro MJ, Peralta JM, de Freitas MRG, Zalis M, Puccioni-Sohler M. Review of the etiologies of viral meningitis and encephalitis in a dengue endemic region. J Neurol Sci. 2011 4/15;303(1-2):75-79. [ Links ]
2. Mendoza LP, Bronzoni RVdM, Takayanagui OM, Aquino VH, Moraes Figueiredo LT. Viral infections of the central nervous system in Brazil. J Infect. 2007 6;54(6):589-596. [ Links ]
3. Solomon T, Michael BD, Smith PE, Sanderson F, Davies NWS, Hart IJ, et al. Management of suspected viral encephalitis in adults-Association of British Neurologists and British Infection Association National Guidelines. J Infect. 2012 4;64(4):347-373. [ Links ]
4. Freire MC, Cisterna DM, Rivero K, Palacios GF, Casas I, Tenorio A, et al. Analysis of an outbreak of viral meningitis in the province of Tucuman, Argentina. Rev Panam Salud Publica. 2003 Apr;13(4):246-251. [ Links ]
5. Mendoza LP, Bronzoni RVdM, Takayanagui OM, Aquino VH, Moraes Figueiredo LT. Viral infections of the central nervous system in Brazil. J Infect. 2007 6;54(6):589-596. [ Links ]
6. Cisterna DM, Palacios G, Rivero K, Girard D, Lema C, Freire MC. Epidemiology of enterovirus associated with neurologic diseases. Medicina (B Aires). 2007;67(2):113-119. [ Links ]
7. Lema CL, Cisterna DM, Freire MC. Neurologic disease due to adenovirus infection. Medicina (B Aires). 2005;65(3):196-200. [ Links ]
8. Fica A, Perez C, Reyes P, Gallardo S, Calvo X, Salinas AM. Herpetic encephalitis: case series of 15 patients confirmed by polymerase chain reaction. Rev Chilena Infectol. 2005 Mar;22(1):38-46. [ Links ]
9. Ossa J, Arango A, Patton J, Stewart J. Frecuencia de infección por herpesvirus en 129 niños en edad escolar en Antioquia. IATREIA. 1990 Marzo;3(1):25-29. [ Links ]
10. Aguirre C, Vallejo I, Vargas A, Acevedo L, Uribe G, Londoño A. Epidemia de meningitis viral en Medellín, Colombia, 2004. Revista de Salud Pública. Medellín 2006;1:67-82. [ Links ]
11. República de Colombia, Ministerio de Salud. Resolucion N° 008430 de 1993. Republica de Colombia, Ministerio de Salud Resolucion Nº 008430 DE 1993 (4 de octubre de 1993).Por la cual se establecen las normas científicas, técnicas y administrativas para la investigación en salud. 1993; Available at: http://www.dib.unal.edu.co/promocion/etica_res_8430_1993.pdf. Accessed 09/02, 2012. [ Links ]
12. Kneen R, Michael BD, Menson E, Mehta B, Easton A, Hemingway C, et al. Management of suspected viral encephalitis in children - Association of British Neurologists and British Paediatric Allergy, Immunology and Infection Group National Guidelines. J Infect. 2012 5;64(5):449-477. [ Links ]
13. Wright BL, Lai JT, Sinclair AJ. Cerebrospinal fluid and lumbar puncture: a practical review. J Neurol. 2012 Aug;259(8):1530-1545. [ Links ]
14. Casas I, Tenorio A, Echevarria JM, Klapper PE, Cleator GM. Detection of enteroviral RNA and specific DNA of herpesviruses by multiplex genome amplification. J Virol Methods. 1997 6;66(1):39-50. [ Links ]
15. Tamura K, Peterson D, Peterson N, Stecher G, Nei M, Kumar S. MEGA5: Molecular Evolutionary Genetics Analysis using Maximum Likelihood, Evolutionary Distance, and Maximum Parsimony Methods. 2011; 28(Molecular Biology and Evolution):2731-2739. [ Links ]
16. Basic Local Alignment Search Tool (BLAST) NCBI. Basic local alignment search tool (BLAST) NCBI. 2013; Available at: http://blast.ncbi.nlm.nih.gov/Blast.cgi. Accessed 10/15, 2013. [ Links ]
17. Hsu CC, Tokarz R, Briese T, Tsai HC, Quan PL, Lipkin WI. Use of staged molecular analysis to determine causes of unexplained central nervous system infections. Emerg Infect Dis. 2013 Sep;19(9):1470-1477. [ Links ]
18. Gaeta A, Verzaro S, Cristina LM, Mancini C, Nazzari C. Diagnosis of neurological herpesvirus infections: real time PCR in cerebral spinal fluid analysis. New Microbiol. 2009 Oct;32(4):333-340. [ Links ]
19. Florén-Zabala L, Chamizo-López FJ, Eisman-Maraver A, Pérez-González C, de Ory-Marchón F, Trallero-Maso G, et al. Meningitis aséptica en la población adulta. Etiología y utilidad de las técnicas moleculares en el manejo clínico del paciente. Enfermedades Infecciosas y Microbiología Clínica. 2012;30(7):361-366. [ Links ]
20. Becerra JC, Sieber R, Martinetti G, Costa ST, Meylan P, Bernasconi E. Infection of the central nervous system caused by varicella zoster virus reactivation: a retrospective case series study. Int J Infect Dis. 2013 Jul;17(7):e529-34. [ Links ]
21. Pollak L, Dovrat S, Book M, Mendelson E, Weinberger M. Varicella zoster vs. herpes simplex meningoencephalitis in the PCR era. A single center study. J Neurol Sci. 2012 Mar 15;314(1-2):29-36. [ Links ]
22. Barker KR, Sarafino-Wani R, Khanom A, Griffiths PD, Jacobs MG, Webster DP. Encephalitis in an immunocompetent man. J Clin Virol. 2014 Jan;59(1):1-3. [ Links ]
23. Davies NW, Brown LJ, Gonde J, Irish D, Robinson RO, Swan AV, et al. Factors influencing PCR detection of viruses in cerebrospinal fluid of patients with suspected CNS infections. J Neurol Neurosurg Psychiatry. 2005 Jan;76(1):82-87. [ Links ]
24. Kannangai R, Sachithanandham J, Mahadevan A, Abraham AM, Sridharan G, Desai A, et al. Association of neurotropic viruses in HIV-infected individuals who died of secondary complications of tuberculosis, cryptococcosis, or toxoplasmosis in South India. J Clin Microbiol. 2013 Mar;51(3):1022-1025. [ Links ]
25. Child N, Croxson MC, Rahnama F, Anderson NE. A retrospective review of acute encephalitis in adults in Auckland over a five-year period (2005-2009). Journal of Clinical Neuroscience. 2012 11;19(11):1483-1485. [ Links ]
26. Granerod J, Ambrose HE, Davies NW, Clewley JP, Walsh AL, Morgan D, et al. Causes of encephalitis and differences in their clinical presentations in England: a multicentre, population-based prospective study. Lancet Infect Dis. 2010 Dec;10(12):835-844. [ Links ]
27. Izquierdo G, Cofre J, Torres JP, Venegas G, Vergara A, Farfan M. Neonatal herpes simplex encephalitis: clinical profile versus molecular biology. Rev Chilena Infectol. 2012 Aug;29(4):464-467. [ Links ]