INTRODUCTION
Fever of unknown origin (FUO) is a fever >38.3°C that lasts for more than one week, whose cause cannot be established despite thorough investigations in the hospital. 1 There are over 200 causes of FUO, including infections, connective tissue diseases, and neoplasms. 2
Generally, pheochromocytoma is a benign neoplasm derived from chromaffin cells of the adrenal medulla, with an estimated annual incidence of 0.5-0.8 cases per 100 000 people. 3 This type of tumor is characterized by the production of large amounts of catecholamines and also by the capacity to secrete bioactive peptides such as cytokines, mainly interleukin-1 IL-1, interleukin-6 IL-6, and TNF alpha.
IL-6 is an endogenous pyrogen that has the capacity to activate the hypothalamic-pituitary-adrenal axis at each of its central levels 4-7 and to stimulate the secretion of glucocorticoids directly in the adrenal cortex. This cytokine, together with IL-1, is the major inducer of hepatic acute phase protein synthesis. 8
The following is the case of a patient with FUO, increased inflammatory markers, hyper-cortisolism secondary to excess production of adrenocorticotropic hormone (ACTH) and an adrenal mass with histologic features of pheochromocytoma, in whom all symptoms normalized after tumor removal.
CASE PRESENTATION
A 24-year-old male patient from Bogotá (Colombia), an industrial engineer, attended the emergency room of a private tertiary referral hospital for fever, most often >39°C, for 10 days, accompanied by myalgia from the first day and choluria in the last 3 days. Although the feverish peaks had decreased with treatment with non-steroidal anti-inflammatory drugs (NSAIDs) and acetaminophen, adequate control of this clinical sign had not been achieved.
The subject reported that two days before the onset of the fever, he visited a rural area with a warm climate (Melgar, Tolima). He had a history of smoking for 10 years until the year before the consultation, bicuspid aortic valve without hemodynamic consequences and appendectomy during childhood. With the exception of fever, his physical examination was normal; however, laboratory results showed marked elevation of leukocyte count (18 000 U/microliter, normal value 4 000-10 000) and platelet count (920 000 U/microliter, normal value up to 350 000), as well as increased liver transaminases (>500 U/L, normal value up to 32) and C-reactive protein (5.5 mg/dL, normal value 0.0-0.8). According to serum creatinine and blood urea nitrogen values, kidney function was preserved.
In search of an infectious process, blood, stool and urine cultures for common germs and serology studies for dengue, leptospirosis, Epstein-Barr virus and cytomegalovirus were performed, which yielded negative results; therefore, infectious causes were ruled out. Subsequently, given the normal results of tests for antinuclear antibodies, antibodies to extractable nucleus antigens, and C3 and C4 complements, autoimmune causes were ruled out. Chest x-ray was normal and the echocardiogram reported no vegetations. A lumbar puncture was performed, after verification of a normal brain CT scan, which also had a normal result. However, an abdominal ultrasound showed a left adrenal mass that was described as a heterogeneous mass of 7x5cm, hypointense in T1, hyperintense in T2, with areas of necrosis and diffusion restriction, in an MRI of the abdomen with contrast agent (Figure 1).

Source: Document obtained during the study.
Figure 1 MRI of the abdomen (axial plane). The arrow points to the left adrenal mass of 7cm in diameter.
At first, the fever was considered to be an incidentaloma but, since the fever persisted, tumor fever was suspected. To rule out the presence of extra adrenal lesions, a fluorine-18-fluoro-deoxyglucose positron emission tomography (FDG-PET) was performed, in which only the left adrenal mass with increased tracer uptake was evident (Figure 2). Moreover, the patient underwent high-performance liquid chroma-tography, which showed that 24-hour urinary metanephrine levels were elevated (7.8 ug/24 hours, normal value <1.0). Morning ACTH and cortisol levels were 19 pg/mL (normal value 5-65 pg/mL) and 27 ug/dL (normal value 5-18 ug/dl), respectively; the latter was not suppressed in the overnight suppression test with 1mg dexamethasone (22 ug/dL, normal value <1.8U g/dL).

Source: Document obtained during the study.
Figure 2 Fluorine-18-fluorodeoxyglucose positron emission tomography (coronal planes). The arrows indicate left adrenal mass with increased tracer uptake.
Based on the findings, ACTH-producing pheochromocytoma was suspected, so the patient, after preoperative preparation with alpha-adrenergic blocking agents and intravascular repletion with isotonic fluids, was taken to surgery for open resection of the mass. During the procedure, the subject presented transient hypotension that was reverted with intravenous fluids. In the postoperative period, he did not require prolonged replacement glucocorticoid since baseline serum cortisol remained in normal ranges; he also had a rapid reversion of the alterations and did not have more ever episodes. The pathology report confirmed pheochromocytoma with low Ki-67 proliferation index (1%), and immunohistochemistry was negative for ACTH and positive for chromogranin A and protein S100 in sustainable cells.
At the time of writing this case report, the patient had an adequate clinical progress, with no biochemical relapses and normal values of fractionated plasma metanephrine and urinary and plasma cortisol. The follow-up MRI of the abdomen did not show any structural relapse either.
Given the age of the patient and the increased PET-FDG uptake of the adrenal mass, it is likely that the pheochromocytoma found was associated with a mutation in the succinate dehydrogenase enzyme. However, this diagnosis was not confirmed because genetic testing could not be performed.
DISCUSSION
Pheochromocytomas are tumors derived from chromaffin cells of the adrenal medulla, characterized by increased and uncontrolled secretion of catecholamines, 9 which can also produce other biologically active peptides such as IL-6.
This cytokine is a glycoprotein known primarily for its role in innate immune response due to its pyrogenic and acute-phase protein inducing capacity. 10
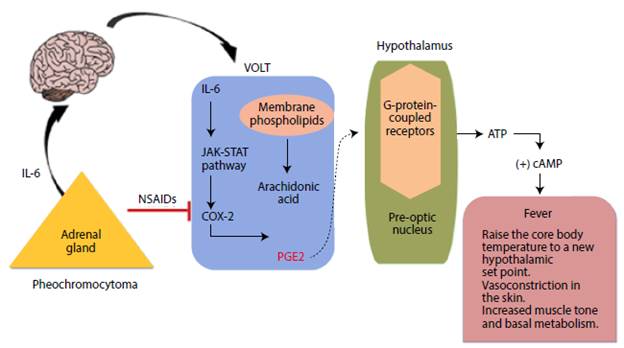
In the central nervous system, IL-6 raises body temperature by stimulating the vascular organ of the lamina terminalis after binding to its IL-6R receptor, thus inducing the transcription of the cyclooxygenase-2 protein, a key enzyme for the production of prostaglandin E2 (PGE2). 11 The latter, through its EP3 receptor, is involved in the activation of various somatic and sympathetic thermogenic mechanisms responsible for fever in the preoptic nucleus neurons, 12 as described in Figure 3.
Source: Own elaboration.
Figure 3 Mechanism of interleukin-6 fever production. NSAIDs: non-steroidal anti-inflammatory drugs; VOLT: vascular organ of lamina terminalis; ATP: adenosine triphosphate; IL-6: interleukin-6; PGE2: prostaglandin E2; COX-2: cyclooxygenase 2; cAMP: cyclic adenosine monophosphate; JAK: Janus kinase; STAT: Signal transducer and activator of transcription proteins.
IL-6 also stimulates the release of ACTH from the anterior pituitary gland; this hormone, in turn, promotes cortisol synthesis in the adrenal cortex. 13,14 The classic signaling of this cytokine starts with the binding to its membrane receptor (IL-6R), which leads to the activation of the intracellular signaling pathway of the Janus kinases. Subsequently, signal transduction-activated transcription factors translocate into the nucleus and gene expression is induced, as in the case of proopiomelanocortin (POMC), 15,16 which then generates ACTH by cleavage. In this way, it is possible to explain ACTH-dependent hypercortisolism, which was one of the biochemical alterations presented by the reported patient. It should be noted that, given the short time of evolution and the direct effect of IL-6 on corticotrophs, no suppression of the adrenal axis is expected when removing the IL-6 producing tumor, as in the reported case.
IL-6 hypersecretion also explains the changes in the leukocyte and platelet count, since it stimulates the differentiation of B and T lymphocytes (which causes leukocytosis) and intervenes in the proliferation and maturation of the megakaryocyte cell lines, generating thrombocytosis. In addition, it has proapoptotic effects on hepatocytes that generate hyper-transaminasemia. 17,18
In the case presented herein, the feverish peaks decreased after using NSAIDs, which act by blocking the production of PGE2. 19,20 However, complete remission of fever was only possible after surgery, which also allowed normalizing inflammatory markers (leukocytosis, thrombocytosis, hypoalbuminemia and hyper-transaminasemia). This supports the role of IL-6 as responsible for the unusual manifestations observed in this case.
Although plasma levels could not be determined, the reversal of all inflammatory alterations after tumor removal and the review of similar clinical cases reported in the literature 21-28 allow us to infer that the secretion of IL-6 by a pheochromocytoma should be considered as an explanation of the fever and the marked inflammatory response (thrombocytosis, transaminasemia, and ACTH-dependent hypercortisolism).
CONCLUSION
FUO is a condition with multiple causes, including tumors, which must be considered in the etiological diagnosis process. The presence of an IL-6 producing pheochromocytoma is a rather rare cause of FUO (less than 10 cases reported in the medical literature), so the description and publication of this report will allow clinicians to increase diagnostic suspicion and thus improve therapeutic interventions.














