INTRODUCTION
Cystic hygroma (CH), also known as nuchal edema, is a type of lymphangioma characterized by the presence of benign cysts that form due to congenital malformations of the lymphatic system. Its incidence is estimated at approximately 1 case per 6 000 live births and 1 case per 750 miscarriages 1,2.
The most frequent initial ultrasound manifestation in cases of CH is thickening of the nuchal fold in the first trimester. Its diagnosis is based on the visualization of a bilateral cystic lesion (septated or nonseptated) in the occipitocervical region, this being its main location (75% of cases), followed by the axillary region (20%), the retroperitoneum (2%), the extremities (2%), and the mediastinum (1%) 3,4.
Half of CH cases are associated with chromosomal abnormalities, and approximately 60% of euploid fetuses with this condition have structural abnormalities, including malformations of the heart, abdominal wall, central nervous system, genitourinary system, among others 3,5. The intrauterine mortality rate associated with CH is up to 54.8% of cases and only about 10% of surviving fetuses have no major morbidity 6.
Once the diagnosis of CH has been made using screening ultrasound during the first trimester, invasive genetic study is recommended to rule out chromosomal abnormalities, as well as an anatomy ultrasound to rule out associated malformations, ultrasound follow-up of the size of the lesion, and multidisciplinary counseling to establish the prognosis and management of the patient's prenatal and postnatal period 4,7.
The aim of this article is to establish the perinatal prognosis of two cases of euploid fetuses diagnosed with CH and to analyze their evolution.
CASE PRESENTATION
Case 1
A 19-year-old woman from Bogotá (Colombia), a housewife of medium-low socioeconomic status, with a history of focal epilepsy treated with carbamazepine 800 mg/ day and an obstetric history of complete abortion in the first trimester, attended the Hospital Militar Central of Bogotá, Colombia, in November 2019, when she was 15 weeks pregnant (obstetric formula G2A1V0), for a routine obstetric ultrasound, in which an 18x15x6mm anechoic image of the neck of the fetus and irregular contours, containing a nuchal ligament but no septa or color Doppler uptake, was observed (Figure 1). Based on these findings, a diagnosis of unseptated cervical CH was made. Chromosome karyotyping by amniocentesis was performed at week 16, yielding normal results: 46XY; there were no complications during this intervention.

Source: Image obtained during the study.
Figure 1 Ultrasound at 15 weeks of pregnancy showing simple cervical cystic hygroma. The arrow points to nuchal ligament.
At 20 weeks, follow-up was performed with anatomy ultrasound, showing bilateral clubfoot and persistence of a 32x28x8mm CH in the neck of the fetus. The estimated fetal weight was calculated at the 60th percentile according to the Hadlock IV formula (Figure 2). Fetal echocardiogram and neurosonography were normal. Monthly ultrasound monitoring was used for obstetric follow-up.

Source: Image obtained during the study.
Figure 2 Ultrasound at 20 weeks of pregnancy showing simple cervical cystic hygroma. The arrow points to nuchal ligament.
At 30 weeks, fetal magnetic resonance imaging (MRI) showed adequate neuronal development and neck with increased signal in the dorsal cervical region in T2 sequence, indicating a cystic component of 6mm in diameter and bilateral clubfoot (Figure 3). In subsequent ultrasound examinations, the finding of CH persisted.
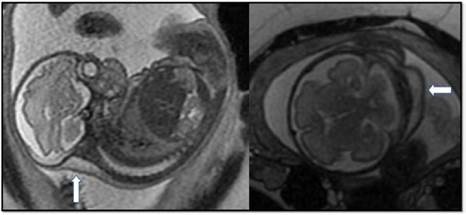
Source: Image obtained during the study.
Figure 3 Fetal MRI at 30 weeks. The arrow points to simple cervical cystic hygroma.
At 37 weeks, a cesarean section was performed due to uterine activity and suspected cephalopelvic disproportion. As a result, a male infant with spontaneous neonatal adjustment, weight of 2 825g, height of 46cm, and Apgar score of 9 at 5 minutes was obtained. The neonatal physical examination showed a neck with abundant, non-obstructive posterior cervical panniculus and no palpable masses, in addition to bilateral clubfoot; there was no evidence of limitation in arcs of motion. Between day 1 and 2 of life, the newborn underwent the following studies: ultrasound of soft tissues of the neck, which did not show any lesion suggesting CH, and otoacoustic emissions test, screening for congenital heart disease, and transfontanellar ultrasound, all of which were normal. After 48 hours of delivery, both the newborn and the mother were discharged.
In pediatric monitoring, performed at 6 months of age, the baby was found to have adequate neurodevelopment, no neck lesions (Figure 4), and orthopedic treatment with Ponseti technique for bilateral clubfoot. Since no syndromic diagnosis was established, the genetics service discharged the baby.
Case 2
A 21-year-old woman from Guateque (Colombia), a housewife, with a low socioeconomic status and no medical history, was referred from the Hospital de Guateque to the Hospital Universitario de La Samaritana in Bogotá in May 2020, when she was 20 weeks pregnant (obstetric formula G1P0V0), due to an ultrasound finding of cervical CH. On admission to the institution, an obstetric ultrasound was performed, showing an anechoic image of 23x32x36mm in the neck of the fetus and irregular echogenic contours, in which the nuchal ligament and multiple septa were observed, without color Doppler uptake, thus confirming the diagnosis of septal cervical CH (Figure 5). The estimated fetal weight was calculated at the 14th percentile according to Hadlock IV formula.

Source: Image obtained during the study.
Figure 5 Ultrasound at 20 weeks of pregnancy showing septal cervical cystic hygroma. The thick arrow points to the nuchal ligament and the thin arrows point to septa.
The patient was admitted and chromosome karyotyping by amniocentesis was performed on the same day, which was normal (46xx), as well as fetal echo-cardiogram and neurosonography, which were also normal. The obstetrics service followed up on the patient with monthly ultrasound monitoring, which showed persistence of septated CH in the fetal neck, with no new ultrasound findings.
At 37 weeks of gestation, the patient visited the hospital again due to regular uterine activity and had a normal vaginal delivery in which a live female newborn with spontaneous neonatal adjustment was obtained, with a weight of 2 550g, height of 46cm and Apgar score of 9 at 5 minutes. The only finding on physical examination was abundant nonobstructive posterior cervical panniculus (Figure 6).

Source: Image obtained during the study.
Figure 6 Postpartum check-up of patient with prenatal diagnosis of septated cervical cystic hygroma. Abundant posterior cervical panniculus is observed.
Postnatal ultrasound showed a 3x1x6mm cystic lesion dependent on subcutaneous cell tissue in the posterior neck region, without color Doppler uptake; ultrasound of the neck vessels, transfontanellar ultrasound, and ultrasound of the abdomen were normal. The echocardiogram, performed the next day after birth, showed a 1.2mm patent ductus arteriosus, although it did not have any hemodynamic repercussions; the other cardiac structures were normal. 48 hours after delivery, both the newborn and the mother were discharged.
A pediatric monitoring performed at 6 months of age found a baby with neurodevelopment according to age and no evidence of neck injury on physical examination. Given the evolution of the baby, the pediatric surgery service did not consider surgical treatment and the clinical genetics service discharged her.
DISCUSSION
CH is a tumor commonly located on the back of the neck that is caused by an obstruction of the lymphatic system and jugular vein and occurs near the end of the sixth week of gestation. In most cases, CH is associated with aneuploidy, hydrops fetalis, and other structural abnormalities that lead to voluntary termination of pregnancy or perinatal death 8,9.
The reported incidence of CH is 1 case per 1 000-6 000 live births and approximately 1 case per 750 miscarriages. Up to 51% of cases with this condition are associated with fetuses with euploid karyotype, of which approximately 17% have spontaneous resolution in utero. Most fetuses with CH and euploid karyotype have better perinatal outcomes than those with cystic hygroma associated with karyotype alterations, such as adequate birth weight and normal neonatal adaptation 1,9.
The first diagnostic suspicion of CH usually arises in the first trimester ultrasound, where a thickening of the nuchal fold >3mm 4 is observed; however, it has been considered that visualization in the cervico-occipital region of a cystic, bilateral and generally symmetrical area (septated or nonseptated) can also be considered to establish an ultrasound diagnosis 10.
Prenatal counseling requires the performance of a fetal karyotype test to rule out aneuploidy since, in euploid fetuses, close ultrasound monitoring is recommended, as well as anatomy ultrasound, echocardiogram and neurosonography to rule out the presence of other structural anomalies. Such anomalies are a determining factor to establish the prognosis of the gestation and decide on the possibility of expectant management, as their association with hydrops fetalis or other fetal malformations are poor prognostic factors that lead to unfavorable outcomes such as termination of gestation, intrauterine death, chromosomopathies, or spontaneous abortion in up to 91% of cases 4,7,8.
One of the causes of CH in euploid fetuses is Noonan syndrome, an autosomal dominant disorder belonging to the group of RASopathies and related to a group of phenotypically overlapping disorders caused by the RAS/MAPK pathway germline mutation in the PTPN11 gene, which requires prenatal diagnosis based on molecular study using amniocentesis or chorionic villus biopsy 11.
Prognosis in patients with CH has been studied according to tumor structure. Some authors have found a worse perinatal prognosis in fetuses whose lesion is >6mm on second trimester ultrasound 4 and in which septa are found 8; however, other studies have found no differences in terms of prognosis when evaluating these variables 10,12.
In the cases presented in this article, the mothers did not have a first trimester ultrasound, so the diagnosis of CH was made in the second trimester of pregnancy. Likewise, in both cases, amniocentesis was carried out to perform karyotype testing, although our limitation was that it was not possible to perform a molecular study for Noonan syndrome, which is a differential diagnosis in fetuses with euploid CH.
Similarly, the literature suggests that studies using microarray technology could increase the yield in the detection of genetic alterations of euploid fetuses with this disorder by 5% 13; however, this study was not available in the diagnostic approach of the cases presented here.
Notwithstanding the above, in both cases, a specialized prenatal imaging study was carried out that allowed to identify the presence of CH at the cervical level, one of which was septated with a diameter >30mm and associated with bilateral clubfoot. Also, in both cases, CH persisted in the ultrasound assessment during the third trimester and in the initial postnatal clinical assessment.
Unlike septated CH, the lesion was not identified in the nonseptated CH on follow-up soft tissue ultrasound performed in the first week of life. Septate CH resolved spontaneously at six months of life.
There were no differences between the two cases during neonatal adaptation or neurodevelopmental assessment. Furthermore, the genetic evaluation was normal and none of the patients required medical or surgical treatment at 12 months of follow-up, which shows, in general, a good perinatal and postnatal prognosis.
Concerning fetal therapy, the possibility of treating this type of tumor by means of fetal sclerotherapy has been proposed for more than two decades, mainly in euploid fetuses without major structural abnormalities and with a high risk of intrauterine death secondary to hydrops fetalis; however, the case series are small and there are no clear clinical parameters for their performance 4,14.
Regarding the route of delivery, in a study that included 626 pregnant women and only 9 were diagnosed with CH and normal karyotype, Behera et al. 15 found that the mode of delivery was cesarean section in 57% of these cases, which was indicated mainly due to abnormal position and presentation of the fetus or poor progression of labor. In the present study, one patient was delivered vaginally without complications and the other by elective cesarean section due to mechanical dystocia not associated with cervical injury.
Euploid fetuses with persistent CH at birth appear to have complete spontaneous resolution of CH in 28% of cases and a reduction of more than half the size in approximately 50% of cases at 1-year follow-up, even in those fetuses with lesions >50mm 15. It has been suggested that sclerotherapy with agents such as bleomycin in cases with large or persistent lesions has good response rates 4,15,16.
CONCLUSION
CH is considered a marker of poor prognosis in pregnancy; however, euploid fetuses with this type of tumor have a better perinatal prognosis if their lesion resolve, do not develop hydrops fetalis, and do not have other associated congenital malformations. Noonan syndrome should be considered as a differential diagnosis, and a multidisciplinary follow-up by pediatrics and genetics should be carried out in postnatal care.















