Introduction and objectives
Healthcare institutions have often renewed their anesthesia machines and monitors, at least in the course of the last decade and the general anesthetist is sometimes faced with the challenge of using these machines to administer anesthesia to a pediatric patient. In addition, there are different anesthetic circuits in terms of size and length, according to each patient. This article for reflection considers the case of anesthetists that treat children only sporadically, with a view to reducing the level of stress and properly fine-tune the anesthesia machines to the child, providing safety and quality tools for mechanical ventilation that increase the probability of success. We shall then define the term "Modern Anesthesia Machines," their main benefits, the basic mechan ical ventilation concepts applicable to anesthetized children, describing the primary ventilation strategies and, lastly, how to make the best use of graphic monitoring provided by the new anesthesia machines. In the end, we shall be able to answer the question: How do we make the best use of the new anesthesia machines and place their technology at the service of children?
The modern anesthesia machines
Arbitrarily and from a convenience perspective, this is the name we have given to those anesthesia machines that bear 3 characteristics: complete a previous self-check-up, exhibit ventilation modes other than the typical pressure or volume-controlled ventilation, and have monitoring charts of ventilation mechanics.
Self-check-up of anesthesia machines
Anesthesia machines must be calibrated before their use because of 2 reasons: the first is testing the correct functioning of the machine's sensors and internal devices; the second one is evaluating the anesthetic circuit to be used, measuring compliance, conducting leak tests, and estimating the internal volume. Both processes are intended to accurately ensure a tidal volume (Vt) that can be low enough (up to 5 mL Vt in some brands and up to 20 mL in most brands) and that the percentage of inhaled anesthetic agent delivered is accurate and with the least possible variability, with changes in fresh gas flow (FGF), hence allowing for small volumes, and even low metabolic levels (below lL/minute). These 2 characteristics meant that for many years, the preferred ventilation mode in pediatrics was pressure-controlled, which additionally compensated for small circuit leaks. Furthermore, the variability of the anesthetic agent with FGF changes forced us for many years to avoid the use of metabolic flows-not even low-in the pediatric population. Both of these scenarios are now possible and reliable: low Vt and low FGF.1,2
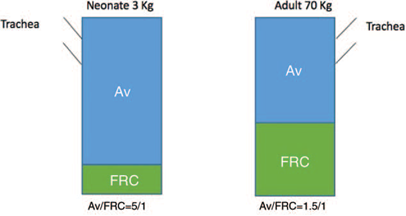
Compliance
The term compliance refers to the change in volume due to pressure changes. In anesthesia circuits, compliance is determined by the ability of the circuit wall used to be compliant, and by the compression of the air molecules inside the circuit when applying pressure, as these molecules are initially compressed and then generate pressure on the walls. Thus, a small, short, and stiffcircuit will be more compliant that a wide, soft, and long circuit. The goal is to have a circuit compliance as close as possible to the pulmonary compliance of the patient, as some machines also make a "dynamic" adjustment during each respiratory cycle, identifying abrupt changes in compliance and correcting them. A large differential between the circuit and the patient's compliance hinders or "fools" the machine sensors to perform this function. With this information, the machine compensates for the volume of air "lost" in the circuit's compliance to make sure that the patient receives the accurate programed volume. 1,2
Leak test
Machines usually tolerate and make up for any minor leaks of less than 250mL/minute. During calibration, it is important to establish, together with the manufacturer, if capnography should be installed, as it suctions around 150mL of air per minute, which in some models return back to the respiratory circuit, but in other cases are expelled and hence must be compensated for. This fact is critical in patients less than 20kg, since this non-compensated leak may represent a considerable percent age of the Vt.
Internal volume
This volume refers to the amount of air handled by the anesthesia machine up to the "Y" circuit; in other words, the circuit volume itself, the volume of the canister, the reservoir bag, the internal circuits, and the mechanical ventilator. This volume ranges from 4 to 8 L and certainly varies according to the reservoir bag used (e.g., 3-0.5 L), to the ventilator system (piston or coil, adult, or pediatric) and to the anesthesia circuit itself. The relevance of this volume is that the machine must saturate that volume with anesthetic agent for a reliable and accurate delivery to the patient. The saturation time of this internal volume is called the "K" time constant. The higher the internal volume, the longer it takes for any changes in the dial of the vaporizer to be actually reflected in the patient's airway. Here lies the importance of having the machine estimate this volume and set the sensors to deliver the anesthetic agent during check-up. Moreover, by enhanc ing the precision and reliability of these 2 aspects, the mechanical ventilation setting will be based on the right parameters.
Mechanical ventilation in the anesthetized child
The most important differences and physiological aspects to be considered when ventilating a child are:
Compliance: The child's pulmonary parenchyma has a low compliance that increases with age. The chest wall is quite compliant, mainly as a result of the horizontal cartilaginous nature of the ribs and the meager muscle mass of the child. This results in the need for adequate pressure to open up the alveoli (low pulmonary compliance) with a risk of volutrauma and barotrauma due to the subsequent poor chest wall resistance as a result of its high compliance. 3,4
Airway resistance: Newborn babies have a very high airway resistance that decreases until it reaches the adult values at around 8 years of age. Inserting a small diameter endotracheal tube further increases this resistance. 4
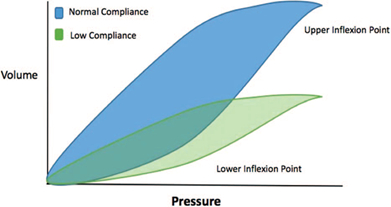
Functional residual capacity: It is the combination of the reserve expiratory volume and the residual volume; in children, it is proportionally less than in the adult and than the total pulmonary capacity. The functional residual capacity is the only oxygen reserve in case of apnea, so the child is overtly vulnerable because of this diminished reserve (Fig. 1). 4
Source: Authors
Figure 1 Functional residual capacity. Av=alveolar ventilation; FRC=Functional residual capacity; Av/FRC=alveolar ventilation/ Functional residual capacity.
Closing volume: It is the minimum volume that should be left inside the alveoli to prevent their collapse; in the child, this volume is proportionally larger than in the adult. In other words, there must be a larger amount of air left in the lungs to prevent collapse. In adults, this volume approaches the residual volume, whereas in children, it approaches the Vt (Fig. 2), with a marked tendency to develop atelectasia. 4

Source: Authors.
Figure 2 Closing volume. ERV=expiratory reserve volume; RV= residual volumen; FRC=functional residual capacity; IRV=inspiratory reserve volume; TV=tidal volume.
Mechanical ventilation: It is hard to believe that although children are ventilated under anesthesia every day, the available literature is poor, with little evidence. Hence, most of the guidelines to ventilate children under anesthesia are derived from adults or from critical children ventilated in the Intensive Care Unit (ICU). 1-3,5-7 Certainly, these are patients with very different characteristics to those undergoing anesthesia that usually present with healthy lungs. 4 Hence, the primary parameters derive from "pulmonary protection ventilation" (PPV) based on 3 aspects applied to any of the ventilation approaches selected:
Low tidal volume: A fair number of trials have shown that both a high Vt (above 10mL/kg), and an extremely low Vt (below mL/kg) results in greater injury; therefore, the recommendation is 6 to 10 mL/kg1-4,8-11.
Positive end expiratory pressure: This parameter shares the strongest consensus; it is a must to keep the alveolus opened. At least the physiological positive end expiratory pressure (PEEP) must be programed, ranging between 5 and 8 cmH2O. Higher values will be needed, however, to improve oxygenation or when the child is discharged from the ICU under mechanical ventilation and high parameters. From the first year of life, approximately 40% to 50% of the positive pressure in the airway translates into intrapleural positive pressure, with the corresponding impact on the pressure gradient in the extrathoracic veins and the right atrial pressure. So the recommendation is to maintain an adequate effective circulating volume expansion. Please remember that PEEP is contra-indicated in patients with endocranial hypertension, hypovolemia, severe cardiovascular involvement and in the presence of high-flow bronchopleural fistula; in the latter case, the idea is to reduce mechanical ventilation as fast as possible because it has been proven that by reducing the airway pressure, the air leak flow drops, hence promoting the fistula closure. 1,2,4,9-11 With regard to the intracranial pressure (ICP), what really matters is to preserve an adequate cerebral perfusion pressure (CPP), which in infants is between 40 and 50mm Hg, 50 to 60mm Hgin children, and over 60mm Hg in adolescents. As normally we don't measure the ICP in these patients, the central venous pressure is used as an indirect ICP measure ment. Thus, the calculation of CPP would be equal to the mean arterial pressure.
Alveolar recruitment: Two events take place during anesthesia that highly predispose the development of atelectasis: an elevated FiO2 and the disruption of the anesthetic circuit because of airway suction, or any other event. 3 Considering and controlling these 2 aspects is as important as keeping in mind alveolar recruitment to "open up" the alveoli that collapsed during mechanical ventilation. Alveolar recruitment means maintaining an airway peak pressure (AWPP) sustained for a period of time. We usually raise the AWPP from 35 to 40cmH2O for 20 to 40 seconds. There are different variables of this basic recruitment, with multiple advantages that are beyond the scope of this article; however, probably the most helpful would be a step-wise increase of the AWPP maintaining the pressure drive (difference between AWPP and PEEP) between 15 and 20 cmH2O measuring the compliance that should increase with each step, until it rises no more, or drops. This is when optimum recruitment is considered, as long as the is no previous hemodynamic decline of the patient because in that case the alveolar recruitment maneuver shall be interrupted. 2,9-11 This recruitment maneuver is extremely useful in ICU with extended mechanical ventilation and is not usually required in the OR, unless the procedure takes several hours, or in the presence of hypoxemia, with the potential to cause hemodynamic instability.
Major ventilation modalities used in pediatric anesthesia
Pressure controlled ventilation
This is the most popular ventilation used in pediatric anesthesia. Basically, the ventilator supplies an airflow until a previously programed pressure level is achieved. In this case, a square pressure-time curve results, and a decelerated time-flow curve or shark-fin curve. Its advantage is to limit the potential for barotrauma, by restraining the peak inspiratory pressure (PIP), compensating for small leaks, as it controls PIP rather than volume; finally, the decelerated flow which allows for reaching a larger number of distal alveoli by reducing turbulent flow. The major disadvantage is the inability to establish an accurate Vt (which is fundamental under the current pressure controlled ventilation [PCV] parameters) as the Vt varies from cycle to cycle according to PIP, which is mostly determined by pulmonary compliance. There are however other variables such as the pressure exerted by the surgeon on the chest of the patient, or partial endotracheal tube obstructions, among other factors. 1-4,6
Volume controlled ventilation
This ventilation modality is often used in pediatric anesthesia but in its "synchronized" version (synchro nized intermittent mandatory ventilation [SIMV]) and with "support pressure" (SP). The primary modality ensures through programing a Vt to be delivered by the anesthesia machine, and this is indeed its advantage. Remember that 1 of the 3 pillars of PPV is ensuring a low Vt. The disadvantages include that such Vt is delivered, regardless of the PIP, raising the risk of barotrauma: moreover, there may be losses from the endotracheal tube leaks (i.e., when using pneumoplug). When ventilating with volume controlled ventilation (VCV), a square flow-time curve is obtained, whereas the pressure-time curve is a shark-fin curve with a plateau (if there is a programed inspiratory break) allowing to determine the plateau pressure (Pplat), which is important for the analysis of the ventilation mechanics. 1-4,6
Support pressure
SP involves a flow throughout the inspiratory phase at a pre-determined pressure; however, the inspiration is initiated by the patient so that the primary condition for its use as a unique ventilation modality is the presence of ventilation stimulus in the patient. SP relieves the patient's ventilation effort and is the best approach to synchronize the patient with the ventilator. Furthermore, SP is a modality that may-and in our opinion should-be accompanied by other ventilation modalities in order to assist and relieve the respiratory effort during spontaneous ventilation. This is the ideal modality for the ventilation weaning process. The higher the SP, the Vt rises and the need for a higher respiratory rate decreases, and vice versa. The minimum SP level is considered to be 8 cmH2O so as to overcome the resistance created by the unidirectional valves of the anesthesia machine, the endotracheal tube, and the hoses of the anesthesia circuits. The highest recommended level is 20cmH2O. 2,6
Synchronized intermittent mandatory ventilation
This ventilation modality is intended to improve the patient-ventilator relationship, enabling the patient to do spontaneous ventilations; in other words, once the ventilator detects any inspiratory effort, it inhibits the delivery of the respiratory cycle and allows the patient to perform. This is when SP becomes relevant to adequately assist these spontaneous respiratorystimuli. SIMVmaybe adapted either to the pressure modality or to the volume modality: SIMV-Pressure Control (PC) or SIMV-Volume Control (VC). The anesthetist determines the "trigger flow" which is the flow or inspiratory pressure needed by the patient in order for the ventilator to allow and assist spontaneous ventilation. Poor ventilator programing under this modality will place the child at risk for hypoventilation and hypercapnia. 3 Although the SIMV is still broadly used, other ventilation modalities are increasingly being selected to lower the risk of asynchrony such as bi-level, and ventilation with adaptive support; however, this requires skills and specific training, so these methods are mostly used in intensive care.
Dual ventilation
Among the various ventilation options, there is no evidence of one being clearly superior to the others. Each modality has pros and cons and must be adapted to the particular situation. However, it seems reasonable that a ventilation modality that uses the best of the pressure modality and the best of the volume modality should be appropriate; in other words, a modality that ensures an accurate Vt, cycle after cycle, with a limited maximum pressure. This modality exists, and generally speaking it is called dual modality; however, each brand of anesthesia machines gives it its own name. The most common denomination is PCV with volume guaranteed (PCV-VG). With this approach, regardless of any changes in compli ance or PIP of the child, the machine will make the necessary changes to ensure Vt distribution, and hence, a stroke volume within the programed pressure limits. When these levels are not achieved, despite the anesthe sia machine compensatory modes, the machine gives a warning sign via the various alarm mechanisms. This is a quite convenient modality in situations where frequent and broad airway pressure changes occur, as for instance during laparoscopic and thoracoscopic procedures. 2,9 Actually some anesthesia machines provide ventilation modalities that were typical of intensive care, such as airway pressure release ventilation, but there is no conclusive evidence in children about its benefits in anesthesia, and its routine use would require special training for the general anesthetist.
Which is then the final suggestion?
Being reasonable with the literature findings, the sugges tion for general practice is that once the airway has been secured, manual ventilation shall proceed to confirm the correct placement of the devices and an adequate ventilation of the pulmonary fields. Then, if the patient received a neuromuscular relaxant, probably the best recommendation is to program the dual mode (PCV-VG). If neuromuscular relaxation has not been used, as is probably the case in most pediatric anesthesia cases may be, the most appropriate modality would be SIMV under the volume or pressure mode, always concurrent with SP: SIMV + SP. Regarding the end of the surgical procedure, when ventilation weaning begins, and making sure that there is no lingering effect of neuromuscular relaxants, the expectation is that the patient develops an adequate respiratory pattern to change over to the SP mode at a level of 8cmH2O and increasing trigger flow as the patient recovers awareness and muscle strength. Finally, based on the state of awareness and the respiratory mechanics, the decision to remove the airway device is made. Along the lines of respiratory mechanics, before removing mechanical ventilation, we must make sure that the child reaches a Vt of at least 6 mL/kg, a respiratory rate consistent with the child's age, an etCO2 below 40 mm Hg, together with a trigger flow of at least 1.0 for infants less than 1-year-old and of 2.0 for older children (Fig. 3).
Ventilation monitoring in the modern machines: curves
One of the key features of the modern anesthesia machines is the broad range of information provided about the ventilation mechanics cycle after cycle; in our opinion, this is the least used characteristic by anesthetists. We will particularly discuss 4 graphs:
(a) Spirometry: There are 3 types of loop type curves (starting and ending at the same point) according to what is being monitored.
Flow-volume loop and flow-pressure loop: These are possibly the least used modalities by anesthetists and the shape of the waves gives us an idea of the endurance of the small airways, or the airflow restrictions, as well as of the high or low airway obstruction, all with a single glance. We shall dwell on the third type of loop that could provide more useful information for the patient's ventilation. 2,4
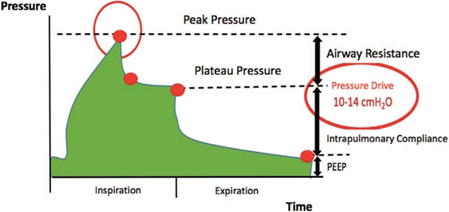
Pressure-volume loop: This loop is more widely used by anesthetists and allows for charting pressure on the X-axis and volume on the Y-axis. At a glance, it is possible to identify the pulmonary compliance cycle after cycle and any changes therein. When the curve flattens, that is an indication of a decrease in pulmonary compliance (Fig. 4). The machines allow for storing a "reference" loop from the beginning and to compare against this loop whatever happens during surgery. Furthermore, the lower inflexion point may be established, which is the point at which the slope of the curve changes from flat to ascending during inspiration and is used as a means to determine the ideal PEEP. We may also determine at the end of this curve whether a "duckbill" to the right occurs, indicating alveolar overdistension which should be corrected immediately by adjusting the Vt and/or the PIP parameters, according to the ventila tion mode. The descending expiratory curve follows a different trajectory than the ascending curve; this phenomenon is called hysteresis and is due to different forces acting during inspiration and expiration, because the latter is dominated by a passive process of pulmonary elastic recoil. The loop area reflects the pulmonary volume being used. Based on all of these characteristics, the pressure-volume loop is usually preferred for ventilation monitoring, as most machines only show 1 of the 3 loops described on the screen. 2,4
(b) Pressure-time curve: This curve depicts pressure on the "Y" axis and time on the "X" axis. A pressure mode results in a square wave with the highest plateau representing the maximum peak pressure and the lower level representing the PEEP value. The most relevant information of lung mechanics may be obtained from the volume-controlled mode using a certain amount of inspiratory pause to obtain a shark-fin type graph indicating 3 points and 2 intervals each with specific significance. The maximum pressure point corresponds to PIP, which combines pulmonary resistance and the airway resistance basically deter mined by the endotracheal tube. Then there is a drop in the curve toward an extended plateau, based on how we program the inspiratory pause. This plateau corresponds to Pplat, which is the balance pressure of all the alveoli and hence is a reflection of intra-pulmonary pressure. The third point corresponds to the lower level where the curve drops and coincides with the PEEP level we programed or which the patient is producing and must be adjusted according to each individual patient needs (Fig. 5). There are 2 intervals in between these 3 points. Between PIP and Pplat the airway resistance is determined which in this case is due to the endotracheal tube. This value is around 5 cmH2O and should not exceed 8 to 10cmH2O. Beyond this level, it is an indication of a high endotracheal tube resistance issue, for instance, a tube bend, partial obstruction form secretions, or a very small tube for the size of the child, inter alia. A high PIP with a normal interval of resistance involves a high Pplat and this is the result of changes in pulmonary compliance. The second interval is the so-called "pressure drive" which presents between PEEP and Pplat. This should not exceed 14cmH2O and ideally should be maintained at a value below 10cmH2O. A big difference involves the need for a large pressure and volume to open and keep the alveoli opened, forcing us to adjust the ventilation parameters, for instance, raising the PEEP level. Both the resistive pressure and the pressure drive above normal have been associated with adverse outcomes in critically ill patients in the ICU, particularly a longer hospital stay and mortality. 5 There are no studies relating these findings with the anesthetized child, usually with healthy lungs. However, due to the lack of better evidence, we suggest taking these limits into account for ventilating anesthetized children. 4
(c) Flow-time curve: This curve represents the flow in liters per minute on the "Y" axis versus time on the "X" axis. If we are dealing with VCV, the result will be a square wave, because the flow will enter and remains constant throughout the inspiratory. In the PCV mode, the flow will reach a maximum peak when it reaches the programed pressure, and from there on, there will be a drop graphically represented as decelerator in the rest of the inspiratory phase until the end of the phase. The expiratory phase is equally traced in both modes. With this type of curve, a single observation is enough to determine the inspiration:expiration ratio (I:E) and if the times are sufficient, for instance, if an inspiratory cycle begins before the expiratory curve reaches the basal level, that would be indicative of a very tight I:E ratio that may result in reinhalation and CO2 retention. Moreover, this curve may identify inspiratory effort by the patient depicted as wave notches and determine whether these are followed by ventilation support so as to help to adjust the patient-ventilator synchrony. A strategy for improving oxygenation is to shorten the I:E ratio, even inverting it, and a strategy for CO2 removal is to increase the I:E ratio even beyond 1:3. All of these changes can be confirmed, followed, evaluated, and adjusted through observation and analysis of this curve. 4
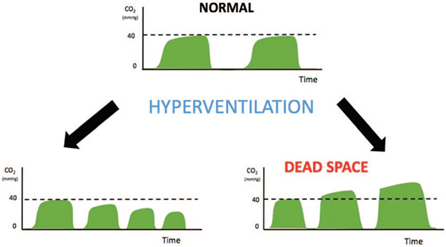
(d) Capnography: Finally, the graphical representation of CO2 detection throughout the expiratory cycle is the origin of capnogaphy. Traditionally, medical doctors believe that these graph is only useful to see whether the patient is intubated or not, but these rationale dismisses several other fundamental uses. Capnography in terms of its value and shape helps to assess the ventilation mechanics and pulmonary function, 1,3 delivering pathognomonic curves, for instance, for bronchospasm (overtly ascending plateau). Furthermore, it should be considered as an indirect measurement but proportional to cardiac output, in as much as CO2 is determined on the basis of pulmonary blood flow, which is also dependent on cardiac output. Hence, if there are no ventilator changes and CO2 starts to drop, this maybe the start of a hypotension period of time. 4 The applications and complete interpretation of capnography is beyond the scope of this article, but there is a need to stress its forgotten value which is extremely important in pediatric ventilation.
Capnography helps to determine the presence of uncorrected dead space in our ventilation strategy as follows: once the ventilation strategy has been established and a level of capnography stabilized, advance to manual ventilation administering some cycles of hyperventilation (5 cycles are enough); in other words, manually increase PIP and Vt. Under the usual conditions, such a short-lasting hyperventilation should decrease the capnogaphy level or at least maintain it. If the value increases, this is a reflection of a dead space that prevented the Vt to effectively reach the child and with this hyperventilation the spaces are "swept," obtaining the CO2 that was not previously discharged (Fig. 6). In this case, the Vt must be adjusted. Particularly in small children (less than 10 kg), the programed Vt may be insufficient when adding elements to the circuit after the "Y"-where the dead space begins-without compensating. Remember that the definition for dead space is the segment of the circuit where the flow becomes bidirectional and may be mixed; that means, from the "Y" but not before. For instance, the length of the inspiratory and/or expira tory branches do not affect the dead space (it may affect the circuit compliance, the compression of the air molecules, the internal volume, etc., but not the dead space). Devices such as extensions, filters, elbow joints, capnography sensors, humidifiers, and so on make up a volume that can be as high as 25 mL1,2. For instance, in a premature 2-kg baby, programing a Vt of 10 mL/kg will result in 20 mL of Vt, which means that the Vt cannot even move from the filter and the child would be absolutely hypoventilated. Under this cir cumstances, the above maneuver is extremely helpful.
Conclusion
Based on the above discussion, could we learn how to make the best use of the new anesthesia machines and use that technology for the benefit of children? This can be summarized into the following practical considerations:
Pre-calibrate your machine with the appropriate circuit to be used: This maneuver enables the evaluation of sensors, determines the internal work volume of the machine, establishes and automatically compensates for compliance and minor circuit leaks. In this manner, we will ensure an accurate though small Vt and a reliable delivery of anesthetic gases.
Determine the most appropriate ventilation mode for each particular case: Regardless of the mode selected, whenever possible add SP (between 8 and 20cmH2O), determine a Vt (6-10mL/kg), always PEEP (at least the physiological: 5-8cmH2O), keep the alveolar recruit ment maneuvers in mind and decrease the alveolar disrecruitment maneuvers (unnecessarily high FiO2 and frequent circuit disconnections with airway suction), keep the Pplat below 20cmH2O and the pressure drive below 14cmH2O. Remember that dual ventilation theoretically delivers excellent advantages (evidence is lacking).
Make use of the monitoring charts: Remember that 3 spirometry loops that at first sight help to evaluate compliance, the ideal PEEP value, alveolar overdistension, pulmonary restrictive, and obstructive processes, inter alia. The pressure-time and flow-time curves help to fine-tune mechanical ventilation, regulating PIP, Pplat, PEEP, airway resistance, pressure drive, I:E ratio, and patient-ventilator synchrony, inter alia. All of these are extremely helpful. Lastly, keep in mind that capnography with a simple maneuver allows for the determination of any poorly ventilated excessive dead space.
Be acquainted with your anesthesia machine: If you are aware of the virtues of your anesthesia machine and make use of them for the benefit of anesthetized children, we could turn mechanical ventilation into a simple, practical, and, above all, safe and useful strategy when delivering general anesthesia.
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.