Introduction
Family planning is a human right enshrined through reproductive health policies aimed not only at restricting births, but also at promoting deliberate decision-making about the responsibility of having children who are wanted and in the right circumstances.1 In this sense, health services have the obligation to educate the entire population about contraception, as well as to provide contraceptive methods and monitor their use.
In 1994, the need to promote male sexual and reproductive health was recognized within the framework of the International Conference on Population and Development. For this reason, a plan of action was proposed to insist on the need to make the population aware of men's responsibility in family planning and to promote their active participation in said activity by encouraging the use of different contraceptive methods,2 including vasectomy, the most effective and widely available permanent male contraceptive method at present.3
Worldwide, the rate of both male sterilization and rhythm method users dropped considerably between 1994 and 2019, going, according to the United Nations,4 from 43 million to 16 million and from 36 million to 29 million, respectively. It has been established that vasectomy use is very limited. For example, Lincoln et al.5 reported in a review that although sterilization is the most common method of pregnancy prevention worldwide, 180 million women rely on this method, while only 43 million men opt for vasectomy. In turn, the United Nations6 stated in 2020 that although Latin America is one of the regions in which the use of modern contraceptives has increased, the number of male sterilizations is very low, whereas female sterilization is widely used.
In a psychosocial study, Hernández-Aguilera & Marván-Garduño7 found that men in developing countries are less likely to opt for vasectomy as a contraceptive method due to various fears related to misinformation and lack of knowledge about the procedure, in addition to the idea that women are responsible for contraception. Moreover, these authors also state that most of the fears concerning the procedure are of a sexual nature.
In order to improve the understanding of the topic and strengthen sex education programs with an equitable medical approach in the long term, the present study aimed to describe the level of knowledge, perception, and level of acceptance of vasectomy (i.e., whether participants would recommend it to their patients and, in the case of men, whether they would undergo it at some point in their lives) in a sample of Latin American medical students.
Materials and methods
Study type and sample
Multicenter, analytical, cross-sectional study conducted in November 2020. The study population consisted of medical students (1st to 7th year) enrolled in medical schools of public and private universities in 8 Latin American countries (Bolivia, Brazil, Chile, Colombia, Ecuador, Mexico, Panama, and Paraguay). Participants were recruited by convenience sampling taking into account the following inclusion criteria: being over 18 years of age and agreeing to participate voluntarily in the study by signing the informed consent form. Students who did not complete the questionnaire used were excluded. The final sample consisted of2 676 students.
Instrument and procedures
An instrument adapted from the questionnaire administered to Colombian medical students by Torrado-Arenas et al. 8 was used for data collection, from whom the corresponding authorization was received for its use. The questionnaire was culturally adapted by the authors of the present study and validated in each of the eight countries through an individual process where the adapted version was reviewed by an expert in urology and university teaching in each country to make some modifications, such as changing the order and wording of some questions without removing any of them and adding more inclusive response options for all participants. The adaptation process was carried out prior to a pilot test with 30 students in each country to ensure that they understood the questionnaire correctly. The same questionnaire was used in all countries, except in Brazil, where a version translated into Portuguese was used, following the same validation and cultural adaptation process.
The instrument used consists of two parts, one is the informed consent form and the other is the questionnaire itself, which is made up of 28 items grouped into 4 domains: the first one includes 8 questions on sociodemographic variables; the second one contains 14 questions that assess general knowledge about vasectomy based on a performance ranking scale depending on the number of correct answers (low: <6, medium: 7-10 and high: 11-14); the third comprises 4 questions related to the perception of vasectomy; and the fourth consists of 2 questions related to the level of acceptance of vasectomy. Except for the questions in the first module (sociodemographic), which had multiple choice answers, all were dichotomous. The full questionnaire is available in Annex 1.
Once the validation and cultural adaptation phase of the two versions of the questionnaire (Spanish and Portuguese) was completed, they were entered into the Google Forms platform, and the study began to be disseminated through social networks on October 20, 2020. Only the questionnaires completed up to November 20 were taken into account, obtaining 2 736 responses, of which 2 676 were selected after applying the inclusion and exclusion criteria.
Statistical analysis
The information was compiled in a Microsoft Excel 2016 database, where the data were organized by country of origin of the participants.
In the descriptive analysis, absolute frequencies and percentages were used for categorical variables, while means and standard deviations were used for continuous variables; the distribution of the latter was evaluated using the Kolmogorov-Smirnov normality test. Furthermore, using the chi-square test of independence, the differences between the three variables studied (level of knowledge, perception, and level of acceptance of vasectomy) were determined based on the following categories: country of origin, sex, religious affiliation, and level of medical training for the first variable, and country of origin and level of knowledge about vasectomy for the second and third variables. All statistical analyses were performed using SPSS 25.0, while figures were created using GraphPad Prism version 8. A significance level of p<0.05 (two-tailed) was considered.
Ethical considerations
The study took into account the ethical principles for research involving human subjects established in the Declaration of Helsinki.9 Additionally, the study was approved by the Research Ethics Committee of the Faculty of Health Sciences of the Universidad Católica Nuestra Señora de la Asunción of Paraguay according to Minutes No. 21 of October 18, 2020. All participants gave their informed consent for participation in the study.
Results
The mean age of the participants was 22.0 years, with a range between 20.00 and 24.00 years, and 59.38% (n=1 589) were female. The average number of respondents per country was 333.37 people, with Chile and Mexico being the countries with the highest number of participants (414 and 379, respectively).
Among the participants, 20.62% were in their third year of undergraduate studies, and 11.28% were finishing their studies (sixth and seventh year); it was also found that 58.59% identified themselves as Catholics, 84.6% stated that they were heterosexual, 94.84% were single, and 3.84% had children (Table 1).
Table 1 Baseline characteristics of the study population (n=2 676).
| Age in years (mean±standard deviation)) | 22.2±3.2 | |
| Sex, n (%) | Male | 1 087 (40.62%) |
| Female | 1 589 (59.38%) | |
| Country of origin, n (%) | Bolivia | 310 (11.58%) |
| Brazil | 330 (12.33%) | |
| Chile | 414 (15.47%) | |
| Colombia | 312 (11.66%) | |
| Ecuador | 301 (11.24%) | |
| Mexico | 379 (14.16%) | |
| Panama | 309 (11.55%) | |
| Paraguay | 321 (11.99%) | |
| Sexual orientation, n (%) | Heterosexual | 2 267 (84.71%) |
| Bisexual | 233 (8.71%) | |
| Homosexual | 133 (4.97%) | |
| Pansexual | 24 (0.89%) | |
| Other | 19 (0.71%) | |
| Marital status, n (%) | Single | 2 538 (94.84%) |
| Domestic Partnership | 88 (3.28%) | |
| Married | 43 (1.60%) | |
| Divorced | 6 (0.22 %) | |
| Widowed | 1 (0.03 %) | |
| Children (yes), n (%) | 103 (3.84) | |
| Religion, n (%) | Catholicism | 1568 (58.59) |
| None | 703 (26.27) | |
| Atheism/agnosticism | 171 (6.39) | |
| Christianity | 91 (3.40) | |
| Other | 143 (5.34) | |
| Year of medical training, n (%) | First | 410 (15.32) |
| Second | 519 (19.39) | |
| Third | 552 (20.62) | |
| Fourth | 501 (18.72) | |
| Fifth | 392 (14.64) | |
| Sixth | 181 (6.76) | |
| Seventh | 121 (4.52) | |
Source: Own elaboration.
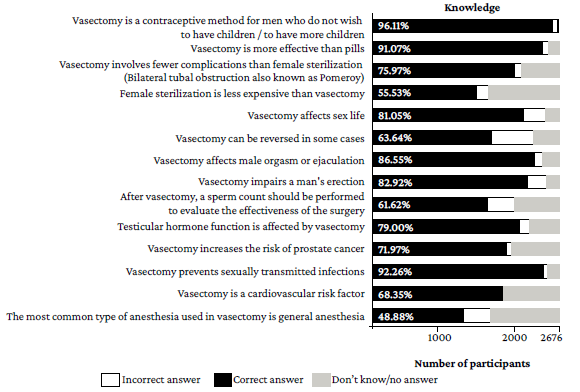
Regarding the level of knowledge of the procedure, it was found that 55.38% of the participants had a high level (11-14 correct answers); 36.32%, a medium level (7-10 correct answers), and 8.29%, a low level (<6 correct answers). The questions that most students answered correctly were those related to the purpose of the procedure and its effectiveness in preventing sexually transmitted infections (96.11% and 92.26%, respectively). In contrast, the question with the lowest number of correct answers was whether general anesthesia is the most commonly used method in vasectomy with 48.88%, followed by whether female sterilization is less expensive than vasectomy with 55.53% (Figure 1).
When comparing the knowledge of the participants who engaged in some religious practice versus those who did not, it was found that the majority of students in the latter group had a high level of knowledge (70.41%), while only 8% of the group of students who identified themselves as Christians had a high level of knowledge.
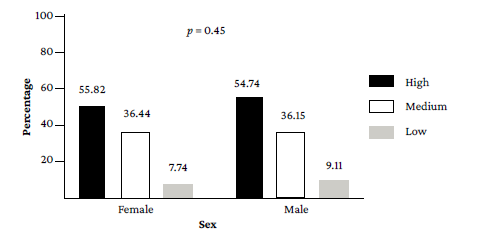
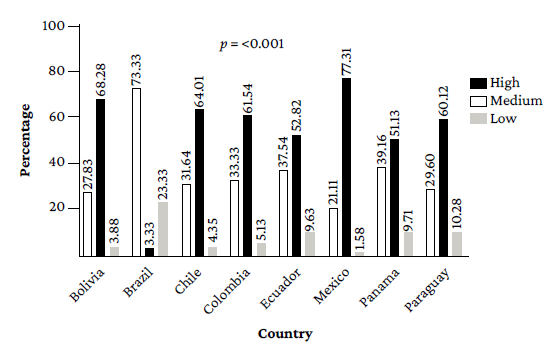
No significant difference was found in terms of participants' level of knowledge by sex (p=0.45) (Figure 2); however, significant differences were observed by country of origin (p<0.00l): most students in Mexico and Bolivia had a high level of knowledge (77.31% and 68.28%, respectively), while in Brazil only 3.33% had a high level of knowledge (Figure 3).
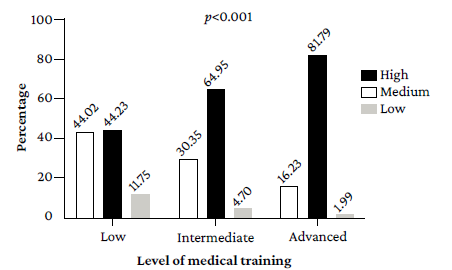
Significant differences were also found in the level of general knowledge about vasectomy among students depending on their level of medical training (p<0.001), as the percentage of students at advanced levels who demonstrated high knowledge about the procedure was higher (81.79%) than those at basic levels (44.02%) (Figure 4).
Source: Own elaboration.
Figure 4 Differences in level of knowledge by level of medical training. Basic: 1-5 term; Intermediate: 5-10 term; Advanced: >10 term.
Regarding the perception of vasectomy, 96.97% of the participants thought that vasectomy does not affect masculinity, 97.31% did not consider it a sin, and 98.99% stated that contraception is not only a woman's responsibility. In addition, for 58.56%, the opinion of someone close to them (friends, relatives, or a romantic partner) is important when making the decision of having a vasectomy or not. Students with a high level of knowledge were the ones who most commonly considered that contraception was not only a woman's responsibility, that vasectomy does not affect masculinity, and that having it done is not a sin, but interestingly, these same students were the most likely to consider the opinion of someone close to them as important when making the decision of whether or not to undergo the procedure (41.36%) (p<0.001).
When analyzing perception by country, it was observed that responses were very similar. However, in Bolivia, vasectomy was most often considered to affect masculinity (3.55%), while in Brazil the majority of students (92.12%) do not consider the opinion of family or friends to be important for deciding to undergo the procedure; in Colombia, no student considered vasectomy to be a sin.
Regarding the level of acceptance of vasectomy, 94.02% of the participants would recommend this procedure to their future patients and acquaintances; in fact, those who did so the most were students with a high level of knowledge (56.87%). This finding on acceptance contrasts with what was found in the question asked only to men about whether they would have a vasectomy at some point in their lives, as only 69.82% indicated that they would (Table 2).
Table 2 Acceptance of the procedure by level of knowledge.
| Level of knowledge | Would you recommend vasectomy to a patient or acquaintance? | Answer only if you are a man, would you have a vasectomy at any time in your life? | ||
|---|---|---|---|---|
| Yes | No | Yes | No | |
| High | 1 431 (96.55) | 51 (3.44) | 458 (76.89) | 137 (23.10) |
| Medium | 904 (93.00) | 68 (6.99) | 50 (54.34) | 42 (45.65) |
| Low | 181 (81.53) | 41 (18.46) | 251 (62.75) | 149 (37.25) |
| p-value | <0.001 | <0.001 | ||
Source: Own elaboration.
Finally, when analyzing the level of acceptance of vasectomy by country, it was found that Mexico had the highest number of participants who would consider undergoing it (83.87%), while Panama had the highest number of students who refused the idea (51.02%).
Discussion
Vasectomy, although a safe, cost-effective and gender-equitable method of contraception, has historically been underused, particularly in low-income countries with a great need for sexual and reproductive education.10 Regarding the latter, it has been reported that the fact that vasectomy is less common as a contraceptive method in Latin American and Middle Eastern countries may be the result of a lack of knowledge about the procedure, which leads to false beliefs, mainly of a sexual nature, and represents an important barrier to its promotion.7
In the present study, it was found that medical students in general have a good knowledge of vasectomy (55.38% have a high level and 36.32% have a medium level), and that the more advanced their medical training, the higher their level of knowledge: while 81.79% of students in more advanced terms demonstrated a high level, only 44.02% of students with a basic level did so.
Highly knowledgeable participants were the most likely to state that they would recommend vasectomy to a patient or acquaintance. This finding is similar to that reported by Ohn Mar et al,11 who administered a cross-sectional survey to 330 Malaysian medical students and, based on their results, suggested that participants' knowledge of and attitudes toward vasectomy improved as they progressed through their medical training, because when asked whether they would prefer vasectomy to female sterilization if the partner looked for a permanent contraceptive method, 30.7%, 41.2%, and 50% of the 5th-4th-3rd year students, respectively, said yes. These findings also concur with those of Muñoz-Pérez et al.,12 who conducted an observational study in 111 men from Ecatepec, Mexico and concluded that having more information about vasectomy was significantly associated with a higher probability of agreeing to undergo the procedure (p<0.05).
On the other hand, in the present study it was found that the participants had large gaps in knowledge regarding the type of anesthesia used in the procedure and its costs compared to tubal ligation, as such questions were answered correctly by only 48.88% and 55.53% of the participants, respectively. This is in agreement with Torrado-Arenas et al.,8 who reported, in a study in 112 medical students in Colombia, that 49.10% of the participants did not know what the difference between the costs of vasectomy and tubal ligation was, and most were unclear about the type of anesthesia used in the procedure.
Although in the present study participants who did not subscribe to any religion performed better in the level of knowledge and were more likely to express greater acceptance and recommend the procedure, it is most likely that the level of acceptance depends directly on their knowledge, since the religious beliefs of the participants were not associated with the perception of vasectomy or its acceptance (p<0.001) when they had good knowledge, further ruling out that vasectomy is a sin. This finding is similar to that reported by Ohn Mar et al.,11 who found no significant association between religion and the perception and acceptance of vasectomy in their study.
The majority of participants in the present study recognized that contraception is not the sole responsibility of women (98.95%), and that the procedure does not affect masculinity (96.93%), which contrasts markedly with the cultural traits typical of machismo in Latin America as documented by some research. For example, Molina-Cevallos,13 who, in a qualitative study that aimed to identify the barriers and opportunities for vasectomy in 34 couples who attended the Hospital Gineco Obstétrico Isidro Ayora in Quito (Ecuador) in 2019, found that machismo is a determinant for the acceptance of vasectomy, especially because virility is culturally associated with the male reproductive organ and any intervention in this area reduces or causes the loss of sexual drive.
It is striking to note the importance given by the participants in the present study to the opinion of friends and family members when making the decision to undergo vasectomy, even among those with the highest level of knowledge (41.36%). Therefore, it is necessary to devise strategies to promote this procedure involving family members, also considering that other studies have already described this pattern of influence and the support of other people.12,14,15
When analyzing data by origin of the participants in this study, it was found that the level of knowledge was better in students from Mexico and Bolivia, where 77.31% and 68.28%, respectively, had a high level, while in Panama and Brazil the performance was lower, with only 51.13% and 3.33%, respectively, having a high level. To date, there is no further research available that presents the distribution of the level of knowledge about vasectomy in medical students by country that would allow comparing these results; however, contrary to expectations, it may be established that the countries in which the highest level of knowledge was reported do not rank first in studies that describe the rates of utilization of the procedure. In a study conducted by the United Nations16 in 2015 on the use of this procedure among married or cohabiting couples, it was found that Brazil had the highest prevalence (5%), followed by Mexico (2.2%), Panama (0.5%), and Bolivia (0.1%).
It is encouraging that in both the present study and that of Torrado-Arias et al.,8 most participants (94.02% and 96.4%, respectively) stated that they would recommend vasectomy. This is especially noteworthy because this differs from the findings of GamalEl Din & Saleh,17 who in a study of 350 unmarried final-year medical students at Cairo University found that 92.4% (n=145) of the men refused the idea of vasectomy as a contraceptive method and would not recommend it to their friends; this marked difference can be explained by the strong religious influence in Egypt.
The trend of acceptance of vasectomy found in the present study also differs significantly from the statistics shown by research conducted with medical personnel, such as the study by Ebeigbe et al.14 in Nigerian gynecology residents, where despite having a good level of knowledge about the procedure, only 5.8% recommended it to their patients. That same study established that 58.6% of respondents would not undergo vasectomy (21.3% for sociocultural reasons, 13.1% for religious reasons, 41% for psychological reasons, and 24.6% for nonspecific reasons),14 while in the present study only 10.8% indicated that they would not undergo this procedure.
Finally, it could be established that medical students in Latin America have a good knowledge of vasectomy, although there are theoretical gaps, especially regarding the cost of the procedure and the type of anesthesia used, aspects that can make a difference in patient decision making.
As noted, the highest proportion of male and female participants who would not recommend vasectomy, and of men who would not undergo vasectomy, are students with low and medium levels of knowledge, respectively. This demonstrates that education can break down the sociocultural barriers that exist around the procedure and, therefore, support the development of medical education programs that ensure the training of health professionals to provide quality vasectomy counseling, which has been shown to significantly expand access to modern contraception in low-income countries12 and promote the elimination of negative attitudes and practices of health care providers that can influence patient decision-making.
The main strengths of the present study are that it is the first research that evaluates variables of knowledge and perception about vasectomy in Latin American medical students, that it shows the level of knowledge of participants from different backgrounds, and that it used an instrument validated by specialists through a pilot test carried out in each of the countries with a sample of students that was different from those surveyed for the analysis of the data. On the other hand, the study population was not selected by randomized sampling, but by convenience sampling, and therefore selection biases could occur due to not having a representative sample from each country, thus limiting data extrapolation. There may also be an information bias since it is possible that the curricula of the medical programs of the students included differ from each other since they are offered by universities in different countries. Likewise, another limitation of this study is that it was not possible to determine the reasons for the variability in knowledge in each country.
Conclusions
The majority of participants have a good level of knowledge and acceptance, as well as a good perception of vasectomy, since they would recommend it. This is critical because in the future, as health professionals, they will play a key role in patient counseling and in the promotion of sexual and reproductive health.
However, although most participants have a good level of acceptance and would recommend vasectomy, a considerable percentage (30.17%) of the men surveyed would not undergo the procedure. Therefore, it is advisable to establish and analyze the factors that could influence this decision and to implement more training strategies to promote the use of vasectomy as a family planning alternative.
Lastly, it is necessary to develop strategies and projects in the region to inform and train not only medical students but also the general population on this topic, in order to overcome the negative perceptions and erroneous knowledge around this procedure, which would greatly contribute to consider vasectomy as a reliable and safe alternative for family planning.