Introduction
The COVID-19 pandemic is a major public health concern for both developed and developing countries, but its impact varies depending on the response capacity of each health system.
The first case of SARS-CoV-2 virus in Latin America was reported in February 2020. Since then, the virus has generated a high burden of incidence, case fatality, and mortality rates1 due to the deep socioeconomic inequalities, inadequate health infrastructure, and fragile health systems in the region.2 Consequently, by the end of 2020, Latin America had become the epicenter of the pandemic, accounting for more than half of all COVID-19 cases and deaths reported worldwide.3 Peru has been no stranger to this problem, and in order to address it, institutions have joined scientific research efforts by conducting studies ranging from clinical-epidemiological,4 genomic5 and prognostic characterization5 of the disease6 to research reporting on the efficacy of interventions for its management.7
By February 2021, COVID-19 had caused almost 1 500 000 infections and nearly 130 000 deaths in Peru, cases that were identified by molecular, antigen, or serological antibody testing.8 At that moment, there was already a great deal of information about the disease and its prognostic factors in hospital settings;9 however, little was known about environmental risk factors such as altitude.
In a study of 159 inhabitants of La Rinconada (the highest city in the world, located in southeastern Peru at 5 100-5 300 m.a.s.l.), Champignuelle et al.10 ruled out the existence of a protective effect of altitude against COVID-19; however, because the study was conducted in the early months of the pandemic and the sample size was very small, it was not possible to generalize this finding. In contrast, Accinelli & Leon11 suggested, based on national data from Peru, that the number of COVID-19 cases and deaths per 100 000 inhabitants decreases as altitude increases. Similarly, in a study that included data from 185 Peruvian provincial capitals with altitudes ranging from 3 to 4 342 m.a.s.l, Segovia et al.12 confirmed that the incidence of COVID-19 infection decreases at high altitudes, although they denied a correlation between altitude and case fatality rate. These somewhat contradictory findings warrant further research to elucidate the correlation between altitude and COVID-19 incidence.
Peru has different altitude levels, which can differ by department or province, so extrapolating findings from previous studies to the ecological level of a district is challenging. Several studies report a correlation between altitude and the number of cases and deaths from COVID-19,11-13which could be explained by environmental factors such as lower atmospheric pressure, low temperatures, and relative air humidity.14 It has even been proposed that there is a lower expression of angiotensin-converting enzyme 2 receptors in inhabitants of populations located at high altitudes, and this enzyme is the receptor that SARS-CoV-2 uses to enter cells.15
Although all these factors suggest that that there may be a correlation between altitude and COVID-19 frequency, the nature of this correlation might differ depending on the frequency measure used. For example, although mortality and case fatality rate are both ratios that measure deaths from COVID-19, in this case, they serve different purposes: the former assesses the number of deaths in a population, while the latter measures the severity of the disease. Similarly, incidence has a different purpose, as it measures the speed at which the disease spreads in the population. Furthermore, the analysis of the correlation between altitude and frequency of COVID-19 should take into account demographic indicators such as population density and poverty, as these factors could influence the dynamics of transmission and deaths, considering that there is an unequal distribution of wealth and excessive centralism in Peru, which creates heterogeneous population densities.
In view of the above, the objective of the present study was to determine the correlation between altitude and incidence, case fatality, and mortality rates due to COVID-19 in Peru.
Materials and methods
Study type
Multiple-group ecological study. The unit of analysis was the district, which is the smallest geographical subdivision of Peru for political and administrative purposes.16
Data used
In Peru, at the time of data collection, there were reports on the number of positive cases and deaths due to COVID-19 from 1 874 districts (distributed across 24 departments) and one constitutional province (El Callao). The data used in the study was gathered from official reports issued from March 2020, when the pandemic began, to February 2021, when the national vaccination campaign against COVID-19 was launched.
Public data retrieved from government sources available on the web was subjected to secondary analysis. Thus, the number of deaths and positive cases of COVID-19 was obtained from the Plataforma Nacional de Datos Abiertos (National Open Data Platform) (available at: https://www.datosabiertos.gob.pe/),17 and information on altitude (m.a.s.l.), surface area (km2), and poverty (%) of each district was obtained from reports of the Centro Nacional de Planeamiento Estratégico (National Center for Strategic Planning).18
It should be noted that poverty was considered monetary poverty when the per capita expenditure was insufficient to purchase basic consumer basket items and other basic goods (housing, education, health, etc.). It is important to bear in mind that the per capita cost of the consumer basket in 2020 was approximately 97 dollars per month.19 Information on the number of inhabitants in each district was obtained from reports of the Instituto Nacional de Estadística e Informática (National Institute of Statistics and Informatics).20
Procedures
The variable altitude was categorized into low (0-999 m.a.s.l.), medium (1 000-2 499 m.a.s.l.) and high (≥2 500 m.a.s.l.) following the categorization used by Castagnetto et al.21 in their study. Since there were many proposals for altitude classification, this categorization was chosen because it was previously employed in a study on COVID-19 transmission dynamics based on a biological-adaptive criterion.
Cumulative incidence, case fatality, and mortality rates were calculated as follows: cumulative incidence rate as the number of positive COVID-19 cases among the total population of each district multiplied by 10 000; case fatality rate was the number of deaths due to COVID-19 among the number of positive cases in each district multiplied by 100; and mortality rate was the number of deaths due to COVID-19 among the total population of each district multiplied by 100 000. These calculations were performed according to the guidelines of the Peruvian Ministry of Health for epidemiological surveillance of the new SARS-CoV-2 coronavirus.22
The general database was structured in Microsoft Excel, where the district count of positive cases and deaths by COVID-19 was performed. Disaggregated databases were joined using a unique geographic location code (UBIGEO) for each district. Only districts with case and mortality frequency (identified by molecular, antigen, or serological antibody testing) greater than 0 were included in the analysis. Therefore, the estimation of cumulative incidence, case fatality, and mortality rates for COVID-19 was made based on the analysis of 1 823, 1 526, and 1 595 valid districts, respectively. COVID-19 cases and deaths reported as such only based on clinical (signs and symptoms) and/or epidemiological (positive COVID-19 contact) criteria were excluded from the count. The unified database was exported to the IBM SPSS V. 26 software, where the corresponding statistical analyses were performed.
Data analysis
The normality of the data on altitude and COVID-19 incidence, case fatality, and mortality rates by district was evaluated using the Kolmogorov-Smirvov test, considering a significance level of p<0.05. An exploratory analysis was also performed using a bivariate scatter plot and Spearman's correlation coefficient (Rho). Then, the Kruskall-Wallis test was used to compare the medians of incidence, case fatality, and mortality rates according to altitude level, with a confidence index of 95%.
Finally, three multiple linear regression models were constructed, with the outcome variable for each model being incidence rate, case fatality rate, or mortality rate by COVID-19. To do this, a logarithmic transformation of these variables was performed, and the assumptions of normality, autocorrelation (Durbin-Watson: ≈2.0), and no multicol-linearity (variance inflation factor <10) were verified.
Ethical considerations
The present study did not require approval by an ethics committee because publicly available data provided by the Peruvian government during the COVID-19 health emergency were used. Furthermore, the data analyzed did not allow the identification of any individual, so the bioethical principle of confidentiality was not violated.
Results
The cumulative incidence rate for COVID-19 (1 823 valid districts) was 114.70 cases per 10 000 inhabitants (interquartile range [IQR]: 54.34-223.51). The COVID-19 case fatality rate (1 526 valid districts) was 9.78 deaths per 100 reported positive cases (IQR: 5.26-16.65). Finally, the COVID-19 mortality rate (1 595 valid districts) was 118.80 deaths per 100 000 inhabitants (IQR: 61.06-232.56).
Cumulative incidence rate (p<0.001) and case fatality rate (p=0.041) varied significantly depending on altitude according to the established categories: the former was higher in low altitude districts (218.59 cases per 10 000 inhabitants) and lower in high altitude districts (83.55 cases per 10 000 inhabitants) (p=0.000), while the later was lower in low altitude districts (9.31 deaths per 100 positive cases reported) and higher in high altitude districts (10 deaths per 100 positive cases) (p=0.038). As for mortality rate, although there was a significant difference depending on altitude (p<0.001), such variation was heterogeneous, being similar between low and medium altitude (96.03 and 89.84 deaths per 100 000 inhabitants, respectively) and higher at a high altitude (135.50 deaths per 100 000 inhabitants) compared with lower altitude levels (p<0.001) (Table 1).
Table 1 Cumulative incidence rate, case fatality rate, and mortality rate of COVID-19 depending on altitude levels in Peru. 2020-2021.
| COVID-19 frequency measurements | Altitude level (Me [IQR]) | p-value | ||
|---|---|---|---|---|
| Low altitude | Medium altitude | High altitude | ||
| Cumulative incidence rate (n=1 823) | 218.59 (130.48-329.98) | 94.82 (49.70-206.68) | 83.55 (41.85-154.61) | <0.001 * |
| Case fatality rate (n=1 526) | 9.31 (4.54-15.45) | 9.52 (4.94-16.66) | 10.00 (5.58-16.66) | 0.041 * |
| Mortality rate (n=1 595) | 96.03 (46.53-214.18) | 89.84 (52.50-193.96) | 135.50 (71.65-253.16) | <0.001 * |
Me: median: IQR: interquartile range.
* Kruskal-Wallis test // Difference in cumulative incidence rate between low altitude and medium altitude (p=0.000) and between low altitude and high altitude (p=0.000) // Difference in case fatality rate between low altitude and high altitude (p=0.038) // Difference in mortality rate between medium altitude and high altitude (p<0.001) and between low altitude and high altitude (p<0.001).
Source: Own elaboration.
A significant inverse correlation was found between the cumulative incidence rate of COVID-19 and altitude in the 1 823 valid districts (Rho Spearman: -0.355; p<0.001), being this correlation weak (Figure 1).
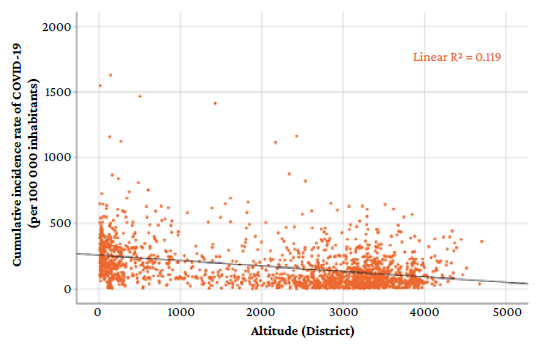
Source: Own elaboration.
Figure 1 Cumulative incidence rate of COVID-19 according to altitude in 1 823 districts of Peru. 2020-2021.
Likewise, a significant direct correlation was observed between COVID-19 case fatality rate and altitude in the 1 526 valid districts (Rho Spearman: 0.131; p<0.001), being this correlation very weak (Figure 2).
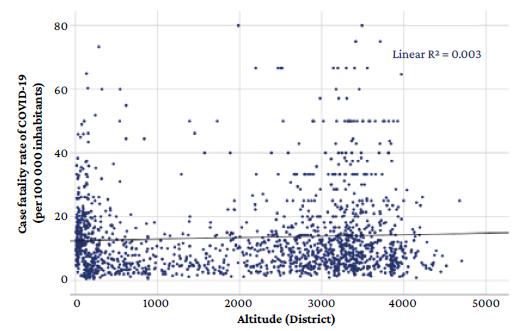
Source: Own elaboration.
Figure 2 Case fatality rate of COVID-19 according to altitude in 1 526 districts of Peru. 2020-2021.
In addition, a significant inverse correlation was found between COVID-19 mortality and altitude in the 1 595 valid districts (Rho Spearman: -0.310; p<0.001), being this correlation weak (Figure 3).
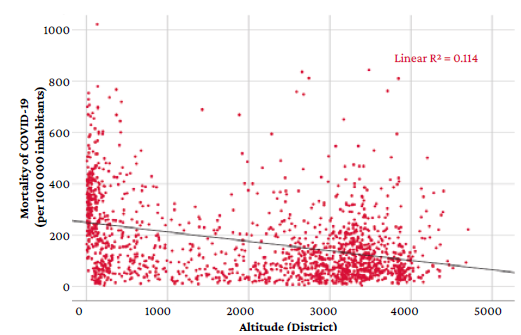
Source: Own elaboration.
Figure 3 Mortality by COVID-19 according to altitude in 1595 districts of Peru. 2020-2021.
In the multivariate analysis, altitude was significantly associated with the cumulative incidence rate (p<0.001) and the case fatality rate (p=0.009) of COVID-19. However, the association between altitude and mortality rate was not significant (p=0.179), even after adjusting for poverty and population density, variables that in all three models were significantly associated with mortality rate (p<0.05). In this sense, poverty showed an inverse correlation with the three ratios in the three models, while population density showed a direct correlation with the three ratios in the three models (Table 2).
Table 2 Multivariate analysis: altitude and incidence, case fatality, and mortality rates of COVID-19 in Peru. 2020-2021.
| Variables | Cumulative incidence rate of COVID-19* | Case fatality rate of COVID-19t | Mortality rate of COVID-19 * | |||
|---|---|---|---|---|---|---|
| ß ** | Valor p | ß ** | Valor p | ß ** | Valor p | |
| Altitude | -0.175 | <0.001 | 0.111 | <0.001 | -1.346 | 0.179 |
| Poverty (%) | -0.461 | <0.001 | -0.115 | <0.001 | -28.872 | <0.001 |
| Population density | 0.048 | 0.016 | 0.052 | 0.049 | 5.191 | <0.001 |
* R2 of the model: 0.324; p=0.000; Akaike information criterion: 1608.9.
† R2 of the model: 0.018; p=0.000; Akaike information criterion: 1342.8.
‡ R2 of the model: 0.431; p=0.000; Akaike information criterion: 748.1.
** Standardized regression coefficient.
Source: Own elaboration.
Discussion
Several scientific evidence support the correlation between altitude and COVID-19 epidemiology, one of them being the lower susceptibility to hypoxic effects in people living at high altitudes (>2 500 m.a.s.l) as a result of acclimatization and physiological adaptation.15,23This is consistent with the significant inverse correlation between altitude and COVID-19 incidence rate observed in the present study (rho: 0.355; p<0.001), which indicates a reduction of positive cases at higher altitudes.
This result agrees with the findings of a study conducted by Segovia-Juarez et al,12 who analyzed official data reported as of June 13, 2020, from 185 provincial capitals in Peru with altitudes between 3 and 4 342 m.a.s.l. (225 132 positive COVID-19 cases), finding that the number of COVID-19 cases is lower in provinces at a higher altitude (R2 =0.42; p<0.001). In this sense, the decrease in the cumulative incidence of COVID-19 as altitude increases could be explained by the adaptive physiology of individuals; however, it is important to consider the possibility of a spurious correlation when inferring an individual correlation from group information (ecological fallacy).
Despite the limitations of its design, the findings of the present study corroborate those of previous national studies at a more specific ecological level11,12since a multilevel model, according to altitude by clustered districts, was not used because adequate variance at the altitude level could not be guaranteed. Therefore, it is recommended that hierarchical models be used in subsequent research to control ecological fallacy.
The cumulative incidence rate of COVID -19 in the present study varied depending on altitude, with a reduction from 218.5 to 83.5 positive cases per 100 000 inhabitants in low-and high-altitude districts, respectively. This inverse correlation was significant even after adjusting for poverty and population density (ß=-0.171; p<0.001). This is consistent with the findings of Seclén et al.,24 who conducted an analytical study with official COVID -19 data recorded from March to July 2020 in 25 regions of Peru and secondary data from the latest Encuesta Nacional de Demografíay Salud del Perú (ENDES 2018 - Peruvian National Demographic and Health Survey), in which they found a sex- and age-adjusted inverse correlation between altitude and cumulative incidence (Rho: -0.8; p<0.000). Their study also showed a higher incidence in coastal regions and a lower incidence as altitude increased.
Likewise, a study by Cano-Pérez et al.,25 carried out using official data on COVID-19 recorded until August 1, 2020, in 70 municipalities and cities of the 32 departments of Colombia (altitude range from 1 to 3 180 m.a.s.l.), found a negative correlation between altitude and incidence of positive cases (rho: -0.315; p<0.01. This means that the frequency of COVID-19 cases was higher in municipalities at low altitudes and lower in those located in areas of higher altitude.
In the study by Fernandes et al.,26 conducted in Brazil between May and July 2020 in 154 cities with altitudes between 5 and 1 135 m.a.s.l., a negative correlation between COVID-19 incidence and altitude was also found (r=-0.38; p<0.01). This is further strengthened by the research of Arias-Reyes et al)13 who, after analyzing data from 23 countries in the Americas reported up to May 23, 2020, found that the rate of coronavirus transmission is lower in populations located above 1 000 m.a.s.l. In this sense, scientific evidence in general suggests that altitude and the incidence of COVID-19 are inversely correlated,27 which may be explained by the climatological factors that characterize altitude, such as lower atmospheric pressure, low temperatures, better air quality, lower relative humidity, etc.14
Prolonged exposure to high altitude and, consequently, to lower atmospheric oxygen pressure leads to adaptive responses at the population level that imply less susceptibility to develop severe adverse hypoxic effects in acute COVID-19 infections,15,23which translates into less symptom expression, fewer reported cases, and low incidence. It should be noted that in many high-altitude areas of Peru, molecular tests for COVID-19 detection were not available at the beginning of the pandemic, which could lead to a bias in the estimation of incidence.28
In the present study, the case fatality rate of COVID-19 was directly correlated to altitude (Rho: 0.131; p<0.001) because there was an increase in deaths, reaching 10 deaths per 100 positive cases in high altitude districts. This direct correlation was maintained in the multivariate model, even after adjusting it for poverty and population density. In contrast, according to the results by Segovia-Juarez et al.12 , there is no correlation between altitude and COVID-19 case fatality rate (R2 :-0.0081, p=0.815), which could be due to the fact that their study was conducted at the beginning of the pandemic with official data recorded as of June 13, 2020, only three months after the first case was reported in the country and when the virus had spread very little.
Consequently, the present research sought to complement the findings of Segovia-Juarez et al12 and Castagnetto et al,21 who reported that altitude does not affect the case fatality rate of COVID -19 in Peru. The present study attempted to overcome the limitations of those studies by analyzing a larger number of cases after excluding the probable effect of immunity from COVID-19 vaccination, which was initiated in the country in February 2021, at a specific ecological level, namely the districts.
Since case fatality rate refers to the proportion of fatal cases over the total number of infected cases, it is considered a measure of disease severity from a population perspective.22 It is likely that the adaptive mechanisms to hypobaric hypoxia are overwhelmed by the severity of the disease, which could have led to deaths. Furthermore, case fatality rate does not depend on indicators of poverty or population density, as demonstrated in the present study, but the cause of the deaths could be related to the host response to the infection and its ability to cope with it.
Finally, according to the results of the bivariate analysis, the COVID-19 mortality rate was inversely correlated with altitude (Rho: -0.310;p<0.001). However, this trend was not permanent as altitude decreased from low to medium and increased from medium to high; that is, multiple linear regressions failed to corroborate the inverse correlation initially observed when adjusting for poverty and population density.
Probably, the present study failed to linearly adjust the overall trend of the data and, therefore, the correlation between altitude and COVID-19 mortality rate could not be demonstrated. This conjecture gains strength when taking into account the findings of Castagneto et al,21 who analyzed 1 636 districts in Peru with 535 946 positive cases of COVID-19 registered between March 6 and August 15, 2020, in which there is a correlation between mortality and altitude that is only valid for altitudes <1 000 m.a.s.l, ruling out any correlation above this altitude. In other words, there is no overall linear correlation between altitude and COVID-19 mortality that encompasses all altitude levels, but it only applies to certain altitude ranges.
The latter statement is supported by Woolcott & Bergman,29 who in a study using data recorded from January 20 to April 13, 2020, in 1 016 counties in the United States and from January 8 to May 13, 2020, in 567 municipalities in Mexico found that the risk of death among Mexican men was 31% higher at >2 000 m.a.s.l. versus that at <1 500 m.a.s.l. (incidence rate ratio (IRR): 1.31, 95%CI: 1.03-1.66; p=0.025). Woolcott & Bergman29 also pointed out that the risk of death of Mexican men under 65 years of age living at altitudes >2 000 m.a.s.l. is 36% higher than that of those living at altitudes <1 500 m.a.s.l. (IRR: 1.36, 95%CI: 1.05-1.78; £=0.022). In other words, not only is there no overall altitude-mortality correlation, but mortality would be influenced by other variables. This finding differs from that reported by Seclén et al.,24 who conducted a study in Peru and reported lower COVID-19 mortality rates with increasing altitude.
The findings of the present study also differ from those of Campos et al.,30 who conducted an ecological investigation in Ecuador in which they included COVID -19 data recorded between February and August 2020 in 23 provinces located at altitudes ranging from sea level to more than 3 000 m.a.s.l., finding an inverse correlation between COVID-19 mortality and altitude (- 0.45; p=0.03). However, it should be noted that the authors concluded that further research is needed to understand why altitude may have a protective effect against mortality due to COVID-19 and how this can be applied in a clinical setting.
Research in this regard has also been carried out in countries with lower altitude levels. For example, Cunha et al.26 conducted a study in 154 Brazilian cities located at altitudes between 5 and 1 135 m.a.s.l., and also reported an inverse correlation between mortality of COVID-19 and altitude (r=-0.43; p<0.01). However, this only applies to the correlation observed in the present study in the bivariate analysis since Cunha et al.26 did not perform a multivariate analysis.
The heterogeneity of this finding and the inconsistent support it receives from previous studies highlight the possibility of certain biases related to the adequate notification of cases in high-altitude areas due to the lack of suitable electronic systems. This is compounded by the shortage of serological detection methods due to the lack of distribution in high-altitude areas with lower accessibility, resulting in an underestimation of cases. If the centralization of COVID-1928 diagnostic tests at the expense of a lower supply in high altitude areas is added to all the above, it is possible to understand why there was a correlation between altitude and mortality. The inverse correlation found between poverty and mortality is noteworthy, but it is not logical, as a direct correlation is expected. In other words, it is not biologically plausible, and this can again be explained by the limitations mentioned earlier.
The main limitation of ecological studies is that they do not have information on exposure (altitude) and outcome (COVID-19 frequency) at the individual level, so the existence of a correlation resulting from aggregate (district) data does not necessarily apply at the individual level.31 Putting aside individual pathophysiological hypotheses related to COVID-19,32 it is worth considering some environmental factors, such as temperature, humidity, air speed and precipitation, and climatological factors that, according to some studies, may have an impact on the dynamics of transmission and deaths due to COVID-19.14,33Although these factors were not taken into account in the present study, they are closely linked to the ecological diversity of climates and altitude levels that characterize the megadiversity of Peru. Consequently, it is suggested that an adjustment analysis be performed in subsequent research, and that the effects of vaccination, social distancing and other measures taken to prevent the spread of virus transmission be studied.
Conclusions
An inverse correlation was observed between altitude and COVID-19 incidence rate, i.e., incidence decreased at higher altitudes, which is supported by the literature. On the other hand, a direct correlation was found between altitude and COVID-19 case fatality rate, that is, the case fatality rate is higher as altitude increases, a finding that is partially supported by previous publications and requires further study. Finally, altitude was not correlated with COVID-19 mortality rate.















