Introduction
Acute appendicitis is an inflammatory disease of the appendix that represents a major health burden, with a worldwide incidence estimated at 86 cases per 100 000 person-years.1 This condition is the leading cause of abdominal surgical emergencies in the pediatric population. In addition, it is estimated that between 30% and 75% of cases in children progress to perforated appendicitis, mainly in children under 5 years of age.2 In spite of the availability of new technological tools, diagnosing acute appendicitis in the pediatric population before perforation occurs remains a challenge because the typical symptoms and signs of this disease are not always evident, children do not always report symptoms clearly, and physical examination findings are similar to those observed in other differential diagnoses.3 Accordingly, a diagnostic error rate ranging from 28% to 57% in patients under 12 years of age and almost 100% in patients under 2 years of age has been described.2
Detecting perforated appendicitis is paramount not only because it allows establishing a treatment strategy and predicting postoperative outcomes, but also because this condition increases the rate of complications, going from 8% in patients with non-perforated appendicitis to 39% in patients with perforated appendicitis.3 These complications include ileus, sepsis, intra-abdominal abscesses and surgical wound infection, and their occurrence leads to increased length of hospital stay and increased use of resources.4
Previous studies, such as the one conducted by Bonadio et al.5 in Brooklyn, USA, with 180 children under 5 years of age hospitalized for appendicitis, have aimed to determine the predictive value of the date of symptom onset, the type of symptoms and signs, and the results of laboratory (complete blood count) and imaging tests during hospitalization for determining the risk of perforated appendicitis. It has been found that the younger the patient and the longer the time of progression, the more likely it is that this outcome will occur.
At present, most of the studies performed to detect predictive factors for perforated appendicitis are retrospective, and there are not many studies involving children. Therefore, the objective of the present study was to identify predictive factors for perforated appendicitis in a pediatric population (<18 years of age) at the time of admission to the emergency department.
Materials and methods
Study design and type
Prospective longitudinal cohort study conducted at the Fundación Hospital Pediátrico La Misericordia (HOMI), a quaternary care institution in Bogotá D.C., Colombia, which primarily treats children from low socioeconomic levels (strata 1, 2, and 3). This research is derived from a postgraduate thesis.6
Study population and sample
The study population comprised all pediatric patients (<18 years old) admitted to the emergency department of the Fundación HOMI or referred to that hospital for acute appendicitis, who underwent emergency appendectomy between November 1 and December 31, 2013 (N=208).
Sample size was calculated based on the 2012 prevalence of perforated appendicitis in the institution, which was 40%. An expected relative risk of 0.38 was estimated with a confidence level of 95%, thus obtaining a sample size of 58 patients for each cohort (perforated appendicitis and non-perforated appendicitis). Fifteen patients were excluded for the following reasons: diagnosis of appendiceal phlegmon without surgical intervention (n=3), intraoperative rupture of the appendix (n=3), and failure to confirm the diagnosis of appendicitis in the histopathology study (n=9) because of poor concordance between surgeons and pathologists.7 Consequently, a final sample of 193 children (98 with perforated appendicitis and 95 with non-perforated appendicitis) was obtained.
Procedures and study variables
A perforated appendix was defined as the presence of a macroscopic hole in the appendix or the presence of fecalith in the abdominal cavity.8,9Independent variables included sociodemographic variables; whether or not the patient was referred to the institution; the duration (in days) of symptoms until surgery; the medical personnel who first assessed the patient; the presence of nausea, emesis, anorexia, diarrhea, dysuria, and subjective fever when questioning on admission to the emergency department; anthropometric status; the presence of tachycardia, temperature >38.3°C, abdominal pain, localized pain, and dehydration on physical examination; a left shift in the complete blood count (determined based on the limits for each age reported by the institutional laboratory); and a pathology report of perforated appendix.
With respect to sociodemographic variables, socioeconomic level was taken into account, which in Colombia is divided into 6 strata depending on the place of residence (strata 1 and 2 refer to households with lower incomes; strata 3 and 4 correspond to households with middle incomes; and strata 5 and 6 relate to households with high incomes).10 The health system regime in which the patients were enrolled was also considered, which in the country is divided into contributory and subsidized. In 2014, 97% of the population was insured, with 47% belonging to the contributory regime; it should be noted that people with higher incomes and, therefore, better access to the health system, are enrolled in the contributory regime.11
Statistical analysis
Data were analyzed using STATA version 15.1. For descriptive analysis, means and standard deviations were calculated for quantitative variables, and relative and absolute frequencies for categorical variables. The distribution of the numerical variables was also verified using Kernel density estimate plots and the Shapiro-Wilk and Kolmogorov-Smirnov tests.
Bivariate analysis of quantitative variables was performed using the Student's t-test or Mann-Whitney U test, depending on the distribution of the data. In the bivariate analysis of the categorical variables, contingency tables were used to calculate odds ratios (OR) with their respective 95% confidence intervals (95%CI) and to perform the chi-square test or Fisher's exact test according to compliance with the statistical assumptions, with a statistical significance level of p<0.05.
As for the multivariate analysis, the variables with statistical significance in the bivariate analysis and those with clinical relevance were included in a logistic regression model to establish the association between them and the presence of perforated appendicitis. A diagnosis of the regression model was performed to determine the influential values and collinearity of the variables. Subsequently, using the stepwise regression method (backward elimination and forward selection), the variables were selected according to their statistical significance, and regression analyses were performed for each of them.
The resulting models were evaluated for goodness of fit to select the model that best explained the association between the variables and the risk of perforated appendix, which was measured calculating the ORs and their respective 95%CI. The explanatory power of the models was verified by calculating the areas under the receiver operating characteristic curve (AUC-ROC) since, as the dependent variable is a dichotomous variable, these areas allow evaluating its diagnostic performance in a manner similar to a diagnostic test.
Ethical considerations
The study protocol was approved by the Ethics and Research Committee of the Fundación HOMI as per Minutes CEI 281-20 of 2014. Furthermore, the ethical principles for research involving human subjects established in the Declaration of Helsinki12 and the provisions on health research in Resolution 8430 of 1993 of the Colombian Ministry of Health were taken into account.13
Results
The mean age of the participants was 9.8 years (SD=3.55), 55.96% were male, 76.68% were referred from other institutions, 87.05% were from Bogotá D.C., and 50.78% had perforated appendicitis at the time of surgery. The percentage of patients with a perforated appendix was lower as the socioeconomic stratum of the patients increased, being 59.46% in stratum 1 and 45.76% in stratum 3. Perforated appendicitis was more frequent in children enrolled in the subsidized regime (61.11%) compared to those in the contributory regime (48.41%). The sociodemographic characteristics per patient group are described in Table 1.
In the bivariate analysis, the following variables were significantly associated with the risk of presenting perforated appendicitis: presence of emesis (OR=3.60, 95%CI: 1.44-9.80), diarrhea (OR=2.23, 95%CI: 1.13-4. 43) and subjective fever (OR=2.11, 95%CI: 1.07-4.17) during questioning on admission to the emergency department, and presence of tachycardia (OR=2.68, 95%CI: 1.41-5.12) and temperature >38.3°C (OR=3.53, 95%CI: 1.42-9.58) on physical examination. Moreover, a significant difference was found in the duration of symptoms until surgery between groups (OR=1.77, 95%CI: 1.28-2.47), and it was observed that the presence of localized abdominal pain on physical examination was associated with a lower risk of perforated appendix (OR=0.23, 95%CI:0.08-0.60) (Table 1).
Table 1 Bivariate analysis and unadjusted risk ratios.
| Variable | Total | Perforated appendicitis | OR | 95%CI | p-value | ||
|---|---|---|---|---|---|---|---|
| n=193 | Yes (98) | No (95) | |||||
| Age in years, mean (SD) | 9.86 (3.55) | 9.60 (3.74) | 10.13 (3.34) | 0.96 | 0.88-1.04 | 0.305 | |
| Duration of symptoms until surgery, median (IQR) | 1.71 (1.17) | 2.12 (1.54) | 1.54 (0.88) | 1.77 | 1.28-2.47 | 0.001 | |
| Sex, n (%) | Male | 108 (55.96) | 54 (55.10) | 54 (56.84) | 0.93 | 0.51-1.71 | 0.808 |
| Female | 85 (44.04) | 44 (44.90) | 41 (43.16) | ||||
| Regimen, n (%) | Contributive | 157 (81.35) | 76 (77.55) | 81 (85.26) | 0.60 | 0.26-1.32 | 0.169 |
| Subsidized | 36 (18.65) | 22 (22.45) | 14 (14.74) | ||||
| From Bogotá, n (%) | Yes | 168 (87.05) | 86 (87.76) | 82 (86.32) | 1.14 | 0.45-2.90 | 0.766 |
| No | 25 (12.95) | 12 (12.24) | 13 (13.68) | ||||
| Referred to the institution, n (%) | Yes | 148 (76.68) | 72 (73.47) | 76 (80.00) | 0.69 | 0.33-1.43 | 0.283 |
| No | 45 (23.32) | 26 (26.53) | 19 (20.00) | ||||
| Stratum, n (%) | 1 | 37 (19.17) | 22 (22.45) | 15 (15.79) | --- | --- | --- |
| 2 | 97 (50.26) | 49 (50.00) | 48 (50.53) | 0.70 | 0.30-1.60 | 0.354 | |
| 3 | 59 (30.57) | 27 (27.55) | 32 (33.68) | 0.57 | 0.23-1.43 | 0.191 | |
| Localized pain, n (%) | Yes | 161 (83.42) | 73 (74.49) | 88 (92.63) | 0.23 | 0.08-0.60 | <0.001 |
| No | 32 (16.58) | 25 (25.51) | 7 (7.37) | ||||
| Emesis, n (%) | Yes | 162 (83.94) | 90 (91.84) | 72 (75.79) | 3.60 | 1.44-9.80 | 0.002 |
| No | 31 (16.06) | 8 (8.16) | 23 (24.21) | ||||
| Nausea, n (%) | Yes | 168 (87.05) | 86 (87.76) | 82 (86.32) | 1.14 | 0.45-2.90 | 0.766 |
| No | 25 (12.95) | 12 (12.24) | 13 (13.68) | ||||
| Anorexia, n (%) | Yes | 126(65.28) | 65 (66.33) | 61 (64.21) | 1.10 | 0.58-2.07 | 0.578 |
| No | 67 (34.72) | 33 (33.67) | 34 (35.79) | ||||
| Diarrhea, n (%) | Yes | 59 (30.57) | 38 (38.78) | 21 (22.11) | 2.23 | 1.13-4.43 | 0.120 |
| No | 134 (69.43) | 60 (61.22) | 74 (77.89) | ||||
| Dysuria, n (%) | Yes | 22 (11.40) | 11 (11.22) | 11 (11.58) | 0.97 | 0.36-2.60 | 0.938 |
| No | 171 (88.60) | 87 (88.78) | 84 (88.42) | ||||
| Subjective fever, n (%) | Yes | 135 (69.95) | 76 (77.55) | 59 (62.11) | 2.11 | 1.07-4.17 | 0.193 |
| No | 58 (30.05) | 22 (22.45) | 36 (37.89) | ||||
| Malnutrition, n (%) | Yes | 35 (18.23) | 15 (15.46) | 20 (21.05) | 0.68 | 0.30-1.53 | 0.316 |
| No | 157 (81.77) | 82 (84.54) | 75 (78.95) | ||||
| Obesity, n (%) | Yes | 7 (3.65) | 4 (4.12) | 3 (3.16) | 1.32 | 0.22-9.24 | 0.721 |
| No | 185 (96.35) | 93 (95.88) | 92 (96.84) | ||||
| Overweight, n (%) | Yes | 33 (17.19) | 18 (18.56) | 15 (15.79) | 1.21 | 0.53-2.79 | 0.611 |
| No | 159 (82.81) | 97 (81.44) | 80 (84.21) | ||||
| Normal anthropometric status, n (%) | Yes | 75 (39.06) | 60 (81.86) | 57 (60.00) | 1.08 | 0.58-2.01 | 0.792 |
| No | 117 (60.94) | 37 (38.14) | 38 (40.00) | ||||
| Temperature >38.5°C, n (%) | Yes | 32 (16.58) | 24 (24.49) | 8 (8.42) | 3.53 | 1.42-9.58 | 0.003 |
| No | 161 (83.42) | 74 (75.51) | 87 (91.58) | ||||
| Tachycardia, n (%) | Yes | 118 (61.14) | 71 (72.45) | 47 (49.47) | 2.68 | 1.42-5.12 | 0.001 |
| No | 75 (38.86) | 27 (27.55) | 48 (50.53) | ||||
| Dehydration, n (%) | Yes | 151 (78.24) | 82 (83.67) | 69 (72.63) | 1.93 | 0.91-4.18 | 0.063 |
| No | 42 (21.76) | 16 (16.33) | 26 (27.37) | ||||
| Signs of peritoneal irritation, n (%) | Yes | 117 (91.71) | 92 (93.88) | 85 (89.47) | 1.80 | 0.56-6.29 | 0.267 |
| No | 16 (8.29) | 6 (6.12) | 10 (10.53) | ||||
| Left shift, n (%) | Yes | 177 (97.79) | 88 (98.88) | 89 (96.74) | 2.97 | 0.23-157.43 | 0.328 |
| No | 4 (2.21) | 1 (1.12) | 3 (3.26) | ||||
Source: Own elaboration
Multivariate analysis showed a statistically significant association between the risk of perforated appendicitis and the presence of emesis in the questioning on admission to the emergency department (OR=2. 85, 95%CI: 1.04-7.78), tachycardia (OR=2.98, 95%CI: 1.39-6.38), temperature >38.3°C (OR=3.70, 95%CI: 1.33-10.30) on physical examination, and duration of symptoms until surgery (OR=1.85, 95%CI: 1.26-2.72) (Table 2).
Table 2 Multivariate analysis of the main model with adjusted estimators.
| Variable | OR | 95%CI | p-value | |
|---|---|---|---|---|
| Age | 1.00 | 0.90-1.11 | 0.946 | |
| Stratum (compared to stratum 1) | 2 | 0.90 | 0.36-2.26 | 0.824 |
| 3 | 0.72 | 0.26-2.00 | 0.533 | |
| Sex | 1.04 | 0.51-2.16 | 0.902 | |
| Localized abdominal pain | 0.41 | 0.15-1.16 | 0.094 | |
| Emesis | 2.85 | 1.04-7.78 | 0.041 | |
| Diarrhea | 1.68 | 0.79-3.57 | 0.180 | |
| Subjective fever | 0.93 | 0.41-2.09 | 0.862 | |
| Temperature >38.3°C | 3.70 | 1.33-10.30 | 0.012 | |
| Tachycardia | 2.98 | 1.39-6.38 | 0.005 | |
| Duration of symptoms until surgery | 1.85 | 1.26-2.72 | 0.002 | |
| Left shift | 2.96 | 0.21-41.99 | 0.423 | |
Source: Own elaboration.
Subsequently, stepwise regression (backward elimination and forward selection) confirmed the statistical significance of these four variables in the multivariate analysis, so a regression analysis was performed using them (Table 3).
Table 3 Final multivariate model with adjusted risk estimators.
| Variable | OR | 95%CI | p-value |
|---|---|---|---|
| Emesis | 4.28 | 1.63-11.21 | 0.003 |
| Tachycardia | 3.38 | 1.69-6.59 | 0.001 |
| Temperature >38.3°C | 3.36 | 1.29-8.70 | 0.013 |
| Duration of symptoms until surgery | 1.95 | 1.37-2.77 | <0.001 |
Source: Own elaboration.
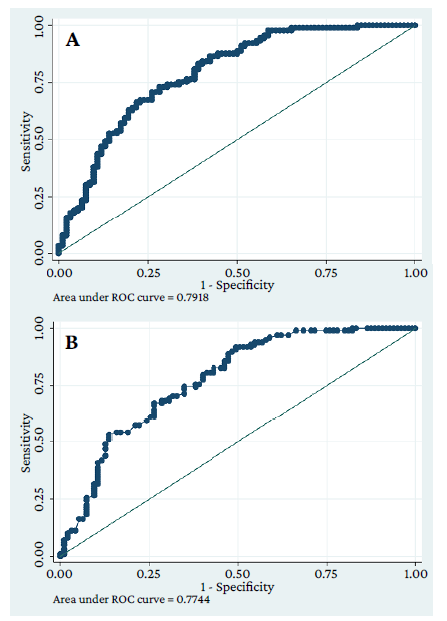
The estimation of the AUC-ROC showed a diagnostic performance of the final model with four variables: 0.7744, which is very similar to that of the original model: 0.7918 (Figure 1).
Discussion
The prevalence of perforated appendix in the present study was 50.78%. This value is higher than the one described by Papandria et al.14 in a cross-sectional study conducted in the United States with data from 683 590 patients (232 732 pediatric) with a diagnosis of hospitalization for acute appendicitis (perforated or non-perforated) registered in the Nationwide Inpatient Sample (NIS) and the Kids Inpatient Database (KID) between 1988 and 2008, finding that the prevalence of perforated appendicitis among children was 29.7%. Similarly, Zvizdic et al.,15 established in a retrospective observational cohort study conducted in Bosnia and Herzegovina with 295 pediatric patients with a confirmed diagnosis of acute appendicitis treated between 2013 and 2015 that perforated appendicitis occurred in 31.2% of participants. However, the findings of the present study are similar to the prevalence reported in studies conducted in lower-income countries. In 2007, Ngim et al.16 conducted a retrospective cross-sectional study in 118 children (<13 years) with a histological diagnosis of appendicitis who underwent appendectomy and found that 52% of them had perforated appendicitis.
Regarding sociodemographic factors, age was not significantly associated with the occurrence of perforated appendicitis, which differs from what has been reported in the literature, where an inversely proportional relationship with age has been demonstrated, with a higher risk of perforation in children under five years of age.5,17,18This could be explained because the hospital where the study was performed is a referral institution, where patients of all age ranges with advanced stages of appendicitis that usually progress to perforated appendix are treated, and this could have hindered the identification of this association in our sample.
Although there were no significant differences between the two groups of patients (perforated and non-perforated appendicitis) in terms of origin, socioeconomic level and health system regime, it was found that the frequency of perforation was higher in children from rural areas, of low socioeconomic level, and enrolled in the subsidized health system. This finding is consistent with what has been described in the literature, where it has been reported that patients living more than 50km from the treating hospital and in rural areas have a higher risk of perforated appendix, as well as those enrolled only in the public health system, living in low-income households, and living with adults with a low level of education.3,19,20
In the present study, a significant association was found between the duration of symptoms until surgery and the risk of perforation (OR=1.85, 95%CI: 1.26-2.72), which is in line with the literature describing the duration of symptoms as a risk factor for this outcome.4,5,16,21Moreover, increases in the risk of perforation have been described for every hour elapsed from the initial assessment until surgery. Bonadio et al.,22 in a retrospective case review of 248 children (<18 years) with uncomplicated CT-confirmed appendicitis between January 2010 and January 2014, found that the risk for developing perforation increased by 1.10 for each hour of time delay from ED admission to appendectomy in the operating room, and that the estimated ORs for developing perforation per in-hospital delay interval were 2.05 at 8 hours, 4.22 at 16 hours, and 8.67 at 24 hours. Also, Meltzer et al.,23 in a multicenter retrospective cohort study conducted in children (<18 years) hospitalized for appendicitis between January 1998 and July 2014, found that every hour increase in the time from ED triage to incision was independently associated with a 2% increase in the odds of perforation with an adjusted OR of 1.02. This finding stresses the need to make an early diagnosis of appendicitis to prevent perforation.
The presence of emesis in the questioning on admission to the emergency department was significantly associated with perforated appendix (OR=3.60, 95%CI: 1.44-9.80). At the time of writing this paper, this symptom had not been reported as associated with this outcome, since the symptoms usually described as risk factors for perforated appendicitis are subjective fever and anorexia,1,21,24,25which also differs from the findings presented here, since no association with these two variables was observed.
Similarly, the presence of tachycardia (OR=2.98, 95%CI: 1.39-6.38) and temperature >38.3°C (OR=3.7, 95%CI: 1.33-10.3) on physical examination were identified as factors that increase the risk of perforation. This is consistent with the findings reported in the literature, where fever measured in the ED has been described as an independent predictor of perforated appendicitis.15,21However, it should be noted that no association with tachycardia has been described.
Other factors associated with perforated appendix have also been described, such as rebound tenderness sensitivity, identified by Obinwa et al.1 in a retrospective review of pediatric appendectomies (0-14 years) performed on 1 037 patients between January 1995 and December 2008 at an institution in Ireland (OR=1.94, 95%CI: 1.23-3.04). Nevertheless, in the present study, localized abdominal pain was identified as a protective factor for perforated appendix (OR=0.23, 95%CI: 0.08-0.60), which could be explained by the fact that this type of pain can occur due to inflammation of the appendix before there is generalized inflammation of the peritoneum as a result of a perforation.26
It is worth pointing out that although the present study did not find significant differences in the left shift of the complete blood count between groups (perforated and non-perforated appendicitis), neutrophilia has been frequently reported in the literature as a risk factor for perforated appendicitis.16-25
In the multivariate analysis, it was found that the duration of symptoms until surgery (OR=1.95, 95%CI: 1.37-2.77) was a predictive factor for the development of perforated appendicitis, hence the importance of an early diagnosis. These findings are in line with the multivariate analysis of other studies where it has been established that this factor is one of the most frequently identified as a predictor of perforation.21,22,24,27-29
Concerning clinical variables, the only symptom associated with perforated appendicitis that remained significant in the multivariate analysis was the presence of emesis in the questioning on admission to the emergency department (OR=4.28, 95%CI: 1.63-11.21). Regarding clinical signs during physical examination, temperature >38.3°C and tachycardia also had a positive association with perforation, which is partly in line with what has been reported in the literature, where fever has been associated with an increased risk of this outcome in the pediatric population,4,24,27but no association with tachycardia has been described.
When combining the duration of symptoms until surgery and the presence of emesis in the questioning upon admission to the emergency room and tachycardia and temperature >38.3°C on physical examination, an AUC similar to that obtained with all the initial variables in the original model was observed. This demonstrates, by maintaining statistical significance, the importance of these four factors as predictors of perforated appendix. It should be noted that emesis and tachycardia as predictors of appendicitis have not been described in the reviewed literature, so they are proposed as new symptoms and signs to be considered during the examination of a pediatric patient with suspected perforated appendicitis.
One of the limitations of the present study is that, although it was a prospective cohort study with a calculated sample (which favors a high statistical quality regarding the findings), the results cannot be extrapolated to the entire population because the research was carried out in a referral hospital where most of the patients treated are from a low or middle socioeconomic level. Therefore, in order to validate these findings, a multicenter study with more recent information is suggested.
Conclusion
In the present study, the duration of symptoms and signs until surgery and the presence of emesis in the questioning on admission to the emergency department and tachycardia and fever (temperature >38.3°C) on physical examination were risk factors for acute perforated appendicitis in pediatric patients. Emesis and tachycardia are variables that were not found to be risk factors in the literature reviewed, so they are proposed as new factors to be considered to prevent this disease.