Introduction
Post-intubation tracheal laceration is a very rare complication, with a worldwide incidence of 1 case per 20 000 intubations,1 but it is associated with high mortality. The estimated incidence of tracheal laceration when performing intubation with a conventional endotracheal tube is 0.005%, and it increases to 0.05-0.19% in cases where a double-lumen tube is used.2 Mortality associated with iatrogenic tracheal laceration is high, reaching up to 42%,3 although underlying patient diseases are believed to be the cause of this high percentage of deaths.2
The suspected presence of post-intubation tracheal laceration based on the various signs and symptoms that may appear should be useful to undertake the appropriate diagnostic and therapeutic measures, but it should also be borne in mind that its management requires a multidisciplinary team to individualize the treatment in each case. In this sense, the joint work between the Anesthesiology and Resuscitation, Intensive Care Medicine, Thoracic Surgery, Interventional Pulmonology and Endoscopy services is the current recommendation to decide on the two possible therapeutic options for this complication: surgical treatment or conservative approach.4
Despite the increasingly widespread use of videolaryngoscopes, there is currently no validated and accepted classification that assesses intubation with these devices. Therefore, scales such as the Cormack-Lehane and Fremantle scales, or the POGO test (percentage of glottic opening) are used, but they have limitations because they have not been validated or because they refer to direct laryngoscope vision. Given this situation, Chaggar et al.5 developed a pilot study with a specific classification for videolaryngoscopes called VCI (Video Classification of Intubation) that can be very useful in clinical practice.
Likewise, adequate training in the use of the videolaryngoscopes is advisable, not only to achieve the best view, but also to facilitate intubation and reduce the risk of injury. This would help to avoid the Kovac's sign, which involves visualization of the cricoid or cricothyroid membrane through the glottis when performing videolaryngoscopy and indicates poor positioning of the videolaryngoscope blade.6
In view of the above, the objective of this article was to describe the case of a woman who presented a tracheal laceration after an intubation performed with a videolaryngo-scope, and who, due to the rapid identification of the complication and the joint work of a multidisciplinary team, had a complete resolution of the injury. It is also important to highlight that in this case, despite not knowing the exact etiology that caused the rupture, neither the diagnosis nor the initiation of treatment was delayed.
Case presentation
74-year-old woman with a medical history of arterial hypertension and mild mitral and tricuspid insufficiency treated with enalapril and furosemide, as well as a surgical history of vaginal hysterectomy and inguinal herniorrhaphy performed under spinal anesthesia without complications. In December 2020, the patient had COVID-19 and was symptom-free.
The patient was scheduled for a laparoscopic cholecystectomy in June 2021 at a tertiary care hospital in Zaragoza, Spain, and one week before the procedure she attended a pre-anesthetic assessment. In that appointment, analytical tests, electrocardiogram and chest X-ray were reviewed and no alterations were observed. An assessment of the airway was also performed, and the most important data obtained were a Class II score on the Mallampati scale, a mouth opening of 4cm, and thyromental distance >6.5cm. The patient was classified as ASA II according to the American Society of Anesthesiologists (ASA) physical status classification system.
On the day of surgery, the patient underwent peripheral intravenous cannulation and received premedication with 2mg of midazolam and a bolus of fentanyl 150pg. Subsequently, a bolus of 150mg propofol was administered as an anesthetic inducer, as well as a bolus of 45mg rocuronium as a neuromuscular blocker. Once adequate relaxation was obtained, train of four (TOF) monitoring was started, and intubation was performed using a Shiley® endotracheal tube with balloon and Murphy's eye, with an internal diameter of 8mm, and a Storz C-MAC D-Blade® videolaryngoscope.
It should be noted that the anesthesiologist who performed the intubation had extensive experience working with the conventional direct laryngoscope, but little experience with the use of videolaryngoscopes. However, since the patient did not show any evidence of a difficult airway and intubation was not urgent, it was decided to use the entry videolaryngoscope to expand the anesthesiologist's training in the use of these devices.
During the first intubation attempt, only partial visualization of the vocal cords and the glottic space was achieved, and it was not possible to place the tube in the proper direction to introduce it through the glottis. In order to solve this problem, a rigid C-MAC® steel stylet was placed inside the endotracheal tube to increase its curvature and the BURP (backward, upward, right lateral position) maneuver was performed, which consists of moving the thyroid cartilage backward, upward, and to the right. The stylet was removed just before inserting the tube into the trachea, and then the cuff was insufflated without quantifying the inflation pressure by means of a manometer. Once the patient was connected to the ventilator, anesthetic maintenance was achieved with 2% inhaled sevoflurane.
The surgery lasted 75 minutes and 5mg of morphine chloride, 50mg of dexketoprofen, and 1g of paracetamol were used as intravenous analgesia. Moreover, 4mg of ondansetron and 4mg of dexamethasone were administered, also intravenously, to prevent postoperative nausea and vomiting. The patient remained hemodynamically stable without the use of vasopressor drugs and had an oxygen saturation of 99%. Ventilatory parameters showed no alterations and remained unchanged throughout the surgery. No changes were made to the patient's head position. At the end of the procedure, the neuromuscular blockade was reversed with a bolus of 150mg sugammadex and extubation was performed without coughing or respiratory effort. Once extubated, she was taken to the post-anesthesia care unit (PACU) without any further incident during the transfer.
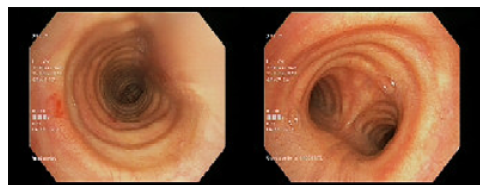
During her stay in the PACU, approximately 20 minutes after the end of surgery, the patient presented several episodes of hemoptysis accompanied by dyspnea and oxygen saturation of 95% which improved with supplemental oxygen at 2L through a nasal cannula. Pulmonary auscultation at that time was unremarkable and no subcutaneous emphysema was found in any location. The case was immediately discussed with the Pulmonology Department, which proceeded to perform a fibrobronchoscopy that showed an erosive, lacerated and bleeding injury of 1.5cm in length on the posterior wall of the trachea and 5cm from the vocal cords (Figure 1). However, due to the active bleeding, it was not possible to establish the depth of the lesion in the thickness of the tracheal wall.
In view of the findings of the fibrobronchoscopy and taking into account that surgical repair of the laceration might be necessary, the Thoracic Surgery Department was informed of the situation. Given the patient's respiratory and hemodynamic stability, immediately after fibrobronchoscopy, tracheal laceration was diagnosed following an emergency chest X-ray and computed axial tomography. The former showed no signs of pneumothorax or pneumomediastinum and the latter showed no images of tracheal disruption or presence of air or mediastinal collections.
Two hours after the intubation incident (with the results of the tests performed and the patient stable), it was decided together with the Pulmonology and Thoracic Surgery Departments to treat the tracheal laceration using a conservative approach. Accordingly, intravenous antibiotic treatment was started with 1g of amoxicillin-clavulanic acid every 8 hours and 500mg of levofloxacin every 24 hours, maintaining the patient in absolute fasting and close monitoring in the PACU for 48 hours. She was then transferred to the surgical floor, where she remained for 24 more hours and was discharged due to her favorable progress.
After discharge, the patient was referred to the Thoracic Surgery Department and at her first follow-up, 10 days after the incident, it was found that she was asymptomatic and continued antibiotic treatment until 10 days had elapsed. During the second follow-up, 20 days after the tracheal laceration, a new fibrobronchoscopy was performed, which showed the tracheal mucosa had healed (Figure 2), so the Thoracic Surgery Department discharged her and indicated that she should be followed up by her primary care physician.
Discussion
Post-intubation tracheal laceration is a rare complication. However, it is difficult to establish its exact incidence because most publications on the subject refer to isolated cases or case series that include a small number of patients.
According to the case series published by Herrmann et al.,3 which included 64 patients with iatrogenic tracheal injury treated between May 2003 and May 2019, these injuries occurred mainly in women (73.4%) and during intubation with a single-lumen tube (45.31%). Moreover, 29.7% of the cases were non-urgent intubations, which is consistent with the present case, in which the intubation performed on the patient was non-urgent and a single-lumen endotracheal tube was used.
The clinical manifestations of tracheal laceration can be quite diverse, and no pathognomonic symptom or sign has been found.4 Still, the most frequent clinical signs of this entity are subcutaneous emphysema, pneumothorax, and pneumomediastinum.7 Other possible clinical manifestations are dyspnea, hypoventilation, cough, hemoptysis, dysphonia, or dysphagia.8 In the present case, hemoptysis was the key symptom to consider the possibility of this complication.
The manifestations of tracheal laceration are not always evident immediately after extubation, which can lead to a delay in diagnosis and, therefore, treatment. In this regard, Miñambres et al.,9 in a meta-analysis that aimed to determine the risk factors that favor tracheal rupture during orotracheal intubation, pointed out that subcutaneous emphysema is not only the most common symptom, but also a protective factor, since its presence provides an early warning of the possible existence of tracheal rupture. In the present case, the early onset of hemoptysis and dyspnea in the patient expedited the performance of diagnostic tests and the implementation of timely therapeutic measures.
Based on the literature review conducted in their case report, Chen et al.10 classified the risk factors for post-intubation tracheal laceration into 3 factors: 1) established risk factors, 2) probable risk factors, and 3) risk factors with no demonstrated evidence. The first risk factors are female sex, age >50 years, intubation with double-lumen tubes, and cuff hyperinflation; the second involve chronic use of corticosteroids, tube misplacement, inexperience of the anesthesiologist, multiple intubation attempts, tracheomalacia, use of rigid stylets, and poor physical condition of the patient; and the third concern obesity, short stature, and percutaneous tracheostomy. Similarly, female sex, advanced age and emergency intubation have been described as the most important non-modifiable risk factors.11In the case reported, the patient presented two of these risk factors: female sex and advanced age; in addition, cuff insufflation was performed routinely, although the balloon inflation pressure should have been controlled by means of a manometer.
In the present case, the inexperience of the anesthesiologist, the use of a rigid stylet, and the BURP maneuver may have contributed to the occurrence of tracheal laceration; besides, the patient's difficult airway (which had not been anticipated in the initial assessment) resulted in the need for two intubation attempts. Although the use of the videolaryngoscope in this case was for training purposes, it was appropriate because the initial use of these devices is recommended in difficult airway situations since they are designed for this purpose.12
As a matter of fact, the Stortz C-MAC D-Blade® videolaryngoscope was used in this patient, which is very useful in difficult intubations because it improves the visualization of the vocal cords due to its crescent-shaped blade and a sharper angulation.13 It is important to keep in mind that, despite providing a better image of the glottis space, with this videolaryngoscope it may be difficult to direct the endotracheal tube, leading to an increase in the number of attempts and lengthening the duration of intubation.14 This difficulty may be overcome by using an stylet, as studies such as that of McElwain et al.15 have shown that in difficult laryngoscopies, the performance of the C-MAC® videolaryngoscope is improved when it is used with a stylet that angles the distal portion of the tracheal tube.
In the present case, intubation was achieved on the second attempt, requiring the use of a rigid stylet to allow for a more marked angulation of the end of the endotracheal tube. In addition, the BURP maneuver helped facilitate both visualization of the glottis and passage of the tube through the vocal cords.
There are multiple models of rigid stylets for endotracheal tubes. In the present case, the C-MAC® rigid stylet was used because it was already available at the hospital where the patient was treated. It is worth noting that in the study by Ömür et al.16 this stylet model proved to reduce intubation time and facilitate the passage of the tube through the cords when using the C-MAC D-Blade® videolaryngoscope.
At the slightest clinical suspicion of tracheal laceration, a diagnostic test should be performed to confirm or rule out the diagnosis of this complication due to its high morbidity and mortality. Fibrobronchoscopy is considered the ideal test17 for this purpose since it allows direct visualization of the injury, showing its exact location in the trachea, as well as its extension and depth.
There is currently no consensus on the therapeutic management of tracheal laceration, so decisions on the most appropriate treatment for each patient should be made by a multidisciplinary team. However, the trend nowadays is to provide conservative treatment in most cases, being this option the most advisable in stable patients with lacerations <2cm and emphysema or moderate non-progressive pneumomediastinum, and with no respiratory involvement, esophageal damage, or signs of mediastinal infection.2,18In the case described above, conservative treatment with intravenous antibiotherapy was chosen, and the patient progressed satisfactorily without presenting any complications.
The main limitation of the present clinical case is that it was not possible to determine the exact mechanism that caused the tracheal laceration. However, this study shows that this complication should be considered when intubating a patient with risk factors for a tracheal injury, even if the intubation is apparently safe, so as not to delay diagnostic tests and treatment.
Conclusions
Post-intubation tracheal laceration should always be considered in patients with risk factors for this type of injury. Moreover, due to its high mortality, timely initiation of diagnostic tests and therapeutic measures is important in order to reduce possible complications and improve prognosis.
Fibrobronchoscopy is the diagnostic test used to confirm the presence of a laceration, and therapeutic decisions should be made early by a multidisciplinary team.
When intubating a patient with risk factors for tracheal laceration, the number of attempts should be minimized, an experienced anesthesiologist should be available, cuff pressure should be controlled with a manometer, the use of rigid stylets should be adequate, and the patient's physical condition should be improved, all of which could prevent this type of injury. It is also important to create a multidisciplinary work team for these cases and to guarantee the availability of diagnostic tests, mainly fibrobronchoscopy.
Although the current trend for the management of tracheal laceration is conservative treatment, there is currently no consensus on the best way to manage this type of complication. Accordingly, further research is needed to develop a protocol along with all the medical specialties involved in the management of these injuries.