With the ongoing advances and evolution in healthcare, we have witnessed new breakpoints in patient management. As a result, there have been tireless efforts to identify and eradicate barriers to care and minimize their impact on patients.
Accordingly, "value-based healthcare" (VBHC) was created looking for a standardized way to measure, provide and remunerate healthcare. The principal purpose does not depend on earnings but on the value, defined as "the favorable outcomes relative to the costs of obtaining them"1.
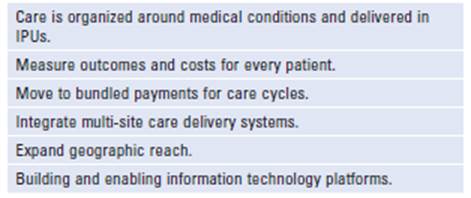
The VBHC strategy is based on six value statements (Table 1) that guide the healthcare plan. The first step is to organize medical conditions around the "integrated practice units" (IPUs) model, where the diagnosis, treatment, and procedures are delivered by a team in fewer appointments instead of multiple individual ones; value-based healthcare aims to provide wellness to the patient and its caregivers in the whole process through a change in the financial approaches of treatments and the quality of outcomes achieved. Once these methods become reliable enough, the larger goal is to use them as a foundation to expand the geographic reach and improve healthcare plans in the surrounding areas1.
This strategy has been studied and widely applied in different disciplines. However, areas such as urology and urooncology lack research and information regarding the use of value-based healthcare. For that reason, Reitblat et al.1 summarized relevant information, which is described in the following:
European and North American healthcare systems have been studied, and the available information is inconclusive to different geographic territories like Asia, Latin America, East Europe, and Africa. For this reason, a worldwide vision of value-based healthcare is still unavailable for urology1.
Regarding care and medical condition surveillance, multidisciplinary clinics allow patients better experi-ences, such as more treatment adherence, higher preventable strategies, and better surveillance for urooncology conditions1. At the same time, when considering the costs, multidisciplinary clinics provide substantial improvements, with more conscious investments, meaning less unnecessary spending1.
Applying systematic outcomes measurement in urology provides immediate information for the leading surgeon. This can facilitate a continuous learning environment through real-time feedback, allowing an improvement in patient care1. As a clear example, we have the routine care provided by the Martini-Klinik in Hamburg, Germany. They implemented the prostate cancer treatment assess-ment and showed that the systematic measure-ment improves the outcomes and stimulates the generation of system tools that can be used in a more accessible manner for every institution2.
One of the pillars of VBHC is the creation of bun-dled payment plans; currently, this is not being implemented in urology. Although the available information only covers the USA, there are no known existent bundled payment plans for urology interventions, mainly because there have not been studies on the topic1.
With all this in mind, we can say that the VBHC is starting to shape how we deliver medical attention in a more human and centered way. It all starts with implementing models that see healthcare as a team-based resource; we need to improve how data is collected alongside the growth of studies focusing on the topic.
By focusing on the principles of patient-centered care, quality and safety, cost-effectiveness, and continuity of care, VBHC can help healthcare providers deliver high-quality care that meets the needs of patients while using healthcare resources efficiently3.
In urology, selected areas such as pediatric urology, female and reconstructive urology, and our focus, genitourinary oncology, already show that the use of multidisciplinary clinic models that focus on value-based healthcare instead of volume-based healthcare improve the outcomes and should become the standard plan for care4.
The plans include multiple visits in one appointment to different care providers in the exact location. This model reduces the impact of several appointments in the patient's life, optimizing their time and reducing unnecessary costs. At the same time, having more organized medical schedules allow patients to understand a more linear path to their diagnosis, treatment plan, and procedures. In the long run, it translates into enhanced decisions made without rushing with good communication between caregiver and patient.
For a more specific scenario, prostate cancer patients who are treated in multidisciplinary clinics show better outcomes than those who are not4. In the USA, the treatment for prostate cancer is still in charge of urologists that do not work in a specialized cancer center, and it leads to a not standardized plan for the treatment that differs not only in price and procedures but in outcomes. Creating multidisciplinary clinics for the treatment will improve and unify the existing plans looking for the best and most useful one that improves outcomes for patients and caregivers.
Improved communication with patients can increase their willingness to participate in clinical trials or research4, which benefits the medical community. This allows gathering valuable information to continue improving the quality of healthcare provided. We should also keep in mind that the standardization in the data collection using patient reported oriented instruments is essential to minimize missing information and achieve quality research data without losing time5.
The future of value-based urology lies in the continued emphasis on patient-centered care and technology integration into urological practice. Patient-reported outcomes and satisfaction metrics will become increasingly important in assessing the value of urological care. Finally, collaborations between healthcare providers, payers, and patients will drive value-based urology forward. It is crucial to continue researching and applying the tools that we have, to achieve the best healthcare that can be given and close the gaps between cost and outcome that modern medicine creates each day.