INTRODUCTION
Metabolic syndrome (MS) is a group of closely linked conditions, which generate a considerable increase in the risk for cardiovascular disease and diabetes, almost double when compared to people who do not have it. MS is characterized by insulin resistance, excess weight, glucose intolerance, dyslipidemia, high triglycerides and low high-density lipoprotein cholesterol (HDL), inflammation, and prothrombotic state. 1
The International Diabetes Federation (IDF), the National Cholesterol Education Program Adult Treatment Panel III (ATP III), and the American Association of Clinical Endocrinologists (AACE), as well as the World Health Organization (WHO), have formulated their own diagnostic criteria for (MS) 2. The Latin American Diabetes Association (ALAD), based on the definition of the IDF, defines the figures for evaluation of abdominal perimeter in the Latin America Region 3.
Regardless of the classification system, the main concern is early detection and timely intervention.
Most people with MS will develop insulin resistance, which increases the risk for type 2 diabetes. When this type of diabetes is clinically noticeable, the risk of cardiovascular disease rises very noticeably. 4
Interventions have been implemented around the world to find functional strategies to reverse smetabolic syndrome and they range from the use of herbal medicine, alternative and complementary medicine, supplements, probiotic use, drug therapy, bariatric surgery, gut microbiome transplantation, lifestyle changes, and counseling, as well as physical activation and diet, exercise practice, dietary regime.
The purpose of this study is to conduct a systematic literature review to analyze the characteristics of the interventions that combine two or more therapeutic aspects for the control and management of metabolic syndrome.
Methodology
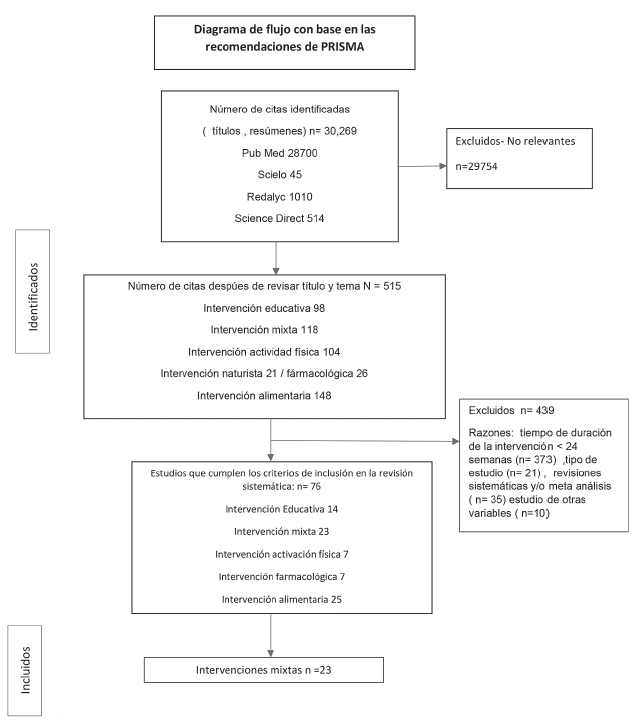
Systematic literature review using the PRISMA criteria. Data collection was carried out from scientific articles published between 2011 and 2021, and whose objective was focused on the effect of interventions on metabolic syndrome.
The review was carried out with the purpose of extracting data and obtaining various intervention alternatives, such as: 1. Lifestyle interventions, including educational interventions (physical or nutritional activation counseling), physical activity, and a dietary approach, 2. Pharmacological, herbal or supplemental interventions, 3. The combination between any of the aforementioned (mixed intervention).
Search Strategy
For the systematic literature review, keywords were used in two categories: from the type of intervention performed in metabolic syndrome, and methodological specification for the characterization of clinical studies.
The articles were obtained from the keywords of the term's metabolic syndrome, intervention, and human. In the collection of clinical studies, the terms article, clinical trial, controlled clinical trial, controlled study, randomized controlled trial, randomized trial, and placebo were used.
We classified identified manuscripts/articles according to inclusion and exclusion criteria to obtain the studies to be analyzed from the interventions with the best effect on metabolic syndrome.
The search strategy was carried out in the databases: Pub Med, Science Direct, Scielo, Redalyc. Once the search was completed, duplicates were excluded, and a database was designed to record the relevant documents for review.
Selection of Studies
The search yielded a total of 30,269 articles, in which specific inclusion and exclusion criteria were used to select the information and compare the various interventions used in the resolution of some aspect of metabolic syndrome.
Inclusion Criteria
Controlled trials in human populations in any age range, the sample of which included a proportion of patients (greater than 1), contained participants diagnosed with metabolic syndrome, and included interventions lasting 24 weeks or more, with or without follow-up.
We classified interventions as lifestyle-related (diet, physical activity, and educational interventions), and as pharmaceutical treatments (medicines or dietary supplements), alone or in combination with any of the lifestyle-related interventions. Articles were included in several languages, and also those in which the diagnosis of metabolic syndrome and the quantifiable parameters before and after the intervention or the combination of these were available.
Exclusion Criteria
Systematic reviews, meta-analyses, pilot studies, intervention proposals, protocols, testing of educational materials and scales, other measurement elements, as well as studies in which the aspects obtained by the results focused on enzymatic, molecular, and hormonal levels that were different from the clinical parameters that make up the diagnosis of metabolic syndrome were excluded. Interventions such as bariatric surgery (with or without lifestyle components) or mi-crobiota transplantation, studies in pregnant women, or in patients with specific pathologies, such as surgical procedures combined with lifestyle modifications, were excluded.
Extracting the Data
A strategy for the extraction and evaluation of data from selected publications was designed, using keywords and capturing data in Excel to verify that the selected revisions met the terms and criteria for inclusion and exclusion. Articles from primary research, country, year, population under study, purpose, type of intervention, duration, outcome, conclusions, and limitations, were taken into account.
RESULTS
30,269 publications of interventions published from January 2011 to November 2021, which met the criteria, were identified. This included the duration and type of intervention. A total of 76 interventions for MS with duration greater than 24 weeks, 14 educational interventions, 7 interventions focusing on activity physical, 7 pharmacological interventions, 25 dietary or dietary interventions, leaving, 23 mixed interventions, that is, two or more of the treatments implemented for metabolic syndrome were combined (dietary counseling, physical activation counseling, practice of physical activity or supervised sessions, implementation of diet, as well as multidisciplinary management in the lifestyle). Therefore, we reviewed the publications in which a mixed intervention for metabolic syndrome was performed.
The lifestyle-based interventions were 19, two interventions based solely on physical activity and diet, one intervention based on body-mind exercise (yoga), including physical activity and caloric intake, another of omega 3 dietary supplement and oleate, plus physical training. In 6 studies, the interventions were performed in children and the remaining 17 interventions in adults.
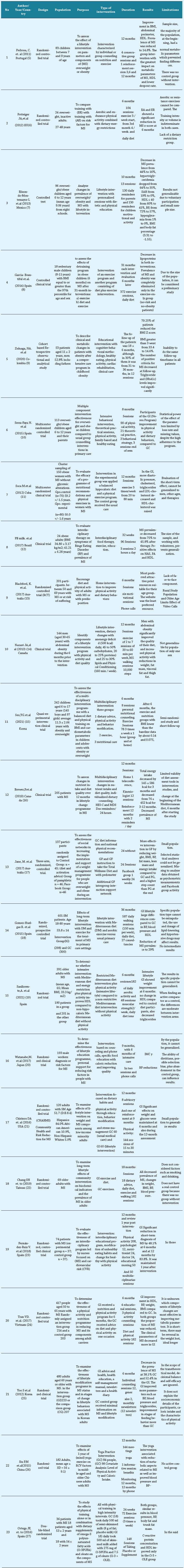
The characteristics of the interventions are detailed in Table 1.
Table 1 shows the selection process for manuscripts selected for review. These studies were conducted in Europe (Portugal, Spain), Asia (Korea, Japan, Taiwan, Vietnam, and China), America (Canada, United States, Mexico, Cuba, Colombia, and Brazil), and Oceania (Australia).
Note: Classification of publications according to exclusion and inclusion criteria.
A decrease in the prevalence of MS, and/or its cardiometabolic parameters contemplated in the quantification studies at the beginning, and whose condition was modified in the course of the intervention, was classified as good of the intervention.
Interventions in Children
A total of 605 participants between the ages of 6 and 17 were included in the analysis. The duration was between 6 and 31 months. One of the interventions for children assessed the effect of detraining after 31 months of intervention; the remaining 5 studies were educational and multidisciplinary lifestyle interventions. In one study, individual educational counseling compared with group counseling on good nutrition and exercise, the latter had a better effect by decreasing MS parameters, showing less dropout. An educational intervention in the school environment focused on lifestyle, personalized by instructing parents or caregivers, significantly decreased all parameters, as well as the prevalence of MS. There was no negative effect on detraining 6 months after diet and exercise interventions. Educational intervention aimed at patients and parents, or caregivers combined with physical activity sessions, reduced the criteria as the diagnosis of MS improved. The Nereu program, characterized by behavioral interventions for children and families in an integrated manner, presented an improvement in eating and physical behaviors. In mul-tidisciplinary intervals with constant physical activation and adequate feeding, MS parameters were reduced. Interventions in children in food and physical counselling showed improvement in clinical parameters and decreased MS prevalence.
Interventions in Adults
There were 3448 adults included in the reviewed studies, with ages between 27 and 69 years. Adult interventions lasted between 6 and 36 months. Four interventions did not include females in the sample; however, results did not differ from those found in populations of both sexes. The interventions positively impacted the clinical parameters of MS, reduced its prevalence, or achieved a change in eating behavior and physical activity.
DISCUSSION
The result of our review supports previous findings (Aguilar et.al, 2014) which found that, if in an intervention includes physical activity, diet, and reinforcements (positive???), better results are obtained. The collaboration of the family is a factor of greater impact than food education itself, when it comes to guaranteeing results. In the present 28 review, group counseling was effective among children, and the use of motivational reminders against sedentary lifestyle were regarded as useful tools. The group approach reinforced adherence. Personalized, multidisciplinary care in children with family support offers success in acquiring healthy lifestyles such as diet and physical activation.
Regardless of a personalized or group intervention for children, family involvement helped decrease MS, overweight, and obesity. When the mixed intervention included diet, there are good results in decreasing MS. The Mediterranean diet, which was the most implemented in the present review, shows good reduction of energy intake, optimization of the regimen with 24-hour reminders, constant nutritional advice, and ideas for adaptations to the Mediterranean diet.
The symptoms of binge eating disorder, which are excessive and recurrent food intake, with the feeling of losing control, without compensatory and appropriate weight control behaviors, were controlled in one of the multidisciplinary interventions, as well as the decrease in the prevalence of MS from 75% to 45% and changes in metabolic parameters. 29 Binge eating disorder (BED) is considered the most prevalent food disorder, and a major risk factor for obesity and MS. 30
Findings from educational home intervention on healthy lifestyles in adults from rural communities in Australia (Blackford K, et.al, 2019) 19 suggest the majority of people in this study preferred printed resources to the Internet. We considered that this phenomenon could be attributable to population characteristics such as age, rurality, and disinterest in access to technology. This result contrasts with another Australian study (Jane M et al., 2017) 23, which found that using the web (Facebook) worked as an excellent tool as a support network to modify diet and physical activity for weight control. It appears that technology could serve as a barrier or facilitator, depending on the population group, when addressing MS in different population groups.
We found similarity with what was stated by Yamaoka K et al. (2012) in relation to the improvement of the cardiometric parameters 31 of MS since the lifestyle interventions in the significantly reduced the mean values of blood pressure and the abdominal perimeter.
Evidence from clinical trials (32, 33, and 34) has shown that the key points to prevent diabetes in adults are increased physical activity and weight loss. In people at risk of developing type 2 diabetes, it was possible to reduce the risk by 50 to 60% in the intervention period of 3 to 6 years, through the combination of diet, exercise, with the objectives of weight loss and increase in physical activation and, despite decreasing, the effect of the intervention may continue (35, 36, and 37). The large-scale implementation of dietary interventions and physical activity in clinical settings and communities is beginning to be carried out, but requires dissemination.
It is not yet decisive how it is recommended to carry out the reinforcement and if it is different in children or adults, since the maintenance phase must be structured to extend as long as possible the change of behavior and habits that favor the healthy lifestyle become customary. Having access to information technologies motivates us to imagine that the maintenance of what has been learned in the interventions will be strengthened with interactive virtual programs and constant communication for the user, and that it will possibly be an accessible instrument in interventions for children.
In the present review, one study (Fernández-Ruiz et al., 2018) 30) demonstrated effectiveness and efficacy in MS reduction of an interdisciplinary nursing-guided intervention at 6, 12, and 24 months, respectively, with a reduction in metabolic syndrome of 83.8% at 12 months. The literature suggests that interventions that transmit knowledge, modify sedentary lifestyle, change dietary patterns, promote self-care, and promote self-responsibility, positively change the health conditions of society. The literature also suggests that reinforcement is indispensable for permanent change.
Findings from this literature review support previous findings (Dunkley AJ et al., 2012) 38 that any interventions is useful to reverse metabolic syndrome, but multidisciplinary lifestyle interventions (Guzmán A et al., 2019) are more effective by promoting the acquisition of behaviors that modify and prevent metabolic syndrome in a more lasting way. Based on this review, a minimum of 24 weeks is ideal for optimal results
CONCLUSIONS
Attention to MS includes the reduction of its causes (obesity and physical inactivity) and the treatment of associated risk factors through the modification of lifestyles, especially nutritional habits and physical activity. In children, interventions in school environments control and decrease MS, group participation leads to a lower dropout rate, there is more effectiveness in integrating the family, and the reduction in prevalence in individual or group programs is similar.
More experience and implementation of adaptable and modifiable models in the different populations at risk is required, to be able to make primary care more efficient and effective in the management and knowledge of metabolic syndrome, and realize the importance of intervening, as well as disseminating throughout the population, the tangible benefits of stopping before the appearance of something that will bring the imminent deterioration of health.
Interventions that combine the promotion of healthy lifestyles, diet, and physical activation show a clear improvement in the prevalence of metabolic syndrome, as well as in decreasing the number of cardiometabolic risk factors in the people under study. Programs are effective in a wide range of characteristics, but interdisciplinary lifestyle interventions seem to be better at achieving the desired goal. It is necessary to implement long-term designed interventions, and to monitor the results to know which objectives that were achieved in the control are the most impactful, and how to make them permanent through reinforcement, evaluation, and continuous feedback, to achieve effective strategies to prevent and control Metabolic Syndrome, and that could be managed as health policies.