Introduction
Radical cystectomy in women poses a special challenge from the urinary diversion standpoint. During the last 50 years, reconstruction of the lower urinary tract has evolved from cutaneous incontinence1,2 to orthotopic continent diversion to the intact native urethra. Choosing an orthotopic neobladder is appealing from both the cosmetic and functional points of view, but increases the risk of complications such as stress urinary incontinence and neobladder vaginal fistula (NBVF) development.
Initial management of NBVF usually involves an attempt to close the fistula from a vaginal approach. The abdominal approach is less popular among patients and surgeons since the surgery becomes more challenging due to adhesions. There is a high-risk of damaging the neobladder, the ureters, the bowel, and the rectus. Irreparable damage to the neobladder may require removing it and building up a new one or even performing an undiversion to the ileal conduit or heterotopic reservoir. There are few reports regarding vaginal closure of NBVF, and success rates are low3,4. Failure is the most likely outcome after vaginal surgery. In this setting, the next step is to perform an abdominal closure attempt or a urinary undiversion. Since closing the fistula from the abdominal approach is most of the time not feasible, urinary undiversion is the usual way to go.
Urinary undiversion involves highly complex surgical procedures, where the mean focus is improving quality of life (QOL). Complications during and after surgery are highly frequent. This probably explains the low number of procedures around the world and the limited number of publications about this subject5,6.
Our aim is to describe the resolution of three cases of laparoscopic urinary undiversion due to recurrent NBVF in a single center.
Materials and methods
We performed a retrospective review of patients who underwent urinary undiversion due to NBVF from January 2015 to 2022. Information was collected from patients' electronic medical records with previous informed consent.
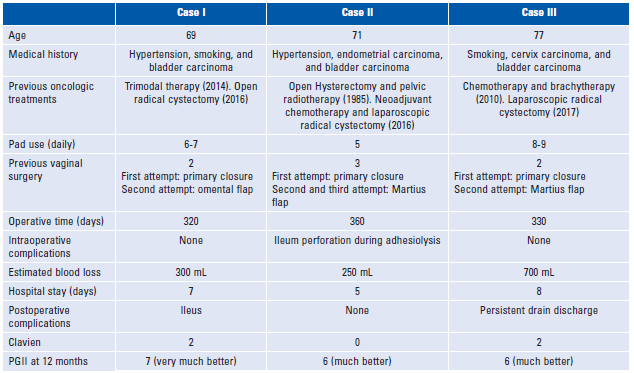
The information assessed was: age medical history, previous oncologic treatments, number of pads used daily, previous closure attempts, characteristics of undiversion surgery, hospitalization time, and postoperative complications according to Clavien classification.
All patients completed the Patient Global Impression of Improvement Questionnaire (PGII) at 12 months of follow-up to assess postoperative QOL.
Surgical technique
A Foley catheter was placed in the fistula. Fanshaped trocar placement was performed, one umbilical 12 mm trocar, two 12 mm trocars in both flanks, and two 5 mm trocars in both iliac fossae. Firstly we performed adhesiolysis followed by neobladder and bilateral ureter dissection. The distal aspect of the neobladder was opened to identify the fistula. The neobladder was fully dissected en bloc with the distal aspect of both ureters using a harmonic scalpel and bipolar cutting device. The specimen was removed in a bag through the vagina. The vaginal defect was closed using a running barbed suture. We selected the ileal portion of the future conduit 20 cm proximally to the ileocecal valve. Enterotomy and entero-enteric anastomosis were performed with mechanical sutures. Termino-lateral ureteral reimplantation was done using absorbable multifilament suture and simple J stents were placed on both ureters intracorporeally. A urethral drainage was placed and the conduit was exteriorized through the right flank port.
Results
During the study period, three laparoscopic urinary undiversions were performed in a single center. Patient characteristics and outcomes are shown in Table 1. In all cases, an ileal conduit was built intracorporeally. With a median follow-up of 18 months, there were no long-term complications.
Discussion
Urinary tract diversion is a complex choice after radical cystectomy. Most of the postoperative complications, both in the short and long-term are related to the urinary diversion and the necessary steps to build it. Neobladders may appear as the best possible diversion since they resemble normal urinary tract physiology. Even though, neobladders may come at a high cost, especially in women, when a NBVF is developed.
Refunctionalization of the diverted urinary tract was popularized by Hendren7 with favorable results reported by numerous authors. Most cases initially reported were pediatric patients who underwent urinary diversions (UD) for obstruction, myelodysplasia, or vesicoureteral reflux.
Undiversions to orthotopic continent reservoirs, heterotopic continent reservoirs, and even laparoscopic approaches have been described by different authors7-11. However, with the increasing number of cystectomies, we believe that more reports of Urinary undiversion are necessary12,13.
The largest single-center urinary undiversion series was reported by Hautmann et al.14 In 51 cases, secondary or tertiary surgeries were performed for oncologic (n = 23) and nononcologic (n = 28) indications using an open approach. Most reports of urinary undiversion are from an incontinent to a continent reservoir8,14-16. In our three cases, an orthotopic continent reservoir to an incontinent Bricker-type ileal conduit was performed, due to a nononcological complication, a previous unsuccessful surgical fistulectomy. Patients were free of oncologic disease, with a good performance status but severe deterioration of their QOL related to permanent urinary leakage.
In this study, we found that all patients failed the vaginal closure attempts and since abdominal closure was highly challenging, we decided to perform a urinary undiversion and ileal conduit. We decided to perform a new ileal conduit due to the neobladder injury during adhesiolysis associated with the large defect in the urinary fistula.
Despite other authors having described the use of urinary undiversion after the failure of fistula closure3,4,17, we haven't found other reports in the literature regarding the laparoscopic approach. Other series have described better results in NBVF closure, with success rates of up to 61.5%.17,4 All the remaining patients that failed fistula closure underwent urinary undiversion. Our low rate of success in fistula closure may be related to the fact that all of our patients had had previous pelvic radiotherapy. However, another topic to highlight is QOL after NBVF, since other authors that succeeded in closure have described severe stress urinary incontinence18. In spite of requiring a urinary undiversion, our patients had a high degree of satisfaction according to the PGII.
As previously mentioned, we consider that being an infrequent procedure that requires complexity and experience both in the surgical team and in the perioperative management, an interdisciplinary approach is needed as well as a highly complex intensive care unit, without neglecting that selection of patients is a core principle of urinary undiversion. Patients must be well-informed and determined to undergo this type of treatment. We would like to highlight that the cornerstone of this surgery is to perform it in experienced hands regardless of the chosen approach. However, the laparoscopic approach provides greater benefits in the recovery of our patients.
The primary limitations of our study are the retrospective nature, the low number of patients recruited, and from a single center. Furthermore, we did not measure the fistula size. However, despite having experience in the resolution of complex fistulas through the vagina, we consider that our casuistry could be relevant due to the scarcity of studies regarding recurrent NBVF solved through the laparoscopic approach.
Conclusion
Urinary undiversion is, despite being a last resort, a complex procedure. Even though, it may be the only chance to improve QOL in patients with recurrent or unrepairable NBVF. In spite of this, it is feasible to perform laparoscopy and stands as a valid alternative in patients with recurrent lower urinary tract fistulas. A laparoscopic approach with neocystostomy, fistulectomy, and intracorporeal ileal conduit is feasible but requires a high degree of surgical expertise in laparoscopy. Further studies are required to assess the best approach in the management of NBVF. Even though surgical experience and interdisciplinary management are required, it offers a suitable resolution with clear improvements in the patient's QOL.