Introduction
A well-functioning and safe vascular access (VA) for chronic hemodialysis (HD), must ensure adequate blood flow to achieve the goals of dialysis therapy. The evidence summarized in management guidelines by many international committees and medical associations, recommends the arteriovenous fistula (AVF) as the best option for VA (1-3). Notwithstanding the clearness of the evidence, and systematic efforts to increase the proportion of HD patients with a permanent AVF access, there is wide variability in the use of different VA for chronic HD across the world (4-7). This body of evidence, showcases that the onset of HD with a vascular catheter has been associated with a significant increase in mortality (8, 9), and fatal infections (10).
Several studies have focused on identifying factors related to the patency of access for HD (11, 12); where it has been observed that the age, female gender, diabetes, the history of smoking, and the poor initial blood flow, among others, are risk factors for VA failure. Likewise, the longitudinal follow-up of HD cohorts shows that survival of VA, and the frequency of related procedures are variable and not uncommon (7). It should be noted, that the frequency of use of the different VAs for HD varies according to the clinical scenario, clinical practice patterns, and the time of clinical course within the chronic HD program (6).
To contextualize, Baxter Renal Care Services (BRCS) is a network of renal care clinics in Colombia, which provides dialysis care to around 9.000 patients; with 60 % of this population in hemodialysis. A dialysis care based on standardized process and procedures allows to reach quality indicators in dialysis, such as a proportion of patients with AVF greater than 80 % (13).
BRCS clinical teams use temporary vascular access (non-tunneled catheter, cuffed catheter) when urgent HD had performed or when AVF or arteriovenous graft (AVG) were not possible to create, following the clinical practice guidelines for vascular access (1, 2). The decision of vascular access type made, takes into consideration factors such as life expectancy, comorbidities, and vascular system status. The objective of this study, is to describe the pattern of use of VA for HD, the frequency of VA failure, and the factors associated with failure in 15 months of follow-up.
Materials and methods
Study Design and Patients
This is a retrospective cohort study of end-stage renal disease (ESRD) patients, treated in BRCS Colombia network between January 1rst and December 31, 2016. We included hemodialysis patients with cohort’s inception the first day of HD. The patients had a potential follow-up time within the cohort of up to 15 months from the inception. The inclusion criteria were patients over 18 years of age, with diagnosis of ESRD, incidents in HD; however, we excluded of the analysis patients with more than one active vascular access at the study inception. Data collected included demographics, CKD cause, presence of diabetes, hypertension, cardiovascular disease, characteristics of vascular access, and laboratory data.
Vascular access
All dialysis accesses within the study period were tracked; at the inception (day 1 of HD) we recorded the first access and then, we followed the patient until its VA failure or elective change, with follow-up of all the eventual changes in vascular access. Patients were followed within the study from their inception until the end of the follow-up period, death or loss of follow-up were considered as right censored.
The analysis of person-time in risk was based on the vascular access type in use; when one VA was changed to another one, the remainder of his or her person-time contribution was attributed to the new vascular access type in use. Thus, data of multiple entries from the same patient were possible.
Outcome
Vascular access failure was defined as access that could no longer be used for effectively perform the HD procedure, secondary to dysfunction or infection and required VA change or closure.
Statistical analysis
Descriptive statistics were used to report the population characteristics, using mean and standard deviation for normally distributed variables, and median and inter-quartile range (IQR) for non-normally distributed variables. We evaluated time to VA failure using Kaplan-Meier failure function, to estimate the cumulative probability during the follow-up. Survival time was calculated from the date of access first use until the date of failure. Patients were censored if there were an elective change of vascular access, kidney transplant, switch to peritoneal dialysis, change of provider or lost to follow-up. Only in the group of permanent VA we used multivariable analysis to determine risk factors of failure; this, because in the case of catheters, the access’s failure is due to factors inherent to the catheter and not to modifiable factors. For analyzing time until failure, dealing with recurring-event data, the models included the Andersen Gill extension to the Cox proportional hazard models (14). These models considered independent variables as age, gender, rural/urban origins, diabetes, hypertension and levels of hemoglobin, albumin and calcium, and in addition, the effect of gender-age interaction was evaluated.
The backward stepwise regression method was applied for variable selection to have a more parsimonious model using a fixed p-value threshold of 0.15 which was defined according to what is widely accepted to build a model that contains significant covariates and confounders proposed by Hosmer and Lemeshow (15). The proportional hazards assumption was evaluated using Schoenfeld residuals for each predictor. For hypothesis testing, P-values of less than 0.05 were considered statistically significant, except for stepwise procedures and the 95 % confidence intervals (CI) for the estimators were calculated. STATA 14.2® (StataCorp LLC, College Station, Texas) was used in the statistical analyses.
Results
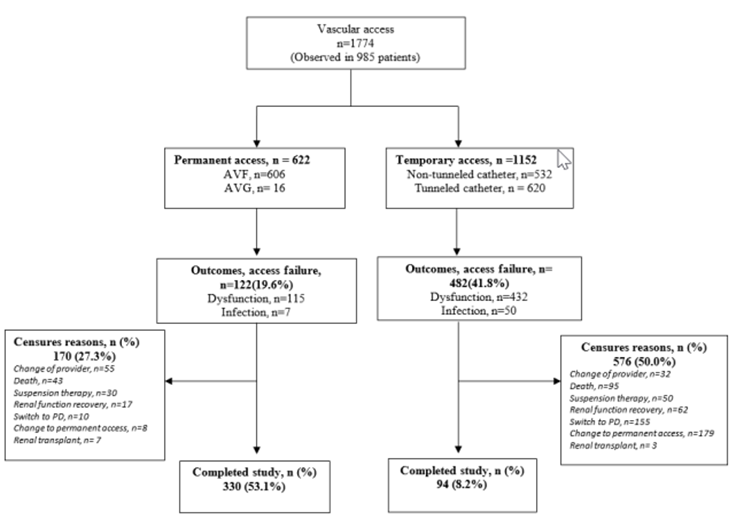
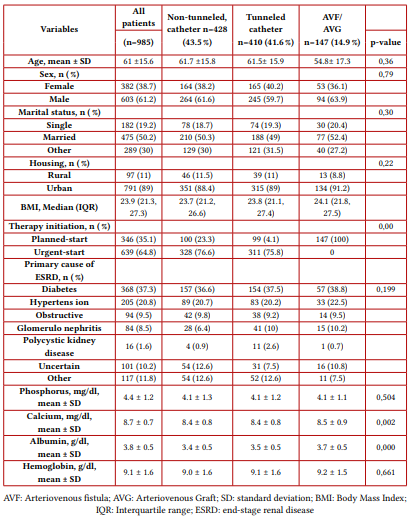
A total of 985 patients were included in this analysis, which required 1774 procedures for vascular access during follow-up; mean age was 61 ± 15.6 years, 37.3 % of the population (N=368) had diabetes mellitus (DM) as the cause of ESRD; details of demographic and clinical characteristics are presented in Table 1. Of the total vascular accesses recorded during follow-up, 35 % (N = 622) were AVF/AVG (See Figure 1). At day 1 of HD, 15 % of the patients had AVF/AVG, and at day 90 this proportion had increased to 70 % after change of temporary vascular access (See Figure 2).
Note: The diagram shows the flow of vascular accesses, a total 1774 vascular accesses were observed in 985 patients (corresponds to the total number of incident adult patients on hemodialysis at RTS network in Colombia), 35 % (n = 622) were AVF/AVG. Likewise, we can also observe the distribution of outcomes and censures during the follow-up of vascular access.
Note: This figure shows that at day 1 of HD, 15 % of the patients had AVF/AVG, and at day 90 this proportion had increased to 70 %. AVF: Arteriovenous fistula; AVG: Arteriovenous Graft.

Source: the authors.
Figure 2 Vascular Access distribution comparing day 1 and day 90 of hemodialysis initiation
Vascular access procedures
The 1774 procedures for vascular access performed during the 15-month follow-up, represented a rate of 1.95 procedures per patient-year, 95 % CI 1.86 - 2.04; details are presented in table 2.
Vascular access failure
In 985 patients, 604 vascular access failures were observed, which represents a rate of 0.66 events per patient-year, 95 % CI 0.61 - 0.72. According to the type of access, the failure function estimated at 3, 6, 9, 12, and 15 months are presented in table 3.
Multivariable analysis
For the 622 AVF / AVG, the best subset of variables in the Cox model using stepwise regression included: being diabetic, female, and living in rural areas, which showed the higher hazard ratio (HR) in this model Table (4).
Discussion
The ideal vascular access for HD should provide a safe therapy that allows for an adequate flow rate, be easy to use, reliable, and have a minimal risk of complications. However, the provision of good quality access is a matter still difficult to achieve (2, 16). Studies have consistently shown that AVF presents better survival and less occurrence of complications compared to AVG and CVC (5,9). Nevertheless, despite the clarity of the evidence, and the systematic efforts that propose the AVF as the best access, there is wide variability in the use of different vascular accesses for chronic hemodialysis worldwide (5-7, 17). Our study shows that the proportion of patients receiving dialysis with AVF or AVG at the beginning was around 15 %, and this proportion changed to about 70 % after the day 90th after conversion from CVC, requiring a frequency of procedures close to 2 per patient -year. Yet, there were some patients that presented non-tunneled catheters for so many months, this was mainly explained by two reasons: first, impossibility to achieve an AVF and second, patient desire (a few patients do not want an AVF for cosmetic reasons).
We also found a VA failure rate of 0.66 events per patient-year, which is much higher in catheters than in fistulas, and should move our efforts to achieve VA based on AVF or AVG. It is known that VA failure remains the leading cause of morbidity and a significant cause of mortality in patients with HD therapy (11). Although many factors related to VA failure have been described, access dysfunction can be attributed to many causes, and the progression from dysfunction to corresponding non-function varies accordingly (1). There are several studies aimed at identifying factors related to the VA patency, which found that age, female sex, diabetes, smoking history, and poor initial blood flow, among others, are risk factors of VA failure maturation (11-18).
The multivariable analysis showed that factors associated with permanent vascular access failure were: age over 65, female sex, and diabetes, as seen in the literature (7, 12, 19-21). It is noteworthy that two additional factors appear associated with this outcome: rural housing that confers significant high risk, and the hemoglobin that is a protective factor.
We hypothesize that rural housing may imply a condition that brings together several socio-economic and cultural determinants of health that can negatively impact this outcome, as seen in peritoneal dialysis programs (22). Moreover, the finding of hemoglobin as a protective factor is striking, which could be explained as that hemoglobin protects against access failure when evaluated as a continuous variable, which implies that for each g/dL of hemoglobin, there is a decrease in risk of around 30 %. The model does not establish a ceiling level for this protection. In the literature, it is known that hemoglobin level above 13.0 g/dL begins to be a risk factor for vascular access failure (23).
To highlight the strength of the study, we could mention that it is a cohort of incident patients in HD with a substantial number of subjects and, with a follow-up from day 1 of dialysis up to 15 months, which allows to describe and estimate patterns of therapy and frequency of events very precisely and illustratively. However, some weaknesses of this study should be pointed out, such as the fact of not having pre-surgical vascular assessment information or detailed vascular information of permanent vascular accesses, variables that are surely also related to the outcome of access.
Conclusion
In this cohort of incident HD patients, vascular access failure for dialysis was frequent, particularly in vascular catheters, which implies a high frequency of procedures related to maintaining vascular access. Factors associated with the failure of access were age over 65, female sex, the presence of diabetes, anemia and rural housing.