Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957
Rev Col Gastroenterol vol.30 no.2 Bogotá abr./jun. 2015
Gastric Xanthoma is Associated with Malignant ad Premalignant Lesions
Martín Alonso Gómez Z. MD. (1), William Otero R. MD. (2), Melisa Buitrago MD. (3)
(1) Professor of Medicine, Universidad Nacional de Colombia. Gastroenterology and Endoscopy Unit (UGEC), Hospital El Tunal. Bogota, Colombia.
(2) Professor of Medicine, Gastroenterology Unit, Universidad Nacional de Colombia. Gastroenterologist, Clínica Fundadores. Bogotá, Colombia.
(3) General practitioner, Universidad Nacional de Colombia. General Surgery Fellow, Hospital El Tunal. Bogota, Colombia.
Received: 15-08-14 Accepted: 06-04-15
Abstract
Gastric xanthoma lesions, which involve lipid accumulation in the gastric mucosa, are found incidentally during upper endoscopy. These lesions have been reported in series of cases associated with metaplasia or atrophy and in reports that link them to gastric cancer, but no analysis has been done to date that examines the possible connections among these associations. The aim of this study was to evaluate whether patients with xanthoma have more malignant lesions (dysplasia or cancer) or premalignant conditions (atrophy or metaplasia).
Materials and Methods: This is a retrospective case-control study that was conducted in the Hospital El Tunal among patients who underwent upper endoscopies for evaluation of dyspepsia. Participants were chosen at random from among patients who had symptoms of dyspepsia. Each participant underwent endoscopy to check for xanthoma on the same day. All patients had biopsies taken and were assessed histologically for H. pylori infection.
Results: The study enrolled a total of 186 patients who met the inclusion criteria of requiring upper endoscopy due to symptoms of dyspepsia. as was indicated field-work one EVDA that with uninvestigated dyspepsia were recruited. Two groups of patients were compared: one included 90 patients who were diagnosed with xanthoma through gastric endoscopy (n = 90), and another group which consisted of 96 patients in whom no symptoms of xanthoma were found. The average age of the patients with xanthoma was 57.4 years while the average age of the control group was 38.3 years. 35% of the xanthoma group were male while 35.6% of the control group were male. 72% of the patients in the xanthoma group had only one lesion: 53% were located in the antrum, 32% were located in the corpus, 10% in the antrum or corpus, and 5% in the fundus. Among patients without xanthomas, there were no cases of dysplasia (0%) while 5.5% of the patients with xanthomas (5 cases) developed dysplasia. Two were low grade and three were high grade. 66% of the xanthoma group and 85% of the control group had H. pylori infections. Three patients in xanthoma group (3.3%) had early gastric cancer, but no patients in the control group had early gastric cancer.
Conclusion: Our study shows that gastric xanthomas are a risk factor for the premalignant conditions of atrophy and intestinal metaplasia. Most importantly, they are associated with dysplasia and gastric cancer which obliges us to be even more careful with endoscopic evaluations when we find xanthoma incidentally. Probably, these findings should be followed up with gastric mapping because of the high probability that we will find a premalignant condition. Nevertheless, larger multicenter studies to test these associations still need to be done.
Keywords
Xanthoma, cancer, dysplasia, metaplasia, atrophy.
INTRODUCTION
Gastric xanthomas, also known as xanthelasmas, are rare tumor-like lesions. They appear as plaques or yellowish-white nodules that vary in size from 0.3 mm to 10 mm. They can be found in any part of the mucosa of the gastrointestinal tract but are most often found in the stomach (76%) especially in the antrum and prepyloric region (70%). Six percent of gastric xanthomas are found in the esophagus, an additional twelve percent are found in the duodenum and colon additional (1). They occur in groups of more than one in 13% to 24% of cases, and 17% of patients have 5 or more lesions simultaneously. From a clinical point of view they do not produce definite symptoms. Diagnosis is usually a pathological finding after an endoscopist takes a sample of the lesion. Although population studies have shown an incidence of 0.018% for gastric xanthomas, endoscopic studies have reported an incidence of 2% to 9% in the general population. The incidence is even higher in patients with previous gastric resections, gastric ulcers or active lesions. Xanthomatosis is considered to occur more frequently with age reaching a peak of 40% of patients in the seventh decade of life (2). On the other hand, case reports have suggested that these lesions may be associated with gastric cancer due to chronic inflammation of the mucosa (3).
The main objective of this study is to evaluate whether patients with gastric xanthomas have a greater number of premalignant conditions (atrophy or metaplasia) or malignant lesions (dysplasia or cancer) than do patients with dyspepsia who have no xanthomas.
OBJECTIVES
General Objective
The general objective of this study is to determine whether patients with gastric xanthomas have a higher incidence of gastric cancer or premalignant conditions than a population with dyspepsia.
Specific Objectives
The specific objective of his study are to establish the incidence of gastric xanthomas among patients who underwent upper endoscopies, to determine the primary locations of xanthomas and their endoscopic characteristics, and to determine whether there are relations between the clinical characteristics of patients and the presence of xanthomas.
MATERIALS AND METHODS
Type of study
This is a retrospective case-control study.
Population and sample
The reference population consisted of adult patients treated at the Hospital El Tunal in Bogotá while the study population consisted of patients who underwent upper endoscopies in the Gastroenterology Unit from August 2007 to August 2012.
Two groups were evaluated. Group I consisted of patients diagnosed with gastric xanthomas confirmed by biopsy. Group II consisted of patients without endoscopic evidence of xanthoma who underwent upper endoscopies to evaluate dyspepsia on the same day as patients in Group 1 and who were otherwise randomly chosen.
Inclusion and exclusion criteria
Inclusion criteria
- Patients older than 18 years.
- Patients with symptoms of dyspepsia.
Exclusion criteria
- Patients with decompensated heart failure.
- Patients with histories of gastric surgery.
- Patients with histories of previous endoscopy.
- Patients with histories of H. pylori infections.
Descriptive statistics
Initially descriptive statistics of the variables were analyzed using measures of central tendency and dispersion. Quantitative variables were described with averages and standard deviations, and qualitative variables were described with absolute frequencies and percentages.
Bivariate analysis
ANOVA (Analysis of Variance) was used for bivariate analysis to identify statistical differences between findings of gastric xanthomas and findings of gastric cancer or premalignant conditions.
RESULTS
This is a retrospective study which evaluated patients in the Gastroenterology service of the Hospital El Tunal of the National University of Colombia who had histologically confirmed diagnoses of gastric xanthomas from 2007 to 2012. These patients were compared with patients who were randomly selected from patients who were diagnosed with dyspeptic symptoms but were not diagnosed with xanthomas who were seen on the same day as patients who were endoscopically diagnosed with xanthomas.
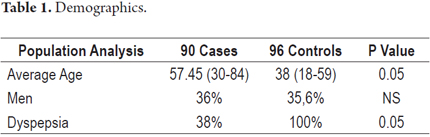
Two groups of patients were compared. The first consisted of 90 patients who had been endoscopically diagnosed with gastric xanthomas while the second (the control group) consisted of 96 patients who had no xanthomas (Table 1). The average age of patients with xanthomas was 57.4 years while the average age of patients without xanthomas was 38.3 years. Thirty-five percent of the patients with xanthomas were male while 35.6% of the control group were male (p = ns).
In total we found 90 patients with histologically confirmed diagnoses of gastric xanthomas during the 5 years of the study. During that period there were 27,200 upper gastrointestinal endoscopies performed which means the incidence of gastric xanthomas was 0.33%. Xanthomas were singular in 72% of the cases, the majority (53%) were located only in the antrum, thirty-two percent were located in the corpus, ten percent were located in the antrum, and 5% were located in the fundus.
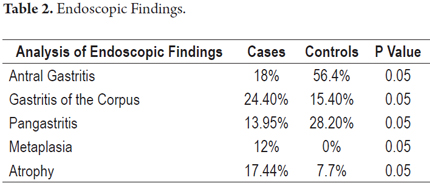
Endoscopic findings (Table 2) included greater frequency of antral gastritis in patients without gastric xanthomas (56.4% vs. 18%, p <0.05), but the opposite pattern was found among patients with gastritis of the corpus: 24.4% of the patients with gastric xanthomas had corporeal gastritis while only 15.4% of the patients without xanthomas had corporal gastritis (p <0.05). Intestinal metaplasia was suspected following endoscopy in 12% of the patients with xanthomas but not in any of the patients in the control group (0%). Atrophy of the gastric mucosa was suspected following endoscopy in 17.4% of the patients in Group 1 and in only 7.7% of those in group 2 (p <0.05).
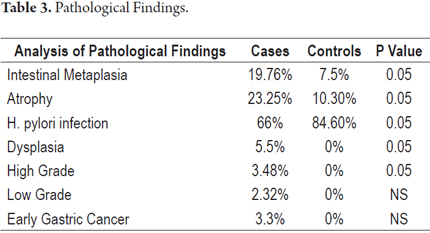
Histology (Table 3) detected greater frequencies of intestinal metaplasia (19.76% vs. 7.5% p: 0.05) and atrophy of any degree (23.2% vs. 10.3%, p <0.05) in patients with gastric xanthomas than in the control group. Among patients without xanthomas, no cases of dysplasia (0%) occurred, while in the group with xanthomas 5.5% of patients had dysplasia. Of these, two were low grade but three were high grade. H. pylori infections were found in 66% of Group I patients and in 85% of Group II patients.
Three patients in the group with xanthomas had early gastric cancer (3.3%), but none of the patients in the control did. In other words, six patients (6.6%) in the group with xanthomas had lesions that could be considered to be malignant if we add together the three cases of high-grade dysplasia and the three cases of early gastric cancer. None of the patients in the control group had any malignancies (0%, p = 0.05). Defining premalignant lesions as metaplasia, atrophy and low-grade dysplasia, we found that 45.5% of the group with xanthomas had premalignant lesions while only 17.8% of the control group did (p = 0.05). The three cases of early cancer were located in the distal third of the stomach, and all were treated endoscopically.
DISCUSSION
Gastric xanthomas were previously considered to be very rare lesions, but with the mass of endoscopic reports now available they are becoming increasingly common. Their incidence varies from 0.018% to 0.8% (4). In our work we found of 0.33% which is higher than that reported by Arévalo and Cerrillo which reported 26 patients (0.28%) over six years (5). The incidence we found is also higher than that reported by Petrov et al (6). In a study of 21,650 gastroscopies, they identified only four patients (0.018%) with gastric xanthomas. Similarly, Chen and colleagues (7) looked at 3,870 panendoscopies and found 30 cases of gastric xanthomas (0.88%). We believe that these discrepancies are mainly due to environmental variation as all xanthomas were found by endoscopy rather than biopsies. This condition is more common in women than in men and its incidence increases with age. This coincides our study in which 64% of the patients with xanthomas were female and over the age of 60.
The pathogenesis of gastric xanthomas is still uncertain, but in some cases chronic gastritis, H. pylori infections, diabetes mellitus and hyperlipidemia have been involved in the origin of this condition (8, 9). This indicates that inflammation contributes to the development of gastric xanthomas (10). In the work of Arévalo and his colleagues HP infections were found in 42.3% of the patients (5), but other researchers report up to 94% (11-13). Hori et al. found HP infections in 48% of a total of 145 patients (14). In our study, H. pylori infections were present in 66% of the cases and in 85% of the controls (p = 0.05). This may be explained by the facts that atrophy and metaplasia were more common in the group with xanthomas. H. pylori infections may have been resolved in these patients since, as has been pointed out in various studies of atrophy and cancer, glandular loss contributes to the disappearance of H. pylori infections once the damage has been caused (15, 16).
Xanthomas are most frequently located in the stomach, and less frequently located in the esophagus, duodenum, colon and rectum (17). Within the stomach they are most common in the antrum (67% to 69%) (3). In this study we found that 53% were located in the antrum and 32% in the corpus. In most reports in the literature xanthomas are singular as was the case in this study where we found singular xanthomas in 72% of the patients.
The mechanism that triggers the formation of gastric xanthomas and its clinical significance is not yet clear. Although since the first description of this entity in 1929 by Lubarsch and Borchardt (2) multiple hypotheses have been postulated, there are two theoretical groups of these efforts to explain the nature of gastric xanthomas.
Gastric xanthomas are secondary to altered lipid metabolism
A Korean study of 776 patients found that patients with gastric xanthomas had lipid profiles with lower HDL counts than those of controls (48.8 ± 12.3 vs. 62.9 ± 40.5, P = 0.028) and higher levels of LDL (112.9 ± 29.9 vs. 95.9 ± 22.4, P = 0.032) (18). However, the level of total serum cholesterol, triglycerides, and the presence of dyslipoproteinemia were unrelated to xanthomas in that study.
Gastric xanthomas are secondary to chronic lesions and scarring of the gastric mucosa
Repairing the damage caused by chronic inflammation releases lipid moieties that are consumed by histiocytes (foam cell formation). In addition, under conditions of intestinal metaplasia with bile reflux, increased intracellular and extracellular lipid transport has been found. These phenomena explain the close relationship between gastric xanthomas and atrophic gastritis, intestinal metaplasia, gastric ulcers, bile reflux and possibly gastric adenocarcinomas (19).
Our histological findings indicate that 19.7% of cases of gastric xanthoma were accompanied by intestinal metaplasia while only 7.5% of the controls had intestinal metaplasia (p = 0.05). This incidence is higher than reported by Chen et al. of 13.3% in 30 cases (7), but it is lower than that reported by Moreto et al. who found an incidence of intestinal metaplasia of 48% in 109 cases (20). Nevertheless, these studies did not have control groups. Gastric atrophy was found in 23.5% of our patients with xanthomas while it was found in only 10.3% of the control group. This is much lower than the figure reported by Naito et al. who found that 89% of 131 patients with gastric xanthoma had gastric atrophy (21). This difference is large and raises questions about whether the histological criteria in our study were the same as those used in the Japanese study for pathological diagnosis of gastric atrophy.
For the first time in a comparative study of patients with xanthomas, our study found that patients with xanthomas have a higher incidence of cancer and premalignant lesions than do other patients with dyspepsia. This is the most interesting finding from our study. Three patients (3.3%) in the group of xanthomas but none of the patients in the control had early gastric cancer. There were also three cases of high-grade dysplasia in the group with xanthomas which means that 6.6% of this group had malignant lesions (p = 0.05). This pattern had never been reported before this (only isolated cases have been published). Furthermore, if we consider premalignant conditions of metaplasia, atrophy and low-grade dysplasia 45.5% of the group with xanthomas had one of these conditions while only 7.8% of the control group did (p = 0.05).
However, it should be noted that this study has many limitations because it is a retrospective study that is susceptible to various biases that could explain the results. It should be especially noted that the age difference between the two groups was statistically significant. The differences in the prevalence of premalignant lesions and dysplasia could be due to the fact that the patients in the group with xanthomas was significantly older, and in this age range the prevalence of these lesions may be higher.
Nevertheless, our work suggests that whenever a patient is found to have xanthoma during an endoscopic examination, the endoscopist must be very alert to avoid overlooking the possibility of malignancy (cancer or dysplasia) or a premalignant condition (atrophy or metaplasia). In our opinion this being stricter about cleaning the gastric mucosa and more careful about observation of all areas of the stomach. Chromoendoscopy should be considered and gastric mapping should always be done. Nevertheless, it is important to point out that prospective studies and studies with better control groups that include larger numbers of patients are required to confirm these observations.
REFERENCES
1. Yi SY. Dyslipidemia and H. pylori in gastric xanthomatosis. World J Gastroenterol. 2007;13(34):4598-601. [ Links ]
2. Henke F, Lubarsch O, Uehlinger E. Handbuch der speziellen pathologischen Anatomie und Histologie. Berlin: Springer-Verlag; 1928. [ Links ]
3. Sataka M, Iida Y, Sakaki N, Odawara M, Nagatomi Y, Saito M. Clinical study on background mucosa of gastric xanthoma. Gastroenterol Endosc. 1982;24:739-44. [ Links ]
4. Gursoy S, Yurci A, Torun E, Soyuer I, Guven K, Ozbakir O, et al. An uncommon lesion: gastric xanthelasma. Turk J Gastroenterol. 2005;16(3):167-70. [ Links ]
5. Bartolini S. Xantomatosi gastrica circoscritta. Sperimentale Arch Biol. 1936;90:423-49. [ Links ]
6. Petrov S, Churtchev J, Mitova R, Boyanova L, Tarassov M. Xanthoma of the stomach-some morphometrical peculiarities and scanning electron microscopy. Hepatogastroenterology. 1999;46(26):1220-2. [ Links ]
7. Chen YS, Lin JB, Dai KS, Deng BX, Xu LZ, Lin CD, et al. Gastric xanthelasma. Chin Med J (Engl). 1989;102(8):639-43. [ Links ]
8. Isomoto H, Mizuta Y, Inoue K, Matsuo T, Hayakawa T, Miyazaki M, et al. A close relationship between Helicobacter pylori infection and gastric xanthoma. Scand J Gastroenterol. 1999;34:346-52. [ Links ]
9. Kubosawa H, Yano K, Oda K, Shiobara M, Ando K, Nunomura M, et al. Xanthogranulomatous gastritis with pseudosarcomatous changes. Pathol Int. 2007;57:291-5. [ Links ]
10. Aikawa M, Ishii T, Nonaka K, Nakao M, Ishikawa K, Arai S, et al. A case of gastric xanthogranuloma associated with early gastric cancer. Nippon Shokakibyo Gakkai Zasshi. 2009;106:1610-5. [ Links ]
11. Gencosmanoglu R, Sen Oran E, Kurtkaya Yapicier O, Tozun N. Xanthelasmas of the upper gastrointestinal tract. J Gastroenterol. 2004;39(3):215-9. [ Links ]
12. Kametani S. Xanthoma of the stomach. Gastroenterol Endosc. 1963;5:34-41. [ Links ]
13. Stolte M, Meining A. The updated Sydney system: classification and grading of gastritis as the basis of diagnosis and treatment. Can J Gastroenterol. 2001;15:591-8. [ Links ]
14. Hori S, Tsutsumi Y. Helicobacter pylori infection in gastric xanthomas: immunohistochemical analysis of 145 lesions. Pathol Int. 1996;46(8):589-93. [ Links ]
15. Dixon MF, Genta RM, Yardley JH, Correa P. Classification and grading of gastritis. The updated Sydney System. International Workshop on the Histopathology of Gastritis, Houston 1994. Am J Surg Pathol. 1996;20:1161-81. [ Links ]
16. Kimura K, Hiramoto T, Buncher R. Gastric xanthelasmas. Arch Pathol. 1969;87:110-7. [ Links ]
17. Morais DJ, Yamanaka A, Zeitune JM, Andreollo NA. Gastric polyps: a retrospective analysis of 26,000 digestive endoscopies. Arq Gastroenterol. 2007;44(1):14-7. [ Links ]
18. Yi SY. Dyslipidemia and H pylori in gastric xanthomatosis. World J Gastroenterol. 2007;13(4):4598-601. [ Links ]
19. Vimala R, Ananthalakshmi V, Murthy M, Shankar TR, Jayanthi V. Xanthelasma of esophagus and stomach. Indian J Gastroenterol. 2000;19(3):135. [ Links ]
20. Moreno Muro M, Coca Menchero S, Martos Peregrin JA, Gutiérrez Pérez JA. Xantelasmas gástricos: Aportación de dos casos y revisión de la literatura. Rev Esp Enf Ap Digest. 1979;56(4):369-71. [ Links ]
21. Naito M, Miura S, Funaki C. Gastric xanthomas in the elderly. Nippon Ronen Igakkai Zassshi. 1991;28:683-7. [ Links ]











 texto em
texto em