1. Background
Breakthroughs in telecommunication technologies have allowed the creation of new services, such as telemedicine [1]. Telemedicine is a health service in which information is remotely exchanged between a medical specialist and a patient for the awareness, prevention, diagnosis, and treatment of and rehabilitation from diseases using information and communication technologies that promote access to and opportunity to receive services by populations facing limited supply of and/or access to such services in their geographical area (i.e., the geographically vulnerable population) [2,3]. Remote clinical care has been performed in both teleassisted [4-7] and teleoperated manners [8-11]. The term “teleassisted” refers to a visual or over-the-phone telemonitoring system by which the therapy processes are specified and that works as a guide for treating of the patient [12]. The term “teleoperated” describes a system that allows long-distance human-device interaction to be controlled and operated remotely through a master device [13,14].
Due to the novelty of the telemedicine processes, information systems (ISs) are typically implemented to guarantee the efficiency of the remotely generated information flows during the patient care process. In the health sector, an IS consists of a set of elements that interact with one another to collect, store, manage and transfer a large amount of information obtained from the clinical processes performed in a health center [15]. These systems are a key factor for improving the efficacy of care processes because they provide fast and complete access to information [16].
Different authors have developed ISs for different clinical domains. Teixeira et al. [17] developed a web-based IS for the comprehensive care of hemophilic patients via user-centered engineering processes. Eguskiza A. et al. [18] created a generic methodology for developing ISs for the patient screening process for diabetic retinopathy in the Health Service of Navarro - Osasunbidea Service in Spain. Regarding previous ISs implemented in teleassisted or teleoperated processes, only a few studies are available. Castellano N. et al. [1] designed an IS for telemonitoring patients during transportation in an ambulance, which was coordinated though a portable system implemented by reference hospitals in Spain.
The limited number of studies on ISs implemented for telemedicine processes could be due to the fact that this technology was developed only a few years ago but has become very important in countries with insufficient health coverage for their populations.
Given the benefits of telemedicine for patient health and the importance of well-structured telemedicine systems, this study presents the development of an IS for the web-based teleoperated care of patients with mild knee injuries in geographically vulnerable zones. The aim of this work was to facilitate the construction of a set of technical, clinical, economic and social indicators for the evaluation and follow-up of the teleoperated rehabilitation system.
This report is organized as follows: The materials and methods considered for the development of the IS are described in Section 2. The results of the IS development process are presented in section 3. The methodology and results are discussed in section 4, and finally, conclusions are drawn in section 5.
2. Materials and methods
2.1. Study context
The prototype was developed by an interdisciplinary group formed by two physiotherapists, one industrial designer, one electronics engineer, one systems engineer, one industrial engineer and one statistician. The prototype's mechanical structure and the requirements related to the functionality of the machine to meet the needs of the population with physical disability and poor access to the health system, were defined by the multidisciplinary group as a whole. Then the design methodology was defined focusing on the development of a modular device and an architecture that integrated the required computer, electronic and mechanical.
First of all, the by physiotherapists defined the functional parameters according to the protocols of active and passive therapy in the knee joint. Subsequently, the industrial designer created the interaction with the user, through the hardware-software interfaces, the mechanical engineers participated in the verification and validation of the mechanical structure of the rehabilitation devices and the electronic engineer installed the control structure in the electronic components and conditioned the power system according to the requirements of the hardware components. The systems engineer managed the database, software interfaces; and the computational applications of the distributed system.
The IS was developed to evaluate the process of teleoperated rehabilitation care for patients with mild knee injuries in the physiotherapy sector of the ESE Ladera Health Network in Cali, Colombia. This network consists of ten and six centers distributed in rural and urban zones, respectively [19]. The care process is directed to patients with minor knee injuries because the people living in the rural areas of Cali are frequently affected because of the geographical conditions in these areas and their daily activities.
At ESE Ladera, the rehabilitation process is performed with a teleoperated assistive functional prototype for the knee joint (Fig. 1), which is controlled by a computer that adjusts the therapy protocols relating to the speed, strength and position at which the prototype performs the therapeutic routines in two types of movements: passive and active. Because the prototype is multifunctional, the developed IS is applicable to all joints treated by the device (i.e., shoulders, hips, knees and elbows). The prototype addressed in this work is located in a rural center, where the facilities have been adapted to receive patients and perform the therapy with the help of an assistant. In the urban zone, a specialist is in charge of determining the therapy routine for the patient and performing the rehabilitation process. The guidelines to follow in each therapy are defined by the specialist, meeting the requirements of the conventional physical therapy protocols.
2.2. Development of the IS
In developing the IS, the care processes implemented before and during the patient rehabilitation therapy were considered. Flowcharts for the prototype, assistant and specialist roles were used, in addition to the flow chart of the care process previously established by ESE Ladera. The data inputs of the system; the required materials; human and technological capital; technical, mechanical and economic data; and the data outputs of clinical and social information were also determined. These aspects are presented in this section.
2.2.1. Identification of the needs for teleoperated therapy
The design of the IS focused primarily on characterizing the data flowcharts of the processes and roles of the patient, assistant, specialist and assistive device in the care process. Furthermore, because part of the rehabilitation process for each patient is performed with the device, the development of the IS focused on ensuring the safety of the patient during the care process and constantly verifying that the elements involved in the process were working properly. The IS was intended to generate physical and virtual records of possible incidents that could affect the correct operation of the teleoperated process and to report the respective corrections and data associated with the evaluation of the various components of the teleoperated system. The elements, records and components considered in the development of the IS are presented below.
2.2.2. Elements involved in the teleoperated therapy process
The tangible and intangible elements involved in the teleoperated rehabilitation process were as follows:
Teleoperated assistive device: This prototype was designed by a group of engineers with differente specialties for knee rehabilitation. A computer establishes the duration of the therapy (from 1- 240 min), the speed (from 30 to 150 °/min), maximum extension/maximum flexion (from -10 to 140°) and the duration of the movement change delay (from 0 to 30 s).
-
The assistant interface allows searching the clinical history (patient identification number); reviewing the number of therapy sessions performed by the patient, the type of injury and the affected joint; determining whether the machine and the patient are in optimal condition to start the therapy session; and, in the case of an incident, reporting to the specialist and stopping the operation of the device.
The specialist interface is a computational medium that allows visualizing the clinical history of the patient who will start the therapy session, entering the physical parameters of the therapy protocol to be performed; and initializing and ending of the therapy in its geographical location (i.e., stopping the assistive device).
Usability and interoperability were used with the user in order to achieve an intuitive interaction between the user and the system, minimizing the risks due to poor operation of the teleoperation system. This interface has a visual output that records observations made by the assistant about the patient, indicates whether the assistant wishes to accept the therapy protocol and provides information about its development. At the end of this process, the specialist saves the information about the therapy protocol performed, and the patient’s clinical history is automatically updated.
The specialist can make decisions regarding the patient's treatment with the help of the patient information recorded and transferred through the teleoperated equipment and the direct observation of the patient through the video camera. Moreover, there is a permanent communication between the specialist and the assistant. In the same way, the system keeps the information of each care, so it is possible to make a better to keep track of to the patient.
The two interfaces were created in the web service programming environment of the Microsoft Visual Studio free edition, and the clinical history of the patient was structured in a SQL database. The interface and the web service are located on a remote server.
Internet: The communication between the two centers occurs through an interface via the internet, which requires a connection of at least 2 MB and a standard computer in each center.
2.2.3. Physical and virtual records
To verify the correct functioning of the elements involved in the teleoperated system, a technical mechanical checklist and an incident recording form were created. A patient satisfaction survey about the teleoperated system was also developed. The relevant variables involved in the assessment of the teleoperated system were identified in a literature review and based on the knowledge of a team of mechanical engineering, industrial design and industrial engineering and statistics experts from Univalle as well as physical therapists from the ESE Ladera. The development and application of these forms are detailed below:
Technical mechanical operation checklist: This checklist is a tool that functions as a guide for checking the correct operation of each part of the teleoperated device, interfaces and internet. In the rural centers, the assistant should go over the checklist before and during the performance of the therapy. This checklist identified the possible failures of the elements in the teleoperated system.
Incident recording form: This form is completed by the assistant to notify the specialist about the occurrence of any technical mechanical failure or failure attributed to the patient before and during the performance of the therapy. This form also includes the record of the corrective action performed to resolve the incident, the result obtained after the application of the corrective action and the possibility of continuing the therapy.
Satisfaction survey: This survey is administered by the assistant to the patient once all therapy sessions are completed. It is intended to determine the acceptance level of the new technology and the level of satisfaction with the teleoperated rehabilitation service received.
Therapeutic compliance form: This form is filled in by the assistant monitoring the patients and is used to record all patients who have completed the therapy satisfactorily, those who completed it with little improvement and those who did not complete all the assigned therapy sessions.
2.3. Components of the IS
The development of the IS involved the desing of a management indicator system for the comprehensive evaluation of the care system in terms of four components: technical mechanical, clinical, economic and social.
2.3.1. Technical mechanical component
This component includes all aspects related to mechanical, electronic and systems engineering and the industrial design characteristics of the teleoperated system. The information about this component should be used to evaluate the operational characteristics of the teleoperated system from the technical perspective, to monitor the system and to make decisions regarding preventive maintenance. The information for the evaluation of this component is sourced from the technical mechanical operation checklist and the incident recording form.
2.3.2. Clinical or rehabilitation component
This component has two subcomponents:
Efficacy of intervention. The aim of this evaluation is to compare the initial clinical parameters upon the patient’s arrival to the values after performing all therapy sessions assigned in the therapeutic rehabilitation process. The initial physical parameters are used to configure the assistive device, specify the initial therapy, angles of movement and speed levels initially tolerated by the patient and compare them with those achieved by the patient once the teleoperated rehabilitation process is completed.
Evaluation of patient compliance with the rehabilitation process. To evaluate the therapeutic compliance, the patient care records for the assigned therapy sessions and their level of improvement are used. These forms are filled by the nurse assistant and reflect the numbers of patients who have satisfactorily completed the therapy sessions, those who completed them with little improvement and those who failed to complete all the assigned therapy sessions.
2.3.3. Economic component
To analyze this component, a bibliography search was done to explore costing studies applied to health care systems. Based on the project requirements, the absorption costing system was considered. To this end, the cost of the physical therapy service using the new (teleoperated) system was estimated according to the cost structure of the ESE Ladera Health Network. In this model, the direct costs are related to inputs and material, labor, operations and maintenance costs. The indirect costs are associated with the service provided, which comprise payments for public services and the salaries of the administrative staff.
2.3.4. Social component
This component analyzes the tangible and intangible social benefits obtained by implementing the teleoperated rehabilitation system. This component indicates the extent to which the implementation of the teleoperated system benefits the patients in terms of facilitating access to the service and improving the opportunity for receiving care. It also reflects the level of patient satisfaction with the teleoperated physical rehabilitation process and the level of acceptance of the new technology. The information for evaluating this component is based on the results of the satisfaction survey.
3. Results
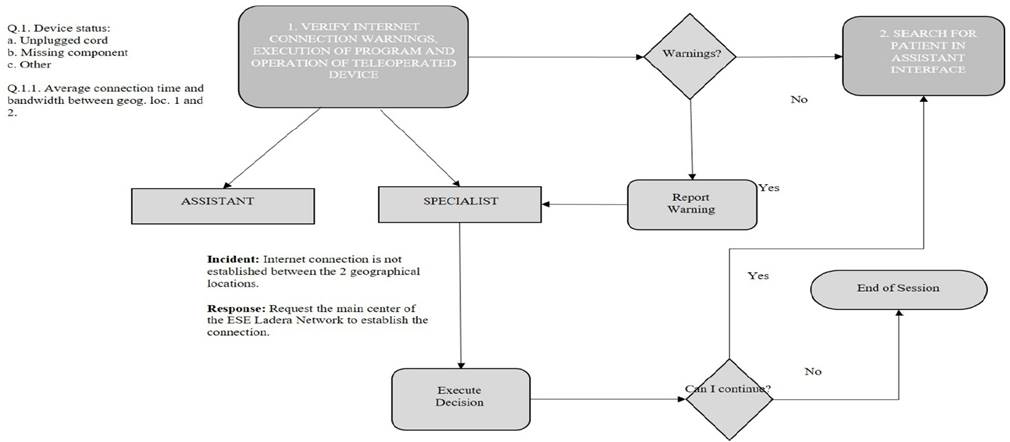
Considering the various components, elements and records listed in the methodology, the IS was based on the four primary activities: to review internet connection warnings, execute the program and the operation of the teleoperated machine; register patients in the assistant interface; log into the specialist interface; and initialize teleoperated therapy (Fig. 2).
The first activity establishes the internet communication between the two geographical locations. Then, via interface, the assistant (remotely located) registers the patient with his or her identification number, searches his or her clinical history and informs the specialist (local), about the therapy session that is about to begin. Through the interface, the specialist consults the clinical history of the patient and assigns the therapy routine. This information is updated in the assistant interface, and the assistant then informs the patient about the rehabilitation process that will be performed. Then, the patient decides whether to accept the therapy process. If accepted, the therapy session starts; otherwise, the therapy session is canceled.
In the IS, the communication is synchronous; i.e., the patient and assistant function as transmitters and the specialist as the receiver to coordinate their activities during a therapy session. The processes involved in these activities are specified below.
3.1. Information system
3.1.1. Verify internet connection warnings, program execution and rehabilitation machine operation
In this process, the internet access conditions and interfaces in both centers and the access to the machine in the rural center are verified (Fig. 3). The verification of the elements of the rehabilitation system is performed to ensure proper functioning so that when patient care is provided, all the components are in perfect condition and able to perform the therapy safely.
Source: The authors
Figure 3 Data flow diagram Level 1: Revision of internet connection warnings, execution of the program and rehabilitation device operating prior to initiation of therapy
For this verification, a checklist is used, which asks the assistant to verify the following:
The status of the machine before starting the therapy: A record should be created reflecting whether the technical assistive device is in good condition and whether any unplugged cord, missing component or other factor could affect proper operation (Question 1); and
The average internet connection time between the local point and the remote point (Question 1.1).
In the absence of warnings during verification, the registration of the patient is performed through the assistant interface. If warnings are found, the assistant should report them to the specialist through the Incident Reporting Form and include the following information:
The name of the specialist to whom the incident is being reported;
The corrective action implemented;
Whether the incident was resolved by the corrective action implemented; and
The possibility of starting the therapy session.
If the corrective measure resolved the problem, the patient is then registered through the assistant interface; otherwise, the session is ended, and the teleoperated therapy will not be performed until the incident is resolved.
3.1.2. Register the patient in the assistant interface
After receiving confirmation of the proper operation of the elements in the teleoperated system, the assistant in the rural center logs in to the assistant interface by entering his or her user code and password and then uses the patient identification number to search for his or her clinical history. The assistant interface displays the patient’s data, including his or her name, surname, gender, age, occupation, home address, order number, injury type, and affected side. The assistant must verify the patient’s weight because the maximum capacity of the device is 130 kg and evaluate the patient’s cognitive state to ensure, among other things, that the patient is not intoxicated. This information is then used to update the clinical history of the patient (Fig. 4).
3.1.3. Log into the specialist interface
After identifying the patient in the rural center, the specialist located in the urban center logs into the specialist interface entering his or her user code and password. The patient’s clinical data recorded in the rural center are automatically downloaded into the specialist´s interface environment. The specialist reviews the clinical history of the patient, the number of therapy sessions performed, and the treated injury or pathology. Once this review is complete, the specialist approves or rejects the therapy session, depending on the patient’s injury because not all pathologies can be treated remotely. Next, the specialist updates the clinical parameters used in the current session (i.e., the movement, speed, position, strength and number of series).
Through the interface, the assistant reviews the therapy protocol assigned by the specialist and proceeds to explain the type of therapy to be performed to the patient. If the patient is willing to accept this therapy, he or she must sign the legal informed consent document. If the patient does not accept the therapy, the therapy session is ended, the clinical history is updated, and the patient is referred for consultation regarding conventional therapy (Fig. 5).

Source: The authors
Figure 5 Data flow diagram Level 3: Arrival of therapy request at urban center. The Expert logs into the interface, approves the session and sends the clinical parameters of the therapy
When the patient accepts the teleoperated therapy protocol, the assistant notifies the specialist via the interface.
3.1.4. Initiate therapy with assistive device
After the teleoperated therapy is accepted by the patient, the assistant follows the machine initialization protocol (Fig. 6) and checks the operational conditions with the help of the checklist, answering the following questions:
¿Was the initialization protocol followed? (Question 2)
¿Are the sensors operative? (Question 3)
In the case of sensor failure, ¿which sensor is inoperative? (Question 3.1)
In the case of sensor failure, ¿is the safety system responding? (Question 4)
¿Are the motors working? (Question 5)
In the case of motor failure, ¿is the safety system responding? (Question 5.1)

Source: The authors
Figure 6 Data flow diagram Level 4A: Execution of initialization protocol of assist device (MACH), transmission clinical parameters and receipt of protocol.
If problems arise with the initialization protocol or initial auto diagnostic, the assistant should check to determine whether the device stops moving and whether the safety system is activated (Question 6.2). Additionally, they should verify that the device sounds the safety alarm and that the error is reported on the screen (Question 8).
Next, the assistant should complete the incident form by recording the type of incident, the name of the specialist to whom it is being reported, the corrective action, and whether the problem was resolved.
After implementing the corrective action and following the initialization protocol, the assistant should check the following: If the initialization protocol was followed, did the device return to its neutral position? (Question 6).
Through the interface, the specialist sends the therapy protocol, and the assistant, through the respective interface, then verifies and transfers the clinical parameters to the device. Finally, the assistant should confirm the following: Was communication established between the device and the computer? (Question 7) That is, are the therapy parameters shown on the machine’s screen and are they correct? (Question 10).
One last activity that should be performed by the assistant before starting the therapy session is to verify the functioning of the therapy mode depending on the protocol established by the specialist. Additionally, regarding the activation of the passive therapy mode, the following questions should be answered: Is the motor engaged and the load simulator disengaged? (Question 11) Upon activating the active therapy mode, is the motor disengaged and the load simulator engaged? (Question 11.1)(Fig. 7).

Source: The authors
Figure 7 Data flow diagram Level 4B: Initialization of teleoperated therapy and execution of configuration (initial physical parameters tolerated by the patient).
At this point, the assistive device is ready and in optimal condition to start operating. The patient has accepted the therapy protocol, and the assistant is ready to start the therapy session once the initialization order issued by the specialist arrives (Question 11.2). The assistive device performs the initial specification or evaluation to establish the range of motion, speed and force tolerated by the patient, and the rehabilitation process begins. These specifications are recorded in the patient’s clinical history.
During the execution of the active or passive phase, any of the following incidents may occur (Fig. 8):
Prolonged internet outage;
Power outage;
Patient sickness;
Sensor failure;
Actuator failure;
Device-computer communication failure; or
Motor failure.
In any of these cases, the assistant should report the incident to the specialist and verify whether the machine returns to its neutral position (Question 20).

Source: The authors
Figure 8 Data flow diagram Level 4C: Execution of first therapy cycle (active or passive) and monitoring of incidents during therapy session.
With the information obtained from each of the activity flowcharts in the IS, a set of indicators for with the comprehensive evaluation of the teleoperated rehabilitation system could be developed.
4. Discussion
Given the increasing use of modern technologies, such as telemedicine, in various clinical processes, the implementation of ISs has become necessary to generate, store and transfer the large amounts of information generated during these processes. Thus, it is important for these ISs to be properly designed and modeled. An IS for care processes should feature user-centered design to improve the effectiveness of the processes and provide quality health care services while ensuring the safety of the user.
Proper IS design is relevant because it facilitates better control and execution of the clinical care process, helps to identify human or technical error and the excessive use of resources, and contributes to improving the follow-up of patients’ therapeutic processes. In this study, an IS was designed in cooperation with a multidisciplinary team of experts to evaluate the viability of implementing a small-scale teleoperated care system to benefit users in need of physical rehabilitation care who live in zones where accessing health services is difficult.
It is important to emphasize that the IS can be used as input for the evaluation of the clinical processes. Another advantage is that the developed IS is applicable to all joints treated by the device (i.e., shoulders, hips, knees and elbows). Therefore, for subsequent studies during the implementation phase of the teleoperated device in its various modes, the IS could be used with few changes. One of the limiting factors for the efficient use of the developed IS may be the level of compatibility of the assistant and specialist with both the teleoperated assistive device and the interface; however, clear instructions have been developed for the users of this system.
The results of this evaluation can serve as the basis for implementing this system in other contexts in Colombia where geographical vulnerability and economic conditions also pose obstacles to accessing physical rehabilitation services. These contexts require examination of the setup conditions of the assistive device and the conditions of the internet connection and the interface. If acceptable working conditions can be achieved, variations would not substantially affect the model of clinical processes considered for the design of the IS or the capacity and efficiency of information management.
5. Conclusions
A web-based IS was developed to model the care processes of patients with mild knee injuries provided through a teleoperated system and to generate information for the comprehensive evaluation of this system. The designed IS allows the assistant and specialist to perform the patient care process more efficiently while evaluating the operation of the elements involved in the teleoperated system and managing the information in a controlled manner for each therapy session. Because the two centers communicate through the interface and internet, ESE Ladera can take advantage of time and cost savings and provide benefits for patients who live in areas in which accessing physical rehabilitation processes is difficult. The information provided by the IS through the forms implemented in the data flow was used to create indicators for the evaluation of the technical mechanical, clinical and social components of the teleoperated system. Based on this study, it can be concluded that the initial design of ISs for implementation in the health sector is very complex, but when ISs are developed with the appropriate focus, they can improve the quality of the processes and, thereby, increase their extension and usability in other clinical scenarios.


















