Introduction
Obstructive sleep apnea (OSA) is a common disease that is associated with cardiovascular disorders such as systemic arterial hypertension,1 mainly resistant arterial hypertension,2,3 arrhythmias such as atrial fibrillation,4 and cerebrovascular accident,5,6 all of which increase mortality rates.7 CPAP (continuous positive airway pressure) is the most effective treatment for OSA, as it reduces the number of respiratory events (Apnea Hypopnea Index - AHI), daytime sleepiness,8 traffic accidents,9,10 and systemic blood pressure values;11 moreover, some evidence shows that its early use improves survival after a cerebrovascu-lar accident.12
Patients' adherence to CPAP is poor, and despite multiple interventions, it has not improved in recent years,13 making it a limiting factor for this treatment. A study in five Latin American countries showed that only 55.7% of patients diagnosed with OSA started CPAP and that only 47% of them were still using CPAP after one year.14 The reasons for poor adherence are varied and related to motivational and psychological reasons, perceived efficacy,15 and side effects caused by the mask or the pressure, which sometimes result in discontinuation of treatment.16 To date, the impact of sex on adherence is unknown, and most studies have not found evidence that it could be a predictor of good adherence.17,18
Many strategies such as education interventions, telemonitoring and behavioral therapies have been studied in patients who are about to start treatment; however, few studies focus on patients who have already started CPAP and are having problems to adapt. Therefore, the objective of the present study was to evaluate the impact of a standardized adaptation session (SAS) in short-term adherence to CPAP therapy in patients with OSA and to determine differences by sex.
Materials and methods
Study design and population study
A before-and-after single cohort study was conducted in patients over 18 years of age with an AHI ≥15/h who attended the pulmonology outpatient clinic of the Fundación Neumológica Colombiana (FNC), Bogotá D.C., Colombia, between 2015 and 2017 and were referred by the treating physician to a SAS in the sleep center of the same institution due to poor adherence to PAP, defined as <4 hours use in 70% of nights during the evaluated period. Each patient was scheduled to attend the SAS between 1 and 4 weeks after the physician deemed it necessary. Participants were recruited through convenience sampling and those who did not attend the follow-up visit or for whom complete data was not available were excluded. The final sample size was 40 patients.
Intervention
A SAS is part of the comprehensive care of sleep apnea patients at FNC and is aimed at patients who have difficulties with PAP use. It consists of an approximately 30-minute group discussion (5 patients per group with a relative) led by a physical therapist trained in sleep apnea and PAP therapy, who provides patients with information about obstructive sleep apnea, its treatment and complications, and also explains to them the benefits of PAP therapy and adherence to treatment, its side effects, and possible solutions. Also, during the SAS, patients ask questions and can exchange their experiences with other patients. Later, on the same day, each subject attends an individual session of approximately 30 minutes with their PAP equipment and mask, during which data on its usage are downloaded and problems encountered during this session are collected to be assessed.
Problems reported by the patients were divided into four groups and were classified according to the criteria used by the physical therapist to establish the main cause of non-adherence:
Mask and leaks: discomfort caused by the mask, including pressure sores, rash, incorrect mask size, mask in a bad condition, mouth leaks, and other leaks.
Humidifier: dryness in the upper airway (mouth, nose, or throat).
Device: not knowing the device and its use, intolerance to the pressure generated by the device, difficulty in exhalation, difficulty breathing due to pressure, and poor programming.
Education: lack of information regarding the use of the equipment or mask, unawareness of the consequences of the disease, benefits of using PAP, and no need for another intervention.
During the SAS, interventions aimed at solving the detected problems included changing the mask, modifying the parameters of the equipment or the level of humidification, and providing educational information on the use of PAP devices or the mask.
The hours of PAP device use and the percentage of days with >4 hours of use were downloaded from the device before and after the intervention to assess changes in the participants' adherence to PAP therapy.
Statistical analysis
Descriptive statistics were used for data analysis. The Kolmogorov-Smirnoff test was used to determine the distribution of data for continuous variables. Qualitative variables were expressed as proportions, while quantitative variables were expressed as means and standard deviations or as medians and interquartile ranges depending on data normality. Differences between men and women were estimated using the Student's t-test for continuous variables with normal distribution, the Mann-Whitney U test for variables with non-normal data, and the chi-square test for categorical variables. The paired samples t-test was used for the comparison of variables before and after the intervention. A significance level of p<0.05 was considered for all statistical tests. All statistical analyses were performed using the statistical software SPSS version 22.
Ethical considerations
The study followed the ethical principles for conducting biomedical research involving human subjects outlined by the Declaration of Helsinki,19 as well as the technical, scientific, and administrative standards for health research set forth in Resolution 8430 of 1993 of the Colombian Ministry of Health.20 Likewise, it was approved by the FNC Ethics Committee, as stated in Minutes 230 of June 3, 2017, and informed consent was obtained from all participants.
Results
There was not a predominant sex; in fact, 50% participants were women. The average age was 64.6±14.1 years, and all participants had moderate to severe sleep apnea (AHI: 44.5±19.0). The majority of patients used fixed CPAP (87.5%) and oronasal masks (70%).
All had attended an initial education session with the PAP equipment supplier, and the mean time of PAP device use prior to the adaptation session was 9.2±11.5 months.
The main issues described by the patients regarding the use of the PAP device were related to mask and leaks (65%), discomfort with the device (45%), and dry mouth (15%). The interventions that were carried out included the provision of educational information (65%), the replacement of the mask (30%), and the modification of the pressure parameters of the device (5%). There were no sex differences regarding apnea severity, type of mask or device, discomfort reported by patients, or interventions performed (Table 1).
Table 1 Baseline characteristics of patients and devices by sex.

SAS: standardized adaptation session; AHI: apnea hypopnea index; PAP: positive airway pressure; CPAP: continuous positive airway pressure; BPAP: bilevel positive airway pressure. Values presented as mean ± DE, median (P25 - P75), or N (%).
p=differences between men and women.
Source: Own elaboration.
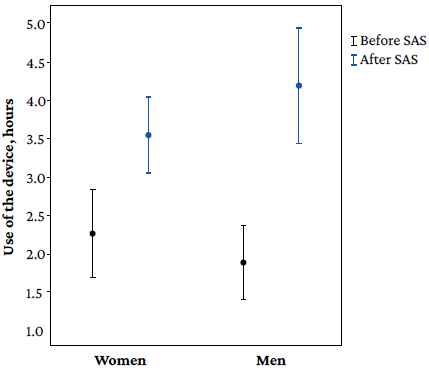
The intervention was evaluated on average 54 days after SAS was conducted. Following the intervention, a significant increase in PAP device use was observed in the whole cohort (1.8h, 95%CI: 1.3-2.3; p<0.001) and in the percentage of days of >4 hours use (35.6%, 95%CI: 26.0-45.3; p<0.001) (Table 2).
Table 2 Changes regarding the use of devices after the standardized adaptation session by sex.
| Total group | Women | Men | p | |
|---|---|---|---|---|
| n=40 | n=20 | n=20 | ||
| Differences in hours of use after SAS | 1.8 (95%CI: 1.3-2.3) * | 1.3 (95%CI: 0.6-1.9) | 2.3 (95%CI: 1.7-2.9) | 0.023 |
| Difference in % of use > 4 hours after SAS | 35.6 (95%CI: 26.0-45.3) * | 23.4 (95%CI: 12.5-34.3) | 47.8 (95%CI: 32.9-62.8) | 0.009 |
SAS: standardized adaptation session.
*p<0.001.
p=differences between men and women
Source: Own elaboration.
There was a significant improvement in the hours of use of the device in both men (p<0.001) and women (p=0.001), as well as in the percentage of days of use >4 hours in men (p<0.001) and women (p<0.001). However, the improvement in hours of use was greater in men (p=0.023), as well as the percentage of use >4 hours (p=0.029) after the SAS (Figure 1). There were no significant differences regarding the hours of PAP device use between participants with PAP device use for more than 6 months and those who had only used it for less than 6 months (p=0.627).
Discussion
The main finding of this study, conducted in patients with OSA and suboptimal PAP equipment use, was the significant improvement in the time of PAP device use after attending a standardized adaptation session aimed at solving the patients' adherence problems. Furthermore, it is worth noting that the improvement was significantly higher in men.
The greater effectiveness of the intervention in men compared to women is a remarkable finding, given that sex has not been described as a predictor of PAP adherence in many of the studies carried out to date. However, Joo et al.21 studied CPAP adherence in a group of more than 300 patients and found that, after adjusting for race, marital status and age, women had an OR=2.49 (95%CI: 1.39-4.46) for non-adherence to treatment.
The foregoing is consistent with our findings and those of Pelletier-Fleury et al.,22 who, in a study conducted in France in 163 patients with OSAS who had been prescribed with non-invasive CPAP therapy, found that factors related to non-adherence to this treatment were being female, having a body mass index ≤30 kg/m2, an Epworth Sleepiness Scale score <15, an AHI <30/hour, and a CPAP pressure >12 cm of water.
Furthermore, Guralnick et al.,23 in a study carried out with data on CPAP adherence of 104 patients with OSAS, found that adherence to CPAP was very poor (only 25% of patients used their CPAP devices more than 4.5/hour per night) and that factors associated with reduced CPAP usage (approximately 1 hour less use of the CPAP equipment) were being male, being African American, and having symptoms of depression.
On the other hand, Sin et al.,24 in a study conducted in 296 patients with OSA after 6 months of CPAP use, found that being female, increasing age and a decrease in the Epworth Scale score were associated with increased CPAP use. In Colombia, Benavides et al.25 found that, in a group of 133 patients with OSA, adherence to PAP was greater in women (77% in women vs. 64% in men).
It is known that the CPAP usage pattern is established during the first weeks of treatment, but some patients continue to use the device for less time than recommended for a long time. In this regard, 15% of the patients included in this study had used the device for more than 6 months, but no significant differences were found in their response to the intervention.
Most studies evaluating the effectiveness of adherence interventions have been conducted in patients who are going to start CPAP or have recently started it, but few have focused on late interventions. Ballard et al.26 evaluated a 2-phase intervention program in 204 patients with poor adherence to CPAP therapy after 118 days of being diagnosed with OSA. In Phase 1, they evaluated the barriers to CPAP use and then provided education and counselling about OSA and its treatment and made adjustments to the CPAP equipment or replaced the mask (after being fitted), which improved adherence in only 24% of the patients.
The most frequent intervention in the present study was simply providing educational information on how to use the PAP device and the benefits of PAP therapy, since it was found that the main problem causing poor adherence in many patients was a lack of information on how to properly use the equipment or not clearly understanding why they had been prescribed with this treatment. Both group and individual education interventions were conducted, bearing in mind that it is an essential part of the acceptance of any chronic treatment; nevertheless, not all education strategies studied have shown effectiveness in improving adherence.
La Piana et al.27 showed, in a study conducted in 202 patients with OSAS, that the use of an intensive education program at the beginning of treatment played an important role in adherence to CPAP treatment at 3 and 12 months, with a decrease in adherence at 2 years, suggesting the need for reinforcement. In turn, Dourado-Rueda et al.28 evaluated an education program conducted by a nurse, consisting of a talk and a video with information about sleep apnea and CPAP, which showed an improvement in CPAP compliance and in time of use at 90 days in the intervention group compared to the control group (71% vs. 56%, p=0.02; and 6.3±1.9 vs. 5.1±1.7 h/night, respectively, p=0.01). On the contrary, Guralnik et al.,29 in a study conducted in 212 patients with OSA (intervention group: 99; control group: 113) found that an educational video seen before the split-night polysomnography (PSG) did not increase CPAP adherence at 30 days compared to the group that received usual care (3.3 to 3.8 h/day vs 3.5 to 4.0 h/day of standard care).
Group education has the benefit of saving resources and time and allows to exchange experiences with similar patients. However, in the case of CPAP adherence, conflicting results have been reported. For example, Lettieri et al.,30 in a study conducted in 2 116 patients (1 032 received group education regarding OSA and CPAP, while 1 084 received individual education) found that, compared to the individual training strategy, group education (15 to 20 people) increased acceptance and adherence, and reduced the frequency of treatment abandonment in the first month.
Furthermore, Delanote et al.,31 in a study carried out in 100 CPAP-naïve patients with moderate to severe OSA, demonstrated that an individual education session combined with one hour of group education improved the time of use per night and reduced the dropout rate at 24 weeks of follow-up. However, according to Soares et al.,32 there were not significant differences in CPAP use at 6 months after performing the group education session.
The other part of the intervention in the present study was an individual session aimed at detecting problems or barriers hindering the use of the PAP equipment. These barriers are specific to each individual and each patient may have more than one reason for discontinuing the use of the PAP device. Most of the patients in this study used oronasal mask (87.5%), and the most frequent complaint was associated with the mask and leaks (65%), thus requiring adjustment or replacement. In this regard, it is known that proper mask selection (type and size) plays an important role in adherence and some studies have revealed that oronasal masks may relate to less use.
Concerning this, Borel et al.,33 in a study conducted in France in 2 311 patients with OSA, reported that the type of interface was associated with a higher risk of non-adherence to CPAP treatment, with the oronasal mask being the most associated with a higher risk of non-adherence (OR: 2.09; 95%CI: 1.67-2.60). On the other hand, in a double limb trial (face or nasal mask; four weeks each limb) conducted in 20 patients with obstructive sleep apnea/hypopnea syndrome, Mortimore et al.34 found that nightly compliance with CPAP therapy was higher when the nasal mask was used (mean: 5.3 vs. 4.3 hours/night) and that most of the patients (95%) stated that nasal masks were more comfortable than face masks (p<0.001). Likewise, Amado-Galeano et al.,35 in a study conducted in 109 patients receiving CPAP therapy (nasal mask only), reported that the main reason related to poor adherence was the inadequate use of the mask and that some interventions, such as education sessions, as well as some medical and surgical treatments resulted in improved CPAP tolerance.
In our study, problems associated with the device due to intolerance to pressure or difficulty in exhalation were reported in 45% of patients. Similarly, in a study carried out in United States in 140 patients with moderate to severe OSA, Aloia et al.36 found that more than 60% of the participants had problems with CPAP equipment at 6 months of treatment such as discomfort, congestion, or sensation of very high pressure, factors that could lead to the intermittent use of this therapy.
Although a significant improvement in the time of PAP device use was observed after the SAS in the present study, adherence in some participants remains below the recommended minimum,37 suggesting that side effects and mechanical barriers are not the only factors explaining poor adherence to CPAP therapy. Despite this, the results of the present study support the importance of knowing the difficulties of individual use, so carrying out specific interventions may impact adherence.
The main limitations of this study are the small sample size and the lack of a control group. In spite of this, the changes observed in the use of PAP devices were significant and positive. In addition, other aspects that may be related to poor adherence were not evaluated, such as psychological factors, marital status, or the presence of comorbidities.
The strengths of the study are that a standardized adaptation strategy was implemented and that the time of device use was objectively evaluated using the data recorded in them.
Conclusions
The SAS offered by the FNC, which includes education strategies and the identification and solution of obstacles hindering the use of PAP devices, significantly increased the hours of use and the percentage of days in which it was used more than 4 hours in the study population, particularly in men.