Introduction
Orotracheal intubation is a therapeutic procedure performed to save patients with respiratory failure,1-5 but it can lead to complications such as laryngeal lesions, respiratory infections (pneumonia), or even difficulties in withdrawing mechanical ventilation due to extubation failure.6-10 The latter is associated with increased days of hospital stay, increased costs of medical care, and the need for tracheostomy, as well as worse prognosis and higher mortality, which can reach up to 40%.1,8,10-12
Complications of orotracheal intubation include post-extubation laryngeal stridor, a condition that is not universally defined, but described in the literature as the development of inspiratory wheezing, grunting or whistling that requires medical intervention and occurs within the first 24 hours after extubation.13-16 Although all intubated patients develop laryngeal edema, only some of them show clinical manifestations or significant lesions. Thus, the incidence of laryngeal stridor is widely variable among studies and depends on the population studied, ranging from 1% to 26%.9,14
Laryngeal and muscular damage induced by orotracheal intubation may persist for weeks after extubation,17,18and ulceration of laryngeal commissures, laryngospasm, laryngeal edema, laryngeal nerve damage, and respiratory muscle atrophy have been described among the associated lesions.5,8-9,18 All of these abnormalities lead to a reduction in airway lumen caliber leading to the clinical manifestation of stridor; however, clinical studies only consider reductions ≥50% of airway lumen to be significant.9
Due to the frequency and severity of these complications, it is necessary to establish predictors in order to design strategies for their prevention and treatment. Therefore, the objective of the present study was to identify factors associated with early extubation failure (≤24 hours) and the development of post-extubation laryngeal stridor in adult patients on invasive mechanical ventilation (IMV).
Materials and methods
Study type, population, and sample
Case-control study conducted in a quaternary care center in Bogotá D.C., Colombia, between April 2019 and February 2020, using prospective data collection. The research derives from the thesis presented by one of the authors to obtain the degree of specialist in internal medicine at the Universidad Nacional de Colombia.19
The minimum sample size needed was estimated at 170 patients using the Kelsey and Fleiss formulas, considering a significance of 0.05 and a beta error of 0.2 with an incidence of extubation failure of 20% and a prevalence of exposure to a factor of interest in 30% of controls; the target OR was 3.0.
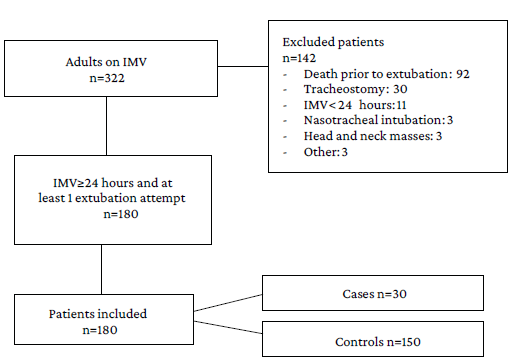
Consecutive sampling was used to recruit all patients over 18 years of age admitted to the intensive care unit (ICU) and receiving IMV (N=322). In order to obtain the final sample, the inclusion criteria were having at least 1 extubation attempt, and the exclusion criteria were death before attempting extubation, undergoing tracheostomy, requiring intubation for 24 hours or less, requiring nasotracheal intubation, having masses in the head and neck, and not having complete data during the follow-up period. Once these criteria were implemented, a final sample of 180 patients (30 cases and 150 controls) was obtained. The patients included in the study were identified prospectively and the detailed sample selection process is depicted in Figure 1.
Procedures
Once participants were identified, their clinical condition was monitored at least once every 24 hours until the end of their ICU stay or exclusion from the study.
Cases were defined as patients with extubation failure within the first 24 hours after the extubation attempt, while controls were defined as patients in whom successful extubation was achieved. On the other hand, the attending respiratory therapy group defined laryngeal stridor as the presence of inspiratory wheezing within the first 6 hours following the procedure. Tidal volume reductions >15% were considered positive and appropriate to extubate patients. Drager C300 and/or C500 mechanical ventilators (Dräger, Lubeck, Germany) were used.
Outcomes and definitions
The primary outcome was extubation failure, defined as the need for a new orotracheal intubation within the first 24 hours after extubation. The secondary outcome was the presence of post-extubation laryngeal stridor, defined as the presence of inspiratory gasping, grunting or wheezing requiring therapeutic interventions for mitigation13-16 noted in the physical examination performed by the attending respiratory therapy team within 6 hours after extubation. The variables of interest considered for all patients included were:
Sociodemographic and anthropometric variables: age, weight, height, and body mass index (BMI).
Relevant clinical variables: medical and surgical history; severity indices according to the Sequential Organ Failure Assessment Score (SOFA); presence of comorbidities such as cancer, chronic obstructive pulmonary disease (COPD), pneumonia, and acute respiratory distress syndrome (ARDS); laboratory test results (hemoglobin values, platelet counts, and creatinine); and 30-day mortality.
Variables related to airway manipulation: difficult intubation, negative inspiratory force (NIF), endotracheal tube number, Yang-Tobin index (also known as rapid shallow breathing index), cuff leak test, and tube cuff pressure.
Furthermore, information on the presence of prolonged mechanical ventilation (more than 7 days) was collected, and in the cases in which the cuff leak test was positive, data on the measurement of exhaled volume before and after deflation of the tube cuff were recorded. Changes >20% of the initial value were considered positive.
Statistical analysis
Collected data were tabulated in a Microsoft Excel 2016 spreadsheet, which was entered into the STATA 14.0 statistical software to process and analyze the information.
Data were analyzed descriptively using absolute frequencies and percentages for qualitative variables, and means, medians and standard deviations for quantitative variables. Differences between cases and controls were determined using Student's t-test for quantitative variables, and Chi-square or Fisher's exact tests for qualitative variables, with a significance level of p<0.05, which was determined using a two-tailed test.
Likewise, a multivariate analysis was performed by constructing an unconditional logistic regression model to obtain the measure of association or odds ratio (OR) (considering a target OR of 3.0), with its respective 95% confidence interval (95%CI), between the exposure (extubation attempt) and the primary and secondary outcomes adjusted for the presence of confounding variables. In this logistic regression model, the variables included in the model were selected using the Hosmer-Lemeshow test.20
The algebraic expression of the initial model included all the variables of interest, and the final model was obtained through a backward modeling strategy. The variables that had an association p<0.20 (Wald test) in the bivariate analysis were included in the unconditional logistic regression model. Finally, the presence of confounding was tested through variations in the magnitude of the OR, for which variations with a change in the original value of at least 20% were considered significant. Significance level for comparing the models by removing variables was set at p<0.01. Tables reporting the results included the OR value, standard error of measurement, hypothesis test results with p value, and 95%CIs.
Ethical considerations
The study, which was approved by the ethics committee of the Faculty of Medicine of the Universidad Nacional de Colombia pursuant to Minutes No. 020-334-18 of December 14, 2018, took into account the ethical principles for research involving human subjects established in the Declaration of Helsinki21 and the provisions on health research contained in Resolution 8430 of 1993 of the Colombian Ministry of Health.22 In addition, participants' data were protected and anonymized and used exclusively for this research, and informed consent was obtained from all participants.
Results
Most (52.77%) patients were men and the mean age, BMI, and days on IMV were 58.5 years (SD±19.7), 25.7 kg/m2 (SD±5.7), and 3.8 days (SD±3.6), respectively. The most relevant comorbidities were cancer in 37 patients (20.55%) and COPD in 20 patients (11.11%). The most common causes of admission to the ICU were respiratory conditions (23.18%), followed by neurological disorders (23.18%), and nonpulmonary infections (18.14%). On admission to the ICU, sepsis was reported in 69 patients (38.33%) and pneumonia in 48 (26.66%). The average hemoglobin and platelet counts on admission were within normal ranges; however, there were elevated average creatinine levels [1.78 mg/dL (SD±3.2)], average SOFA score [5.9 (SD±2.99)], and overall mortality (16.66%). The characteristics of the participants are presented in detail in Table 1.
Table 1 Baseline demographic, anthropometric, and clinical characteristics of the sample.
| Variable | Cases (n=30) | Controls (n=150) | Total (n=180) | p- value * | |
|---|---|---|---|---|---|
| Age (years±SD) | 54.4 (17.9) | 59.2 (20.0) | 58.4 (19.7) | 0.22 | |
| Male sex (%) | 16 (53.33) | 79 (52.66) | 95 (52.77) | 0.95 | |
| Weight (kg±SD) | 69.8 (15.8) | 69.8 (14.5) | 69.8 (14.7) | 0.99 | |
| Body mass index (kg/m2±SD) | 25.3 (5.6) | 25.8 (5.2) | 25.7 (5.3) | 0.62 | |
| Comorbidities | Cancer (%) | 9 (30.00) | 28 (18.66) | 37 (20.55) | 0.16 |
| Chronic obstructive pulmonary disease (%) | 3 (10.00) | 17 (11.33) | 20 (11.11) | 0.83 | |
| Pneumonia (%) | 13 (43.33) | 35 (23.33) | 48 (26.67) | 0.02 | |
| Sepsis (%) | 16 (53.33) | 53 (35.53) | 69 (38.33) | 0.06 | |
| Adult acute respiratory distress syndrome (%) | 3 (10.00) | 5 (3.33) | 8 (4.44) | 0.10 | |
| Hemoglobin (g/dL±SD) | 11.21 (2.7) | 12.15 (3.0) | 12.00 (3.0) | 0.12 | |
| Platelets (10A3/uL± SD) | 221 (160.2) | 270 (137.7) | 262 (142.0) | 0.08 | |
| Creatinine (mg/dl± SD) | 1.28 (0.66) | 1.87 (3.50) | 1.78 (3.21) | 0.36 | |
| Days on invasive mechanical ventilation (±SD) | 4.86 (4.84) | 3.61 (3.31) | 3.82 (3.62) | 0.08 | |
| Difficult airway (%) | 1 (3.33) | 12 (8.00) | 13 (7.22) | 0.36 | |
| Cuff pressure (cm H2O±SD) | 22.57 (8.0) | 22.67 (8.6) | 22.65 (8.5) | 0.95 | |
| Prior intubation (%) | 8 (26.66) | 20 (13.33) | 28 (15.55) | 0.006 | |
| Self-extubation (%) | 3 (10.00) | 10 (6.66) | 13 (7.22) | 0.57 | |
| Yang-Tobin index (breaths/liter/minute) | 42.03 (13.2) | 40.11 (18.3) | 40.41 (17.6) | 0.61 | |
| Cuff leak test (%±SD) | 38.53 (25.0) | 40.4 (36.3) | 40.09 (25.1) | 0.71 | |
| SOFA score (mean±SD) | 5.93 (3.9) | 5.84 (2.7) | 5.85 (2.9) | 0.88 | |
| 30-day mortality (%) | 8 (26.66) | 22 (14.66) | 30 (16.66) | 0.10 | |
SOFA: sequential organ failure assessment; SD: standard deviation.
* The comparison p-value considered was <0.05.
Source: Own elaboration.
The percentage of men in the case group was 53.33% and in the control group was 52.66%, and the average age was 54.5 years in the cases and 59.3 years in the controls (p=0.222). The frequency of COPD between the groups was also very similar: 10.00% in cases and 11.33% in controls (p=0.832). However, there was a trend towards a higher frequency of pneumonia (43.33%), sepsis (53.3%), and cancer (30.0%) among cases compared to controls (23.33%, 35.53%, and 18.66%, respectively).
Regarding laboratory tests, no significant differences were found between hemoglobin or platelet counts, but there was a trend toward a lower creatinine level among cases: 1.28 mg/dL vs. 1.87 mg/dL (p=0.362). Cases showed a trend towards more days on mechanical ventilation: 4.86 vs. 3.61 (p=0.082), and a higher frequency of history of intubation in the last year: 26.66% vs. 13.33% (p=0.006).
There were no significant differences between the groups with respect to the frequency of unscheduled extubation, mean tube cuff pressure, or history of difficult airway. The SOFA score in the first 24 hours was 5.93 (SD±3.98) among cases and 5.84 (SD±2.77) among controls (p=0.877). There was a trend toward higher mortality among the cases: 26.66% vs. 14.66% (p=0.107). Of all the variables collected in the study, at the time of extubation, NIF and Yang-Tobin index values were not recorded in 43.33% and 6.66% of the cases, respectively.
In the analysis of factors associated with the development of extubation failure, the logistic regression showed a significant association between the primary outcome (extubation failure) and history of IMV (OR=4.28, 95%CI: 1.44-12.66), diagnosis of pneumonia (OR=2.84, 95%CI: 1.15-6.99), and presence of active cancer (OR=2.92, 95%CI: 1.08-7.90). Variables such as duration of intubation, severity of admission condition as per SOFA score, and occurrence of stridor had no significant relationship with outcome (Table 2).
Table 2 Risk of extubation failure associated with different variables.
| Variable | OR | Standard error | p-value | Confidence interval |
|---|---|---|---|---|
| Age | 0.98 | 0.01 | 0.122 | 0.96-1.00 |
| Days on invasive mechanical ventilation | 1.07 | 0.06 | 0.190 | 0.96-1.19 |
| Previous intubation | 4.27 | 2.37 | 0.009 | 1.44-12.66 |
| Cancer | 2.92 | 1.48 | 0.035 | 1.08-7.90 |
| Pneumonia | 2.84 | 1.31 | 0.023 | 1.15-6.99 |
| SOFA score | 1.05 | 0.08 | 0.438 | 0.91-1.22 |
SOFA: sequential organ failure assessment; OR: odds ratio.
Source: Own elaboration.
The frequency of post-extubation laryngeal stridor in the participants was 3.88%, and the factors that significantly predict this event were history of intubation (OR=37.99, 95%CI: 2.22-650.88) and duration of IMV (OR=1.53 95%CI: 1.18-1.99). The cuff leak test did not significantly predict the occurrence of extubation failure or the development of stridor (OR=34.37, 95%CI: 0.33-3506.81) (Table 3).
Table 3 Risk of post- extubation laryngeal stridor associated with different variables.
| Variable | OR | Standard error | p-value | Confidence interval |
|---|---|---|---|---|
| Sex | 5.82 | 6.83 | 0.134 | 0.58-58.02 |
| Days on invasive mechanical ventilation | 1.53 | 0.20 | 0.001 | 1.18-1.99 |
| Previous intubation | 37.99 | 55.07 | 0.012 | 2.22-650.88 |
| Cuff leak test | 34.37 | 81.10 | 0.134 | 0.33-3506. 81 |
| Pneumonia | 6.64 | 8.04 | 0.118 | 0.62-71.34 |
| SOFA score | 0.65 | 0.20 | 0.167 | 0.36-1.19 |
SOFA: sequential organ failure assessment; OR: odds ratio.
Source: Own elaboration.
Discussion
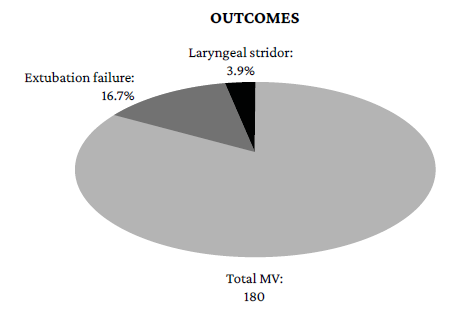
The frequency of extubation failure in the present study was 16.66% (Figure 2), which is within the 10% to 20% range described in the literature.3,8,13 These data indicate that the event continues to be common and that more research on interventions that can minimize its impact is needed, such as shortening the duration of intubation as much as necessary; early bridging to strategies such as noninvasive mechanical ventilation or high-flow nasal cannula; and developing additional tools that can predict and reduce it.
The present study also found that a history of intubation (OR=4.28,95%CI: 1.44-12.66; p=0.009), a diagnosis of pneumonia as the cause of respiratory failure (OR=2.84,95%CI:1.15-6.99; p=0.035), and comorbidity with active cancer (OR=2.92,95%CI: 1.08-7.90; p=0.023) were significantly associated with the occurrence of extubation failure. These factors, very easy to obtain from medical records, can help physicians to properly identify critically ill patients at risk of extubation failure, and thus take appropriate therapeutic or preventive measures.
It has been suggested, as causal mechanisms, that previous intubations are a marker for the presence of major comorbidity; in addition, having undergone IMV produces muscle damage with deconditioning and is associated with neuropathy, a condition that is difficult to overcome.23,24On the other hand, cancer itself is a chronic inflammatory state in which the lung can often be affected and is often accompanied by malnutrition and immunosuppression that impede the resolution of the conditions that generate respiratory failure.25,27 Finally, pneumonia has been described as a factor associated with extubation failure,1,28as it hinders good pulmonary gas exchange, affecting the efficiency of the respiratory system, and complete recovery can be slow, taking up to four weeks.
Some of the probable risk factors reported in the literature for extubation failure include congestive heart failure, diagnosis of sepsis, pneumonia, asphyxiation, unscheduled extubation, inadequate mobilization of secretions, cuff leak test, and upper airway obstruction.13,29 Regarding these factors, the present research inquired about the diagnosis of sepsis, the cuff leak test, and unscheduled extubations, finding no significant association; in fact, the distribution of these events between cases and controls was very similar, with no significant differences being observed.
The foregoing may be explained by several reasons, such as the fact that this is a single-center study, thus reducing its interpretability in the general population; that low severity scores (generally <6 measured by the SOFA score) in the case of sepsis lead to a lower risk of complications; and that the existence of variables not yet determined may have more weight in the prediction of the event of interest (Table 1). The diagnosis of pneumonia, on the other hand, showed an asymmetric distribution between groups (43.33% in cases vs. 23.333% in controls; p=0.023), which was later confirmed in the multivariate analysis, where the diagnosis of pneumonia was significantly associated with extubation failure (OR=2.84, 95%CI: 1.15-6.99). This major finding did not go unnoticed since pneumonia is a frequent disease in the ICU, resulting in increased hospital stay, morbidity, and costs.
Furthermore, it should be noted that the present study found that a history of intubation was significantly associated with the occurrence of extubation failure, which, at the time of writing this article, had not been described in the literature,28 so this finding should be validated and confirmed in future research.
On the other hand, the frequency of laryngeal stridor was very low (3.88%) (Figure 2) compared to the 7% reported in the literature,9 even though the aim was to identify it prospectively and with a clear definition from the beginning. The factors that significantly predicted the development of post-extubation laryngeal stridor were duration of IMV (OR=1.53, 95%CI: 1.18-1.99) and history of intubation (OR=37.99, 95%CI: 2.21-650.88). However, history of intubation showed a degree of imprecision greater than the confidence interval, thereby compromising its validity due precisely to the low prevalence of the event.
The strengths of this research include its design, which allowed consecutive and prospective data collection from all patients admitted to the ICU (reducing selection bias). In addition, variables were defined beforehand, and patients were evaluated daily after intubation to verify outcomes of interest such as the development of stridor and cuff leak test values (reducing measurement biases). Similarly, an adequate sample size was collected for the outcome of extubation failure, which showed a frequency similar to that reported in the literature.13,28
However, there were certain difficulties, such as a very low frequency of post-extubation laryngeal stridor, which prevented an adequate evaluation of the factors associated with this outcome, and the inadequate registration of some variables that could not be included in the multivariate analysis (Yang-Tobin index and NIF). Moreover, recently described predictors of extubation failure were not evaluated because of limitations in research resources, including the presence of congestive heart failure due to high levels of brain natriuretic peptide (BNP) and N-terminal portion of B-type natriuretic propeptide (NT-proBNP), diastolic function suggestive of elevated filling pressures, muscle respiratory strength, or pulmonary and diaphragmatic assessment by point of care lung ultrasound (POCUS).16,30
Conclusion
Based on the results of the present study, it can be concluded that extubation failure continues to be a frequent outcome in the IMV population. For this reason, it is suggested to consider factors such as history of intubation, comorbidity with cancer, and diagnosis of pneumonia when stratifying critically ill patients to increase the likelihood of successful extubation.
On the other hand, post-extubation laryngeal stridor was a rare outcome, and only days of IMV and history of intubation were significantly associated with its occurrence.