Introduction
Core needle biopsy (CNB) is a frequently performed procedure (gold standard) for histopathological diagnosis of breast masses.1 However, after undergoing a CNB, some patients may develop a significant hematoma (a rare event) or a pseudoaneurysm (PA) of the breast (an extremely rare complication).2,3Although the latter is extremely rare, the treating physician should suspect the presence of a breast PA if, following a CNB, the patient develops an hematoma in the breast together with persistent pain and/or if a palpable mass is detected after hematoma resolution.2,3
Once breast PA is suspected, a Doppler ultrasound (US) should be preferably performed. If necessary, other confirmatory tests such as breast magnetic resonance imaging (MRI) may be also used for confirming the diagnosis.2 Regarding the treatment of breast PA, there are several options, including ultrasound-guided compression, thrombin injection, coil embolization, and surgical resection, the latter being an inexpensive and widely accessible procedure that also allows histopathological analysis of the surgical specimen.2
The objective of this paper is to report two cases of breast PA following a CNB of a breast mass. In addition, a literature review was conducted to identify similar cases reported in the PubMed database.
Cases presentation
Case 1
66-year-old woman with a mass in the left breast who visited the Breast Unit of a tertiary care center in São Paulo (SP), Brazil, in January 2010 due to breast carcinoma suspicion, which was confirmed through a mammogram and a histopathology report of the sample obtained by means of a CNB (performed without complications). A month later, the patient underwent segmental mastectomy, sentinel lymph node biopsy and breast symmetrization without any complications. The histopathology report of the surgical specimen revealed a 0.4cm well-differentiated invasive tubular carcinoma (G1) [anatomic/pathological stage: pT1a; pN0 (sentinel lymph node); M0(i+)]. Likewise, the following immunohistochemistry findings were reported: estrogen receptor (ER) positive, progesterone receptor (PR) positive (both 100%), human epidermal growth factor receptor 2 (HER2) (score 0-1) negative, and Ki67: 12%. The patient underwent adjuvant radiotherapy and hormone therapy with tamoxifen.
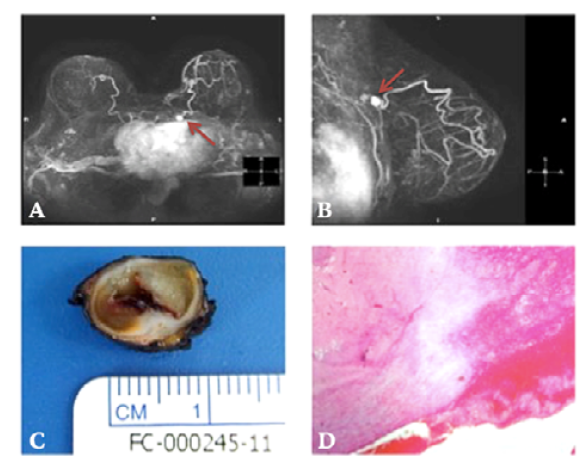
Then, in January 2011, the patient reported a palpable, pulsatile breast mass on the upper inner quadrant (UIQ) of her left breast in a follow-up visit in which a Doppler US revealed a hypoechogenic mass with central blood flow on Doppler located in the UIQ. In addition, a breast MRI performed on the same day showed findings suggestive of a PA (Figures 1A and 1B). Taking this into account, surgical treatment was decided, and in February 2011 the mass was surgically resected using local anesthesia without complications. Figure 1C shows the resected PA (largest diameter: 1.6cm). The histopathology image of the surgical specimen is shown in Figure 1D. Currently, about 132 months after surgery (February 2011 - February 2022), the patient's health condition is excellent, and there is no evidence of malignancy or other complications resulting from the surgical resection of the PA.
Case 2
44-year-old woman who visited the Breast Unit of a tertiary care center in Teresina (PI), Brazil, in April 2021 due to a mass in the upper lateral quadrant (ULQ) of the left breast. On this occasion, a breast US showed a 1.4x1.0cm mass with lobular contours (BI-RADS® 4 lesion). As no abnormalities were found on the patient's mammogram performed in May 2021, a CNB was performed in the same month, and stromal fibrosis and stromal microcalcifications were described in the histopathology report. However, after undergoing the CNB, the patient presented with ecchymosis and a palpable mass in her left breast.
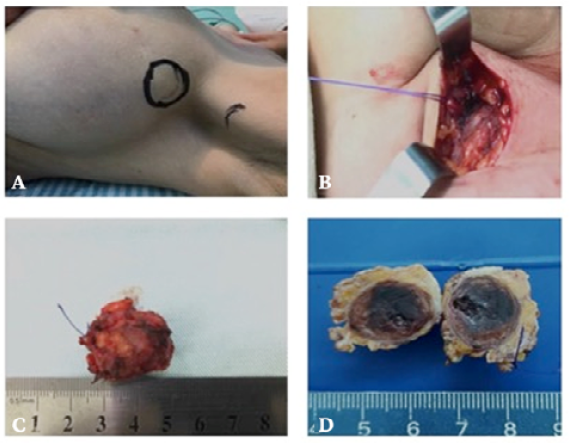
During a physical examination of the patient, a pulsatile mass measuring approximately 1.0cm was detected in the left axillary tail with an audible bruit on auscultation. Thus, a Doppler US was performed on the same day (May 2021), and a 1.4x0.7cm solid cystic lesion suggestive of breast PA was observed with central flow on Doppler. Considering this information, it was hypothesized that breast PA occurred as a complication of CNB. Surgical treatment was decided and a few days later the mass was surgically resected using local anesthesia and sedation without complications (Figure 2). The patient was discharged two hours after finishing the surgical procedure as there were no complications, and she had a favorable clinical course. About nine months after surgery (May 2021 - February 2022), the general condition of the patient is good.
Discussion
The occurrence of breast PA after CNB is extremely rare. In fact, after conducting a literature search in PubMed using the search equation "Breast Pseudoaneurysm AND Core Needle Biopsy AND Case Report" only 17 case reports were found (Table 1).1-17
Table 1 Cases of breast pseudoaneurysm following core needle biopsy reported in PubMed as of 21/02/2022.
| Author(s) | Patient's age (years) | Indication of CNB | Clinical manifestations of PA | Diagnostic imaging of PA | Greatest diameter of the PA (cm) | Treatment of PA | Outcome |
|---|---|---|---|---|---|---|---|
| Russell & Creagh-Barry1 | 45 | Breast mass | Bleeding and hematoma after CNB | Doppler US | 0.9 | Monitoring and watchful waiting | No complications |
| Filho et al. 2 | 51 | Breast mass | Bleeding, hematoma, and palpable, pulsatile mass after CNB | Doppler US and magnetic resonance imaging (MRI) | 2.9 | Surgical resection | No complications |
| Pesce et al.3 | 36 | Breast mass | Bleeding after CNB | Doppler US and MRI | 1.3 | Monitoring and watchful waiting | No complications |
| Azorín-Samper et al. 4 | 47 | Breast mass | Not described | Doppler US and MRI | 0.6 | Surgical resection | No complications |
| Vignoli et al. 5 | 62 | Breast mass | Pain and palpable, pulsatile mass after CNB | Doppler US and computed tomography angiography (CTA) | 2.0 | Surgical resection | No complications |
| Lee et al. 6 | 64 | Breast mass | Palpable, pulsatile mass after CNB | MRI, Doppler US, and CTA | 5.0 | Surgical resection | No complications |
| Sasada et al.7 | 51 | Breast mass | Bleeding and palpable, pulsatile mass after CNB | Doppler US, MRI, and CTA | 1.9 | Surgical resection | No complications |
| Farrokh et al.8 | 42 | Breast mass | Pain and palpable, pulsatile mass after CNB | Doppler US | 2.0-3.0 | Ultrasound- guided compression | Complete resolution of pseudoaneurysm and thrombosis |
| Dixon & Enion9 | 46 | Breast mass | Bleeding, hematoma, and palpable, pulsatile mass after CNB | Doppler US | 3.0 | Surgical resection | No complications |
| Erdil et al. 10 | 41 | Breast mass | Bleeding, hematoma, and palpable, pulsatile mass after CNB | Doppler US and MRI | 0.2 | Surgical resection | No complications |
| Buck et al. 11 | 74 | Breast microcalcifications | Palpable, pulsatile mass after CNB | Doppler US | 3.0 | US-guided thrombin injection | Complete resolution of pseudoaneurysm and thrombosis |
| Bitencourt et al. 12 | 46 | Breast mass | Bleeding and hematoma after CNB | Doppler US | Not described | US-guided compression | Complete resolution of pseudoaneurysm and thrombosis |
| El Khoury et al. 13 | 50 | Asymmetric mammographic density | Bleeding and palpable, pulsatile mass after CNB | Doppler US | 2.0 | No treatment (patient refused surgical resection) | Spontaneous regression |
| Bazzocchi et al. 14 | 42 | Breast mass | Bleeding and palpable, pulsatile mass after CNB | Doppler US | 1.6 | Percutaneous injection of sterile 95% ethyl alcohol (patient refused surgical resection) | Complete resolution of pseudoaneurysm and thrombosis |
| Chorny et al. 15 | 44 | Breast mass | Bleeding and hematoma after CNB and skin discoloration and tenderness at biopsy site | Doppler US | 0.8 | US-guided compression | Treatment failure (patient was referred for surgical resection) |
| McNamara & Boden16 | 70 | Breast mass | Bleeding after CNB | Doppler US | 1.0 | US-guided compression (treatment failure) and thrombin injection | Complete resolution of pseudoaneurysm and thrombosis |
| Swain et al. 17 | 65 | Asymmetric mammographic density | Bleeding after CNB | Doppler US and magnetic resonance imaging (MRI) | 1.7 | Surgical resection | No complications |
CNB: core needle biopsy; PA: pseudoaneurysm.
Source: Own elaboration.
PA is usually caused by arterial trauma and inadequate suturing of blood vessels after surgical manipulation. Blood leaks through a breach in the vessel wall and collects in adjacent tissues, leading to PA formation.2 Moreover, it may be surrounded by a fibrous capsule. After CNB, PA may also occur in parenchymal organs, e.g., the liver and kidneys.2
PAs must be differentiated from simple hematomas, as the former require more serious therapeutic interventions. However, this might be difficult, since a hematoma may conceal the intrinsic pulsations of a PA.2,7It has been described that Doppler US has an accuracy of approximately 95% for the diagnosis of vascular anomalies and it is the most appropriate imaging test for detecting breast PAs.2,7In these cases, Doppler US shows an anechoic mass with arterial flow connected to a blood vessel. MRI also has a high sensitivity and specificity for the diagnosis of PA, and it is frequently used to diagnose breast PA.2,7Doppler US was used to reach the diagnosis of breast PA in the two cases reported here, while MRI was only used in one to confirm the diagnosis.
There are several treatment options depending on the characteristics of each case, including surgical resection, US-guided compression, color Doppler ultrasound-guided thrombin injection, or percutaneous embolization, among others.2 However, it has recently been reported that a watchful waiting approach, together with clinical follow-up, may also be adopted.1 In the cases reported here, surgical resection was chosen as the best treatment option, as surgery is a relatively inexpensive and definitive treatment. Besides, it is worth noting that PAs were resected without complications in both patients. Regarding the 17 case reports of breast PA following CNB found in PubMed, it was found that the patients' mean age was 51 years, that Doppler US was mostly used to confirm the PA diagnosis, and that surgical resection and US-guided compression were the main treatments used.1-17
Despite the rarity of breast PA as a complication of CNB, the appearance of large hematomas on the breast following CNB should raise the clinical suspicion of this entity. When this happens, at least a Doppler US should be performed after the resolution of the hematoma.2 Other diagnostic techniques such as breast MRI and computed tomography angiography of the breasts may also be used.2,3-7,10
Conclusion
Breast PA is an extremely rare complication of CNB, with only 17 cases described in PubMed to date. However, breast PA must be highly suspected in the presence of warning signs such as bleeding, hematoma, and a palpable and/or pulsatile breast mass after undergoing CNB.
Ethical considerations
This study was approved by the Research Ethics Committee of the Federal University of Piauí, Teresina (PI), Brazil, as stated in a concept issued by said committee under reference number: 5.044.112 (CAAE: 50022521.4.0000.5214). All ethical principles currently in force in Brazil to conduct biomedical research involving human beings were followed (National Council of Research resolution number 466/12),18 as well as international standards.19 Likewise, the patients signed an informed consent form and agreed to the use of their data to prepare this case report as long as their anonymity was preserved.