Introduction
Cardiovascular autonomic dysfunction is a cardiovascular disease (CVD) risk factor associated with the occurrence of health conditions such as hyperglycemia, high blood pressure, sudden death, and diabetes mellitus, therefore posing a higher risk of death.1 The use of heart rate variability (HRV) has been proposed to monitor patients with cardiac autonomic dysfunction. 2 HRV is a simple tool that describes the oscillations between heart beats (R-R intervals), accounting for the influence of the autonomic nervous system (ANS) on the sinus node and allowing the evaluation of its cardiovascular health-related behavior. 3 Heart arrhythmia has been associated with low HRV, 4 especially in patients with overweight or obesity, in whom a direct relationship between all-cause mortality and ANS impairment has been described. 5 Indeed, one of the consequences of overweight and obesity is the deterioration of cardiac autonomic function (CAF), which is manifested by decreased vagal activity and elevated sympathetic nervous system (SNS) function. 6
Physical activity (PA) is one of the most promising non-pharmacological interventions to prevent health complications in patients with overweight and obesity. 7 For instance, there is evidence showing that moderate-intensity continuous training (MICT) increases vagal tone, decreases resting HR, activates the parasympathetic nervous system (PNS), and favors autonomic control; 8 dynamic strength training (DST) improves metabolic and cardiopulmonary health; 9 and high-intensity interval training (HIIT) enhances physical and physiological fitness and contributes to reducing CVD risk factors. 10 However, there is insufficient scientific support to conclusively link the positive effect of such interventions on HRV in this population. These limitations are related to the high heterogeneity of components of PA programs in terms of frequency, intensity, duration (time), and types (FITT) of exercise. 11,12
Considering the wide range of PA-based proposals for the complementary treatment of overweight or obesity, it is necessary to conduct a systematic review to identify the most appropriate FITT planning-related variables and contents of such interventions, as well as perform a meta-analysis of the contribution of PA to the modification of HRV, which would make it possible to evaluate the relevance of these models for the control and regulation of patients with overweight or obesity. Hence, the objective of this systematic review was to determine the effect of PA on HRV in adults (>18 years old) with overweight or obesity, while a secondary objective was to determine which training model (HIIT, MICT, and strength-based exercise training models) best modulates HRV in this population based on the evidence reported by randomized clinical trials (RCT).
Materials and methods
This systematic review and meta-analysis were performed following the recommended guidelines for reporting this type of study and the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2020 statement. 13 The systematic review protocol was registered in PROSPERO on December 01, 2020 (protocol code: CRD42021224027).
Search strategy
Systematic searches were conducted between February and March 2021 in the Cochrane, Medline, Embase, Lilacs, and PEDro databases using the following search strategy: Study types: RTCs assessing the effects of PA on HRV in adults (>18 years old) with overweight and/or obesity; publication period: from January 2015 to June 2021; search terms: "Heart Rate Control", "Autonomic Nervous System", "Exercise Physical", "High Intensity Interval Training", "Obesity", "Overweight", "randomized controlled trial", alone and in combination using the "AND" and "OR" Boolean operators. The search strategy was first implemented in Medline and then adapted to the other databases. In addition, a snowball search was conducted to identify other RCTs meeting the selection criteria.
Eligibility and study selection
A data collection and selection form for each RCT was handled independently by two reviewers (JFV and CMA). To identify eligible RCTs, title and abstract screening were performed, followed by full-text reading by the two reviewers separately to verify compliance with the established inclusion criteria. Disagreements were discussed by the three authors (LFB, JFV, and CMA) until a consensus was reached.
Selection criteria and data extraction
Study types
Only RCTs following the PICOT (patient, intervention, comparison, outcome, and [sometimes] time) framework with two or more parallel groups were included. Uncontrolled studies and those conducted in animals were excluded.
Type of participants
Only RCTs involving apparently healthy men and women (i.e., with a clinically controlled disease or without a diagnosis of any disease) and older than 18 years with overweight or obesity were included in the review.
Type of interventions
RCTs describing interventions lasting four or more weeks, regardless of whether they reported or not the FITT of HIIT, MICT, and DST protocols, and the comparison model or control group, were included.
Type of outcomes
We looked for RCTs reporting the following intervention outcomes as part of their main and surrogate outcomes: outcomes on HRV, time domain parameters such as R-R intervals, standard deviation of normal-to-normal R-R (NN) intervals (SDNN), percentage of adjacent R-R intervals that differed from each other by more than 50 milliseconds (pNN50), root mean square of successive R-R intervals differences (RMSSD), and frequency domain parameters (low frequency [LF], high frequency [HF], and LF/HF ratio).
Data analysis
Once the RCTs meeting the inclusion criteria were selected, strict criteria were followed for their assessment, and the resulting data were documented: sample size (n), mean and standard deviation (SD) values, last name of the first author, year of publication, evaluation method, and HRV parameters (R-R intervals, SDNN, pNN50, HF, LF, and LF/HF ratio). Likewise, outcomes of interest, description of instruments, data collection protocol, and methods utilized were extracted. This information was collected independently by each of the three authors in a Microsoft Excel database (V2020); then, these databases were compared to identify discrepancies, review them, and based on this process, obtain a database with final data.
Finally, the Consensus on Exercise Reporting Template (CERT) 14 was used for reporting PA interventions, as it is a helpful instrument for assessing the completeness of interventions and allows the replication of the research and enriches its results.
Risk of bias
The risk of bias of the studies included in the review was independently assessed by LFB, JFV, and CMA according to the criteria described in the Cochrane Handbook and using the Risk of Bias Tool (Version 5.1.0).15 Each criterion was scored as low, high, or unclear risk.
Statistical analysis
The Cochran's Q test and the I2 test were applied since the primary outcomes were continuous variables. The standardized mean difference ± (SD), with its corresponding 95% confidence interval (CI), was considered as the effect size, and a p<0.05 was established as the significance level. The change in the measurement of HRV time and frequency parameters was assessed, and forest plots were used to detect and quantify heterogeneity among studies. Heterogeneity was considered to be low and moderate if P values <25% and between 25-50% were obtained, respectively, while high heterogeneity was established in the case of p<0.05 or I2 50% values. All statistical analyses were performed using RevMan 5.3 software (Cochrane Collaboration). A random effects meta-analysis was carried out to calculate pooled effects for each outcome variable. Subgroup analyses were then performed comparing differences: HIIT and MICT versus the control group in HF, LF, RMSSD, and SDNN; HIIT versus MICT in HF, LF, and RMSSD, and DST versus MICT and functional strength training (FRT) in HF and LF.
Results
Studies included in the systematic review
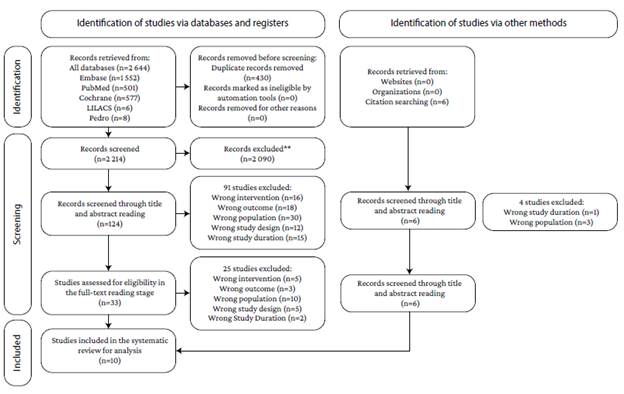
The initial searches yielded 2 650 articles (577 in Cochrane, 1 552 in Embase, 501 in Pubmed, 6 in Lilacs, and 8 in PEDro). These searches, as well as their results, were imported into the Rayyan software. Once duplicates (n=430) were removed, 2 090 articles were discarded in the title screening stage since they did not meet the inclusion criteria; 91 of the remaining 129 were discarded for the same reason in the abstract screening stage. Then, after performing a full-text reading of the remaining 33 studies, 25 were excluded. In addition, a snowball search was conducted in the 8 RCTs that met the inclusion criteria, and 2 more eligible studies were identified and included for final analysis. Therefore, 10 RCTs16-25 were included in this systematic review and meta-analysis. The study selection process is shown in Figure 1.
As shown in Table 1, the included RCTs were conducted in different countries (Australia, Brazil, Denmark, England, Italy, Lithuania, New Zealand, Republic of South Korea, and Saudi Arabia), and all 10 reported HRV parameters in patients with overweight and obesity, 16,18,25 type 2 diabetes mellitus,17,19,20,22,24 and metabolic syndrome21,23 as primary outcomes. In total, there were 398 participants, 205 were assigned to the HIIT, MICT, or DST intervention group and 193 to the control group. The mean age in the intervention group was 52.72 years, and in the control group, 52.27. All interventions lasted between 8 and 16 weeks: 12-week interventions in 5 studies, 19,20,22-24 1 6-week interventions in 4 RCTs, 16-18,21 and 8-week intervention in one study. 25
Table 1 Characteristics of the studies included in the review.
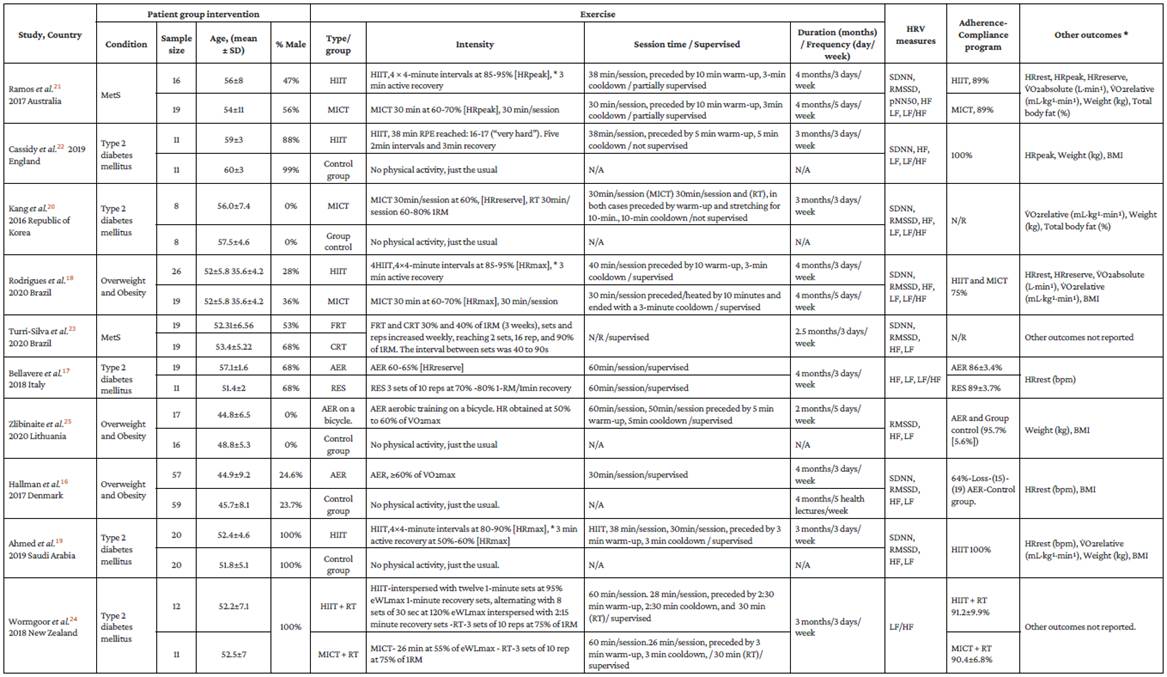
MetS: metabolic syndrome; HIIT: high-intensity interval training; MICT: moderate-intensity continuous training; FRT: functional resistance training; RPE: rating of perceived exertion;CRT: conventional resistance training; AER: aerobic training; RT: resistance training; eWLmax: estimated maximum workload; RES: strength training; HR: heart rate; HRmax: maximum heart rate; HRpeak: peak heart rate; eWLmax: maximal workload; 1RM: one-repetition maximum; HRrest: resting heart rate; HRreserve: heart rate reserve; VO2max: maximum oxygen consumption; VO2absolute: absolute oxygen consumption; VO2relative: relative oxygen consumption; BMI: body mass index; SDNN: standard deviation of R-R intervals; RMSSD: root mean square of successive R-R intervals; pNN50: percentage of adjacent NN intervals that differed from each other by more than 50 milliseconds; LF: low frequency; HF: high frequency; LF/HF: LF/HF ratio.
Source: Own elaboration.
Interventions
Out of the 10 studies, 5 used the HIIT protocol as the intervention method,18,19,21,22,24 4 used the MICT protocol, 16,17,20 and 1 used the DST method. 23 The intensity of the MICT protocol in both the intervention and the control group ranged between 60 and 70% [HRpeak, HRreserve, or HRmax], while in the HIIT protocol, it ranged between 80 and 95% [HRpeak or HRmax]. Five studies compared HIIT or MICT with a control group, 16,19,20,22,25 3 compared HIIT with MICT, 18,21,24 and 2 compared two strength protocols with MICT. 17,23 The duration of each training session varied from 30 to 60 minutes in the case of MICT interventions; training sessions in HIIT and DST protocols lasted 38 and 30 minutes, respectively. Regarding the frequency of the interventions, training sessions were carried out between 3 and 5 days per week in MICT interventions and 3 days per week in both HIIT and DST protocols.
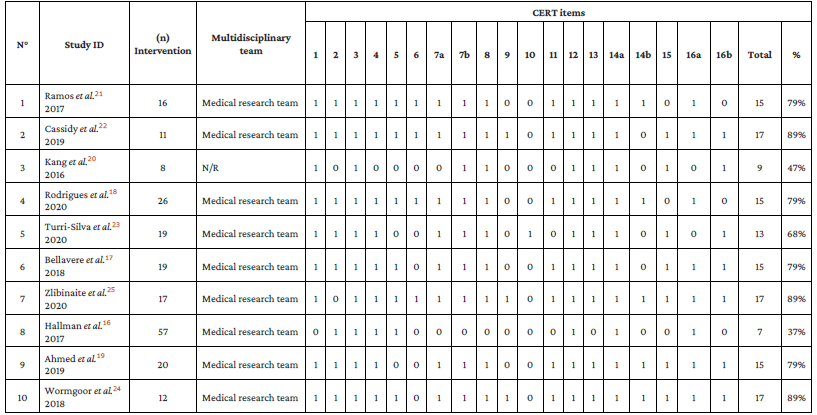
Reporting of the interventions - Consensus on Exercise Reporting Template
The assessment of the reporting of the interventions was carried out using the CERT checklist. The average score of the RCTs was 14 (73.68% compliance), and all described the FITT of the intervention and the means used for its execution. The full report is shown in Table 2.
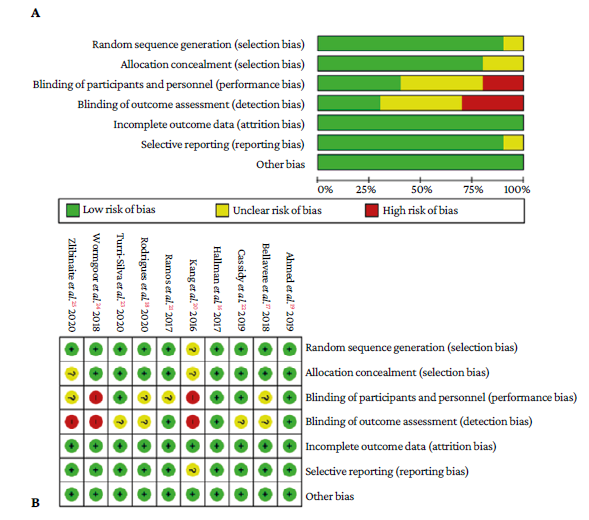
Evaluation of risk of bias
The risk of bias was assessed as per the criteria described in the Cochrane Handbook and using the risk of bias tool (Version 5.1.0).15 Most studies did not explicitly stated if there was blinding of personnel (medical staff and researchers) and participants: 3 RCTs had a high risk of bias, 20,24,25 4 had an unclear risk, 17,18,22,23 and 3 had a low risk of bias in these 2 domains. 20,24,25 Regarding random sequence generation, 9 studies had a low risk of bias, 16-19,21-24 and 1 had an unclear risk. 20 Concerning allocation concealment, 2 RCTs had unclear risk, 20,25 and the remaining 8 had a low risk of bias. 16-19,21-24 Finally, all studies had a low risk of attrition, reporting, and other biases (Figure 2). Overall, the quality of the 10 RCTs was moderate to high.
Outcomes
HRV measurements
All studies reported measurements for the time domain and frequency domain parameters. SDNN data were reported in 7 studies, 16,18-23 RMSSD in 7 studies,16,18-21,23,25 and HF and LF in 9 studies. 16-23,25
Effect of PA on HRV-RMSSD
The pooled effect for RMSSD was reported in 4 studies16,19,20,25 assessing the changes produced by the intervention (HIIT or MICT) in comparison with the control group, and in 2 RCTs18,21 comparing the effect of HIIT versus that of MICT. Heterogeneity was high in the HIIT or MICT versus control group subgroup (P=80%, p=0.002). Although a slight difference in favor of these two PA models compared to the control group was observed in the random effects model, results show that changes in RMSSD were not statistically significant in the intervention group (weighted mean difference [WMD]=0.79, 95%CI: -0.29 to 1.87; p=0.15). On the other hand, heterogeneity was low (P=0%, p=0.99) in the HIIT versus MICT subgroup, and results of the random effects model showed that there were no statistically significant differences in favor of either model. It seems that both HIIT and MICT show the same results (WMD=-0.23; 95%CI: -5.64 to 5.18;=0.93) (Figure 3).
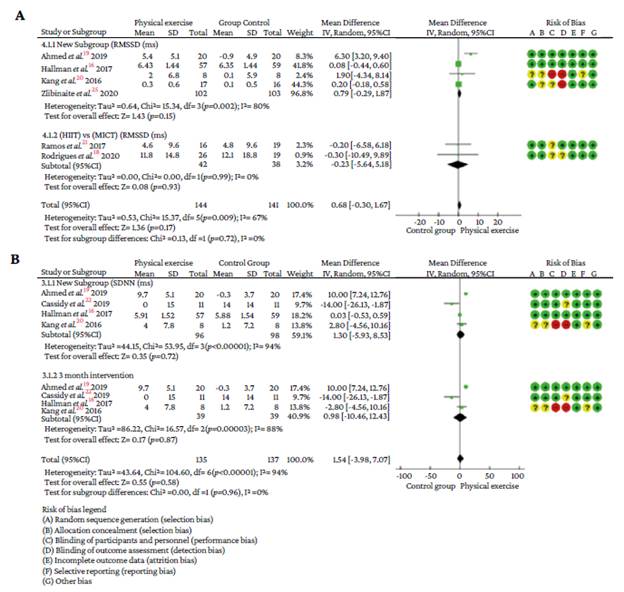
Source: Own elaboration.
Figure 3 A) Summary of the meta-analysis of the effect of HIIT and MICT on RMSSD in patients with overweight and obesity, stratified by the HIIT and MICT versus control group subgroup, and the HIIT versus the MICT subgroup. B) Summary of the random effects meta-analysis of the effect of HIIT or MICT on SDNN in patients with overweight and obesity, stratified by overall pooled result and 3-month intervention. Squares denote study-specific outcome estimates, and the square size represents the study's specific weight. Horizontal lines and figures in parentheses represent the 95%CI. Diamonds indicate summary results with the corresponding 95%CI.
Effect of PA on HRV-SDNN
Four RCTs evaluated changes in SDNN after the intervention (HIIT (n=2) 19,22 or MICT (n=2)16,20 in comparison with the control group; the intervention lasted 3 months in 3 studies, 19,20,22 and 4 months in the remaining one. 16 A significantly high heterogeneity was found in the overall pooled result and the 3-month intervention subgroup (P=94%; p=0.00001 and P=88%; p=0.0003, respectively). The random effects model showed that there were no significant differences between the intervention group and the control group in terms of SDNN changes in both the overall pooled result (WMD=1.30, 95%CI: -5.93 to 8.53; p=0.72) and the 3-month intervention subgroup (WMD=0.98, 95%CI: -10.46 to 12.43; p=0.87) (Figure 3).
Effect of PA on HRV-HF
HF was reported in 3 studies19,20,22 that evaluated changes in this HRV parameter after the intervention with HIIT or MICT compared to the control group. A significantly high heterogeneity was found in this subgroup (P=97%; p=0.00001). The effects of HIIT and MICT on HF were compared in 2 studies, 19,21 and heterogeneity between these 2 RCTs was low (I2=0%; p=0.57). Finally, DST versus MICT and FRT were compared in 2 other studies; 17,23 heterogeneity in this subgroup was high (P=88%; p=0.004). The results of the random effects model in these 3 subgroups showed that none of these intervention models had statistically significant effects on HF: HIIT or MICT versus control group (WMD=6.67, 95%CI: 1.71 to 11.63; p=0.008), HIIT versus MICT (WMD=0.17, 95%CI: -0.28 to 0.61; p=0.57), and DST versus MICT and FRT (WMD=0.91 95%CI: -0.67 to 2.50; p=0.26) (Figure 4).
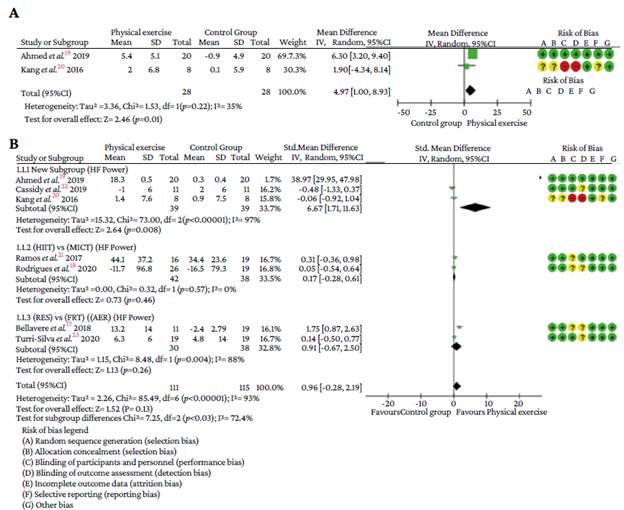
Source: Own elaboration.
Figure 4 A) Summary of the meta-analysis on the effect of HIIT or MICT on RMSSD in patients with overweight and obesity and stratified by the 12-week intervention versus control group subgroup. B) Summary of the meta-analysis on the pooled effect of HIIT or MICT versus control group, HIIT versus MICT, and DST versus MICT, FRT on HF individuals with overweight and obesity.
Effects of PA on HRV-LF
The pooled effect on LF was reported in 3 studies19,20,22 that assessed changes in this HRV parameter after the intervention with HIIT or MICT compared with the control group. In this subgroup, heterogeneity was low (P=0%; p=0.58), and there were no significant differences between groups in the random effects model (WMD=-0.32, 95%CI: -0.73 to 0.10; p=0.13). The effects of HIIT and MICT on LF were compared in 2 studies. 18,21 In this subgroup, heterogeneity was high (P=78%; p=0.03) and, according to the results of the random effects model, there were no statistically significant changes in favor of either model. It seems that both HIIT and MICT show the same results in terms of changes in LF (WMD=10.72, 95%CI:-39.89 to 61.34; p=0.68) (Figure 5).
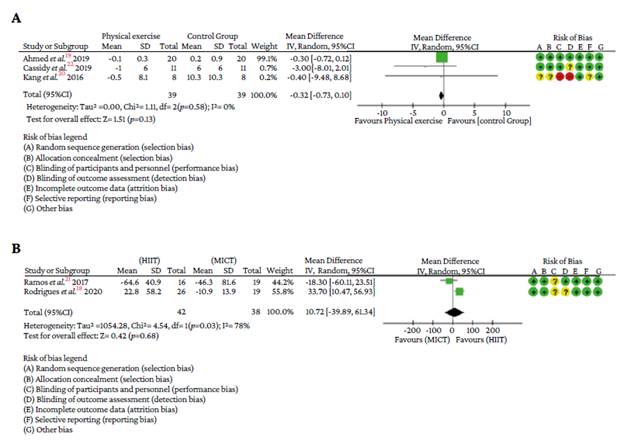
Source: Own elaboration.
Figures 5 A) Summary of the meta-analysis on the pooled effect of HIIT and MICT versus control group. B) Summary of the meta-analysis on the pooled effect of HIIT versus MICT on LF in individuals with overweight and obesity.
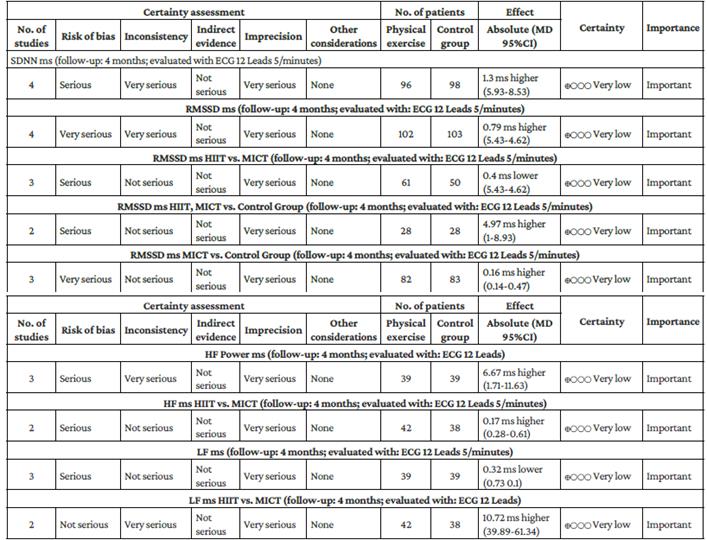
Regarding the quality of the evidence, the comparisons made by the 10 RCTs (either between them or with the control group) were deemed to be of poor quality. Therefore, the certainty of the evidence decreased. Both the lack of blinding and errors in the randomization of participants led to this grading. Besides, the wide confidence intervals, the high heterogeneity among studies, and the small sample size of each study also contributed to the fact that the outcomes reported by the RCTs, which are of great importance to those in charge of developing clinical practice, were finally graded as having a poor quality of evidence. The summary of findings according to the GRADE approach is shown in Table 3.
Discussion
The aim of this study was to determine the effect of HIIT and MICT models on HRV in adults with overweight or obesity (>18 years old) based on the evidence reported by RCTs. The literature review stage allowed summarizing the existing evidence of the effects of different PA modalities on autonomic control of cardiovascular function in individuals with overweight and obesity. The high heterogeneity found among the studies included in this review and the small number of participants in each study limited the analysis and the possibility of drawing conclusions in favor or against any PA model in relation to changes produced in the main variables that modulate the ANS.
A total of 10 RCTs (398 participants) reporting the effects of PA interventions on the main variables that modulate the ANS as their outcomes were included in this systematic review. The mean age of the participants was 52.72 years (intervention group) and 52.27 (control group), and 218 were males. Although the number of studies for each exercise modality and each outcome variable was unequal, the results showed that the effects were not statistically significant, except for the 12-week HIIT or MICT intervention versus control group subgroup (p =0.008), thus preventing us from concluding in favor of any of these two models in terms of positive changes in HRV parameters. PA interventions produced changes in all the HRV parameters analyzed, which is in line with what has been reported in the literature.26
Results of the meta-analysis showed that, compared to the control group, 12-week MICT or HIIT interventions did not cause statistically significant changes in SDNN. In the case of RMSSD, a slight difference, although not statistically significant, was observed in favor of these two exercise models in comparison with the control group. However, when the 12-week HIIT or MCIT intervention versus control group subgroup19,20 was analyzed, a significant change in RMSSD in favor of these two interventions was found (WMD=4.97, 95%CI: 1.00 to 8.93; p=0.01). Finally, when these two training models were compared (HIIT versus MICT subgroup), there were no statistically significant differences in favor of either model. It appears that both models may produce positive changes in this HRV parameter in individuals with overweight and obesity. It should be noted that SDNN and RMSSD represent the vagal nervous system, and that reductions in these parameters are associated with increased risk of cardiovascular morbidity and mortality. 27
In the case of HF and LF, there were no statistically significant differences in favor of PA interventions (HIIT and MICT) compared to the control group. In addition, there were no differences in favor of any intervention models in the HIIT versus MICT and the DST versus MICT and FRT subgroups.
Although it is clear that HF represents the PNS, there is not yet a consensus about LF since some studies consider it an index that allows evaluating sympathetic activity, while others state that it is a parameter that reflects both sympathetic and parasympathetic activity. 28 It is worth noting that in terms of interpretation, an increased LF suggests that there are no positive changes in HRV, as it would mean a sustained increase in SNS activity. 18
Consequently, even though there is evidence of the positive changes caused by PA interventions in the ANS, 26 considering that any cardiovascular adaptation requires an increase in cardiac vagal modulation and a decrease in SNS activity to be deemed as beneficial, the mechanisms through which these changes occur are still unknown. 29 In fact, there is still controversy about the physiological benefits of PA interventions with the ANS since some authors, such as Sousa Fortes et al.,30 in a study conducted in 31 young adults from Brazil (aged 18-25 years) to assess the effect of two different resistance training methods (clustering and multi-sets) on HRV, describe physiological changes related to the reduction of metabolite concentrations and proinflammatory cytokines production levels after exercising, while others such as Grässler et al.,31 in a systematic review that included 26 studies evaluating the effects of PA interventions (endurance, resistance, high-intensity, coordinative, or multimodal training) on HRV, report decreased norepinephrine levels in the blood after exercising, which would lead to CAF balance. In addition, body weight changes after completion of PA interventions could also promote positive changes in HRV. 29
Furthermore, while one of the objectives of this study was to determine which PA training model, HIIT or MICT, best modulates changes in the ANS of individuals with overweight and obesity, the results show that neither model is superior to the other in terms of their effects on the HRV parameters that were assessed. There were no statistically significant differences when they were compared, perhaps due to the high heterogeneity among the studies comparing these two training models or their small sample size. Even so, it is worth noting the changes produced by PA interventions make it possible to infer that HIIT, MICT, and DST could lead to positive changes in RMSSD and HF, important parameters that modulate HRV.
It is worth noting that the results of the present study should be interpreted with caution, that more RCTs assessing the effects of PA interventions on the variables analyzed here are required, and that such studies must maximize control bias measures since situations such as the presence of high or unclear risk of bias give rise to doubts regarding the outcomes assessed, so potentially valuable information might be lost. Furthermore, due to the small number of studies, heterogeneity was substantial in each analysis; moreover, not all RCTs provided information on the means and their SDs using the same unit of measurement, which might reduce the statistical power of the meta-analyses and induce biases in the estimates.
Finally, there is currently no clear evidence on which training models (HIIT and MICT) modulate HRV the best, as studies claim HIIT is better or vice versa. For example, Ramos et al.,21 in a research conducted in Australia in 56 people with metabolic syndrome who completed a 16-week HIIT or MICT program, claim HIIT was superior to MICT. Nevertheless, according to a recent systematic review conducted by Picard et al.11 (21 studies; 523 participants), MICT benefits in modulating HRV were superior to those of HIIT.
The findings of the present study are in agreement with those of some individual studies, such as the one conducted by Kang et al. 20 in South Korea in 16 women with type 2 diabetes mellitus, and systematic reviews such as the one by Picard et al.,11 which have reported that results regarding the effects of any PA intervention on the ANS after its completion are inconclusive and are not statistically significant.
The reporting of the interventions by the RCTs included for analysis was evaluated using the CERT tool. The average score of the 10 RCTs was 14 (i.e., a 73.68% compliance in the CERT scoring scale: 0-19), all provided information on the FITT of the PA training models, and most of them explained how the interventions were supervised and provided data on the participants' adherence. This information implies that all studies met sufficient CERT checklist items for their interventions to be replicable. Therefore, findings are a valuable resource to help decision-makers and medical staff in developing and implementing these interventions in clinical practice. 14
On the other hand, in terms of the methodological quality of the RCTs included in this review, most of them did not provide explicit information about the blinding of personnel and participants and how outcomes were evaluated, which reduced the certainty of the evidence. In addition, although the overall quality of the 10 studies was moderate to high, these findings could lead to an overestimation of the effect, so they should be cautiously interpreted. Likewise, it should be noted that publication bias was not assessed because the number of studies grouped by variable in the meta-analysis was <10. 10
Lastly, this systematic review highlights the need to strictly increase the methodological quality of primary studies, since the gaps in the reporting of interventions weaken the quality of evidence, which were rated using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach.
Some of the limitations of this study include the fact that there may be a risk of publication bias, as only studies indexed in the Cochrane, Medline, Embase, Lilacs, and PEDro databases were searched. Also, the absence of a person specialized in library science during the literature search stage, as well as the fact that only papers published in English and within the last 5 years at the time of conducting the search were considered, could have limited the amount of information retrieved and relevant data might have been left out. In addition, including studies conducted in people with type 2 diabetes mellitus and metabolic syndrome, along with the small number of studies included for analysis and the small sample size of each study, could have contributed to the high heterogeneity among studies and the inability to make strong assertions regarding the effects of PA interventions on HRV parameters in the target population.
Conclusions
Physical activity did not affect any of the HRV parameters studied in adults with overweight or obesity. In addition, it seems that both HIIT and MICT-based interventions for individuals with overweight and obesity could lead to similar changes in most of the variables modulating the ANS.