Introduction
Glaucoma is a multifactorial disease and the most common cause of irreversible blindness in humans worldwide (Chou et al., 2017). In dogs, it presents with progressive disorders characterized by apoptosis of retinal ganglion cells and optic neuropathy associated with a graying of the optic nerve (Pizzirani, 2015). In brief, the patient suffers from visual acuity loss in addition to understandable signs of pain due to increased intraocular pressure (IOP). Bilateral blepharospasm, episcleral vascular congestion, corneal edema, and behavioral changes, such as sleepiness, reluctance to exercise, and even loss of appetite and depression are also observed (Miller and Bentley, 2015).
Glaucoma is classified as open-angle (OAG) or closed-angle (CAG), depending on whether there is a defect in the elimination of aqueous humor. The OAG is known as primary when it occurs without an underlying disease (ocular or systemic); or secondary, when it is due to filter obstruction due to protein material associated with goniodysgenesis, resulting from an abnormal biochemical metabolism of the trabecular cells of the aqueous humor outflow system. In turn, increased IOP is due to increased resistance in the drainage channels (Gellat, 2014). The CAG represents around 20% of glaucoma cases in dogs, with a broad breed predisposition, being hereditary and bilateral. It is due to poor conformation of the anterior chamber, the iridocorneal angle, the trabecular meshwork, or any other part of the ciliary cleft (Baro-Lorenzo et al., 2018). Its pathogenesis evolves with 1) intermittent episode(s) of increased IOP -which are too high for axoplasmic flow from the optic nerve; 2) aqueous humor outflow obstruction; 3) retinal ganglion cell dysfunction -leading to optic nerve atrophy or degeneration; and, finally, 4) visual field loss and blindness (Miller and Bentley, 2015).
Considering that high IOP is only one of the risk factors for the development of glaucoma, reducing aqueous humor production or its outflow would be of benefit. In this sense, medical treatments with topical drugs are proposed. However, they may not control it on a long-term basis and, since it is a progressive disease, some patients may require surgical intervention to reduce IOP and slow the progression of glaucoma (Chen and Moeller, 2019).
Trabeculectomy (TEC) consists of establishing an exit route for the aqueous humor from the anterior chamber of the eye to the subconjunctival space, creating a filtration bleb under the conjunctiva through a small hole in the sclera. With this procedure, drainage of the aqueous humor is favored and, consequently, IOP is reduced (Urcelay et al., 2015).
A successful TEC for the treatment of glaucoma in dogs is based on developing a fistula between two anatomical spaces that do not heal. Viability of this fistula depends on the connective tissue, the aqueous humor, and the vascular tissue. Failure of the procedure refers to scleral fibrosis, which inhibits adequate drainage of the aqueous humor (Zheng et al., 2016). For a successful procedure, it is important to use fibrinolytics to preserve the filtering ampule over time. Its intraoperative application is performed below the subconjunctival and scleral flap (Zheng et al., 2016) at the end of TEC. Bevacizumab (Quiroz-Mercado et al., 2008; Herrera-Herrera and Bermúdez-Cruz, 2015), 5-fluorouracil (Alegre et al., 2002), and mitomycin C (Chen and Moeller, 2019) are drugs commonly used to inhibit the activity of fibroblasts and the subsequent development of scarring fibrosis in the TEC´s filtering ampoule (Güerri and Calvo, 2011).
Bevacizumab is a monoclonal antibody against vascular endothelial growth factor (VEGF) that binds to all the active isoforms of the molecule (Quiroz-Mercado et al., 2008). In humans, it is used to treat macular degeneration and block angiogenesis after filtering surgery -as is the case of TEC. The use of this drug reduces fibroblasts proliferation and migration to the surgical wound and, consequently, a slowdown in healing (Herrera-Herrera and Bermúdez-Cruz, 2015). In addition, it has an ocular anti-inflammatory effect attributed to its ability to bind the VEGF since they are leukocyte chemotaxis mediators (via VEGFR-1) expressed on the surface of leukocyte subpopulations, particularly macrophages and neutrophils (Azanza-Perea and Sábada, 2015).
The 5-fluorouracil belongs to the category of chemotherapy drugs called antimetabolites. These are similar substances to those normally found inside somatic cells. When cells incorporate these substances into their metabolism, they lose the ability to divide. This action inhibits fibroblastic proliferation and increases TEC success (Güerri and Calvo, 2011).
Mitomycin C (MMC) is an antimitotic antibiotic isolated from Streptomyces caespitosus. Its mechanism of action consists in the formation of irreversible bonds between the two DNA chains, preventing their duplication. Its intraocular action is aimed at inhibiting the growth and proliferation of cells with fibroblast activity (Villarreal et al., 2009) and has demonstrated its efficacy in prolonging the half-life of filtration bullae in TEC surgery by inhibiting the growth of fibroblasts and, therefore, scar formation (Alegre et al., 2002).
Although veterinary ophthalmology has evolved during the last decades, knowledge of glaucoma and its treatment is still needed. Therefore, this report aimed to compare fibrosis inhibition of the filtering ampoule after intraoperative application of bevacizumab, 5-fluorouracil, or MMC, in six dogs with primary chronic glaucoma subjected to TEC. To the author's knowledge, this is the first study comparing these three fibrinolytic drugs in veterinary medicine.
Patient examination
Clinical findings
Characterization of the patients that attended consultation at a veterinary ophthalmological unit in Medellín (Antioquia, Colombia) is shown in Table 1. The dogs were diagnosed with a primary chronic closed-angle glaucoma refractory to topical treatment applied for at least 2 months, and an IOP >25 mmHg.
Table 1 Characterization of the patients.
| Patient | Breed | Sex | Age (in years) |
|---|---|---|---|
| 1 | Basset hound | Female | 6 |
| 2 | Bulldog | Male | 1 |
| 3 | Crossbreed (Labrador retriever × German shepherd) | Male | 3 |
| 4 | Labrador retriever | Male | 8 |
| 5 | Springer Spaniel | Female | 8 |
| 6 | Siberian husky | Female | 7 |
As clinical findings, the patients presented no pupillary light reflex, negative visual threat eyeblink response, ocular pain associated with ocular hypertension, loss of appetite, behavioral changes (e.g. aggressiveness, apathy, depression) with abrupt rubbing of the affected eye and leaning head up against wall in addition to other signs, such as episcleritis, corneal ulceration and desiccation, buftalmus, mydriasis, and visual deficit.
Surgical and therapeutic approach
Each of the six patients underwent conventional TEC, a surgical procedure performed under general anesthesia with propofol induction and maintenance with isoflurane. The same surgeon performed all surgeries. Briefly, conjunctival dissection was performed, cauterizing the scleral vessels. The trabecular window was made at 12 o'clock from the eyeball, achieving a superficial scleral flap of 3 to 5 mm on each side, with medium scleral thickness, leaving a thin layer of underlying scleral bed. Conjunctival antimitotic drugs were applied to reduce subconjunctival scarring. A fragment was extracted from the cornea to the sclera, including the trabeculum and angular structures, additionally to iridian resection in its most peripheral part, achieving communication between the anterior and posterior chambers with the subconjunctival space through TEC (Urcelay et al., 2015). The suture of the superficial scleral flap was completed, allowing the apposition of the tapetum on the deep bed, conducting a repositioning to modulate aqueous humor outflow. A resorbable material (polyglycolic acid 8/0) was used. Once the conjunctiva was sutured, the anterior chamber was washed with a balanced saline solution, allowing tissue or blood debris to be removed, and simultaneously checking the operation of the filtering procedure and the formation of a correct subconjunctival filtration bleb (Alegre et al., García, 2002; Chou et al., 2017).
For the following process, patients were randomly assigned to three groups, obtaining two patients for each of the fibrinolytic drugs for intraoperative application, as follows: Group 1 (bevacizumab -Avastin®, Genetech Inc. San Francisco, CA), a single dose of 2 mg in 40 µL, injected with an intradermal syringe under the subconjunctival and scleral flap); Group 2 (5-fluorouracil - Acoflut®, Seven Pharma Colombia. S.A.S, Bogotá, Colombia), a single dose of 25 mg/mL, topically applied by embedded surgical sponge under the subconjunctival and scleral flap for 5 min; and Group 3 (MMC -Mitomycin C®, Quiminet, Bogotá, Colombia), a single dose of 0.5 mg/mL, topically applied by embedded surgical sponge under the subconjunctival and scleral flap for 5 min.
The IOP was measured by flattening tonometry in each patient, and the filtering ampoule was evaluated on days 1, 7, 30, 60, and 90 post-surgery by two different veterinarians.
Postoperative treatment for all patients included 1% prednisolone acetate (topical ophthalmic solution; 1 drop applied to the operated eye every 4 hours for 15 days, decreasing frequency every 2 weeks to 6, 8 and then 12 hours until completing 8 weeks of treatment), moxifloxacin (topical ophthalmic solution; 1 drop applied to the operated eye every 6 hours for 20 days), and cefovecin sodium (a single dose of 0.1 mL/Kg PV, SC). All patients were initially medicated with dorzolamide + timolol and the frequency of the medication was adjusted according to the evolution of each patient.
Data analysis
Demographic data were collected (e.g. breed, sex, age) and a progress scale was established according to three levels, being: 1, little progress; 2, moderate progress; and 3, excellent recovery, defined according to comparative evolution with the photographic record of each previous ophthalmological examination. The variables that contributed to the definition of the progress scale for each patient at each evaluation time (days 1, 7, 30, 60, and 90 of postsurgical evolution) were: eyeball closure degree (i.e. complete palpebral closure, partial eyelid-central cleft of 0.5 mm or more, buftalmus without eyelid closure, complete corneal exposure), signs of pain (i.e. mild blepharospasm, severe blepharospasm accompanied by epiphora, no signs of pain), iris coloration (i.e. normal, with moderate rubeosis -orange coloration with severe rubeosis, reddish coloration), and patient behavior (i.e. apathy/loss of appetite/aggressiveness to handling/constant head movements, no change in behavior). The IOP was classified as satisfactory (15-25 mmHg) or unsatisfactory (≥26 mmHg), as previously established (Chen and Moeller, 2019). Data were manually recorded in Excel spreadsheets (Microsoft Corp., Redmond, WA, USA) and then exported to Stata 16.0 (StataCorp 2020, Texas, USA) for descriptive statistical analysis for all variables of interest.
Results
Treatment allocation of the six patients as well as follow-up of the progress scale and IOP for each evaluation moment is presented in Table 2.
The first measurements showed unsatisfactory IOP values (≥ 26 mmHg), with signs of eye pain still evident, episcleritis, and enlargement of the eyeball. Evaluation of clinical progress -based on clinical signs, started as excellent from day 30 in all patients. The IOP evolution obtained at the time of each revision time was initially unsatisfactory, beginning to be controlled from day 30 in five of the six patients, and being satisfactory on day 60 for all patients (Table 2, and Figures 1 and 2). By day 90, one of the patients presented increased IOP with all the associated ocular clinical signs (Table 2; Figure 3).
Table 2 Intraoperative fibrinolytic treatment allocation and monitoring on days 1, 7, 30, 60, and 90 post-surgery.
| Patient | Treatment | Intraocular pressure (classification†; progress scale‡) | ||||
|---|---|---|---|---|---|---|
| Day 1 | Day 7 | Day 30 | Day 60 | Day 90 | ||
| 1 | Mitomycin C | 40 mmHg (NS; 2) | 32 mmHg (NS; 2) | 23 mmHg (S; 3) | 25 mmHg (S; 3) | 29 mmHg (NS; 2) |
| 2 | 5-fluorouracil | 38 mmHg (NS; 1) | 37 mmHg (NS; 2) | 32 mmHg (NS; 2) | 24 mmHg (S; 3) | 21 mmHg (S; 3) |
| 3 | Bevacizumab | 25 mmHg (S; 3) | 20 mmHg (S; 3) | 20 mmHg (S; 3) | 18 mmHg (S; 3) | 19 mmHg (S; 3) |
| 4 | Mitomycin C | 37 mmHg (NS; 2) | 30 mmHg (NS; 2) | 24 mmHg (S; 3) | 20 mmHg (S; 3) | 20 mmHg (S; 3) |
| 5 | 5-fluorouracil | 38 mmHg (NS; 2) | 32 mmHg (NS; 2) | 24 mmHg (S; 3) | 23 mmHg (S; 3) | 22 mmHg (S; 3) |
| 6 | Bevacizumab | 23 mmHg (S; 2) | 22 mmHg (S; 3) | 20 mmHg (S; 3) | 20 mmHg (S; 3) | 19 mmHg (S; 3) |
†S: Satisfactory (15-25 mmHg); NS: Not satisfactory (≥ 26 mmHg). ‡1: little progress. 2: moderate progress. 3: excellent recovery (all defined according to comparative evolution with the photographic record of each previous ophthalmological examination).
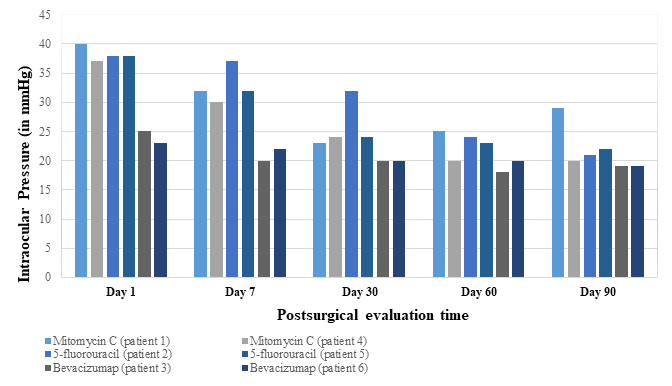
Figure 1 Comparative evolution of intraocular pressure (IOP) results at each postsurgical evaluation time of the six patients.
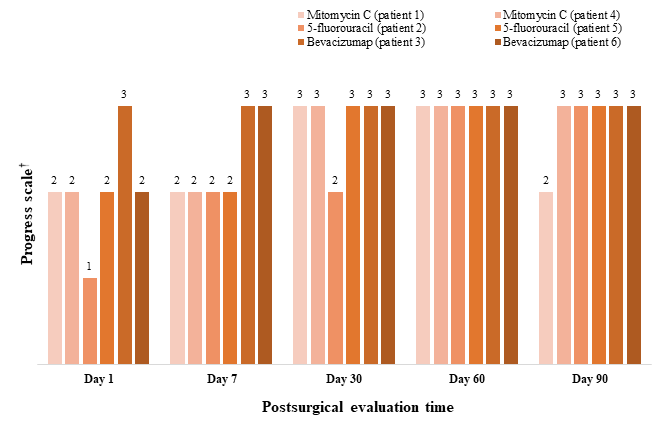
†1: little progress. 2: moderate progress. 3: excellent recovery (all defined according to comparative evolution with the photographic record of each previous ophthalmological examination).
Figure 2. Comparative evolution of the progress scale at each postsurgical evaluation time of the six patients in the study.
The photographic evidence of each patient during the postsurgical evaluation times is presented (Figures 3-8). For all cases, A corresponds to the day of TEC, B to day 1, C to day 7, D to day 30, E to day 60, and F to day 90 post-surgery.

Figure 3 Photographic evolution of ophthalmological evaluation of patient 1 (TEC + MMC). A: creation of filtering ampoule. B: active subconjunctival filtration bleb, but without adequate evacuation of aqueous humor. C: active ampoule, but with congestion and active hypertension. D, E: active ampoule with IOP control. F: moderate fibrosis of the ampoule.
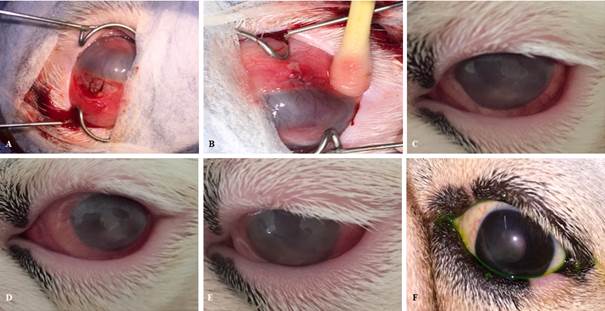
Figure 4 Photographic comparative evolution of each ophthalmological evaluation of patient 2 (TEC + 5- fluorouracil). A: creation of filtering ampoule. B: active subconjunctival filtration bleb, but without adequate evacuation of aqueous humor. C: partially active ampoule, but with hypertension. D: partially active ampoule. E, F: active ampoule with IOP control.

Figure 5 Photographic comparative evolution of each ophthalmological evaluation of patient 3 (TEC + bevacizumab). A: creation of filtering ampoule. B: active subconjunctival filtration bleb, but with localized hyphema around infiltration. C, D, E, F: active ampoule with IOP control.

Figure 6 Photographic comparative evolution of each ophthalmological evaluation of patient 4 (TEC + MMC). A: creation of filtering ampoule. B: active subconjunctival filtration bleb, but without adequate evacuation of aqueous humor. C: filtering ampoule without adequate flow, showing buftalmus and secondary ulcerative keratitis. D: active ampoule, improving the evacuation of aqueous humor. E, F: active ampoule with IOP control.

Figure 7 Photographic comparative evolution of each ophthalmological evaluation of patient 5 (TEC + 5-fluorouracil). A: creation of filtering ampoule. B: active subconjunctival filtration bleb, but without adequate evacuation of aqueous humor. C: filtering ampoule without adequate flow, showing a localized hyphema in the incisional area. D: active ampoule with IOP control and mild diffuse edema. E, F: active ampoule with IOP control.
Discussion
The objective of this case series report was comparing the fibrosis inhibition degree of the filtering ampoule after intraoperative application of bevacizumab, 5-fluorouracil, or MMC in six dogs with primary chronic glaucoma subjected to TEC. Patients presented a satisfactory outcome, with PIO compensation by tonometry being faster -although not immediately, after the surgical procedure.
It is essential to mention that patients not adequately responding to glaucoma therapy are increasingly found in daily practice, having to resort to surgical treatments for the management of this pathology. Therefore, it is necessary to resort to techniques such as TEC to stabilize patients diagnosed with glaucoma and help control IOP when tonometry values continue to be high after 2-3 months of topical treatment (Maggio and Bras, 2015). Nevertheless, this technique may also be insufficient for controlling IOP, being reported that the main cause of failure lies in conjunctival and episcleral fibrosis at the filtration ampoule level. This led to the understanding that TEC requires a filtering ampoule that remains active over time, including the use of drugs to reduce or prevent the formation of scar or fibrotic tissue, characteristic of good resolution of wounds (Chen and Moeller, 2019).
According to our results, a difference was observed between the drugs used in relation to IOP reduction and clinical evolution of the patients, requiring 2 months (60 days) of treatment and follow-up to stabilize the patient and decrease the clinical signs of ocular discomfort, pain, and inflammation characteristic of glaucoma, regardless of the fibrinolytic drug used. However, we believe that revision of patients should not take too long after observing improvement, since it is necessary to adjust the doses of antiglaucomatous drugs, which cannot be suspended even when IOP is within normal ranges. This case was observed in one of the patients, who presented a regression 90 days after performing TEC.
Scleral congestion was maintained in all patients until day 30, even if IOP was controlled. This may be associated not only with IOP itself, but also with the healing process that can be generated from the scleral vessels and that manages to stabilize with the fibrinolytic drugs. The decrease in diffuse corneal edema and corneal opacity improved immediately when bevacizumab was used. For patients treated with 5-fluorouracil and MMC, an improvement could only be observed until postoperative day 30. In addition, mydriasis reappeared on day 30 in the patients treated with 5- fluorouracil, but it only persisted in one of them during follow-up, in which IOP again increased above 25 mmHg. It is worth mentioning that the patients treated with MMC presented moderate scleral congestion again by postoperative day 90. Therefore, the analysis of the three fibrosis inhibitory principles (i.e. bevacizumab, 5-fluorouracil, MMC) evidences the favorable response of the filtering bleb with bevacizumab when IOP and patient progress scale is considered.
These results do not coincide with human studies, where MMC is the drug of choice for active maintenance of the filtering bleb (Wilkinset al., 2001; Quintero-Delgado, 2013; Hu et al., 2021). This may be due to lack of comparative studies on the action of other drugs with a similar mechanism in animals.
From this case report, we conclude that bevacizumab -as a fibrinolytic drug for intraoperative application- achieves IOP regulation under 25 mmHg after performing TEC, when used as a treatment for chronic glaucoma not controlled with topical treatment. It is, therefore, the drug of choice in dogs for maintaining the filtering bleb, helping to improve the signs of glaucoma. The other two fibrinolytic drugs used (i.e. 5-fluorouracil, MMC) improved the clinical signs associated with glaucoma, but did not completely prevent tissue fibrosis; therefore, there were relapses in IOP control up to 3 months after the surgical procedure.
Due to increasing glaucoma diagnosis in dogs and its resistance to topical treatment, strategies should target the modulation of post-surgical conjunctival and episcleral healing to prolong the survival of the filtering bleb, a key aspect for a successful surgery. Therefore, more studies should be conducted with larger number of patients to verify the results reported herein.















