Introduction
Close to one-half of deaths due to trauma are related to hemorrhage, hence the need to recognize it early on to mitigate the effects of hypovolemic shock which leads to tissue hypoxia, anaerobic metabolism, and metabolic acidosis.1 Vital signs and clinical scores have been traditionally used for recognizing shock states in patients with severe multiple trauma; however, various publications have shown that physiological responses to bleeding such as hypotension and tachycardia may not be proportional to the state of shock. This has created the need for using other predictors such as lactate clearance (LC), defined as a drop in lactate levels compared with baseline values; base deficit (BD),2 defined as the amount of base required to bring the pH in 1L of blood to 7.4, as a buffer mechanism to maintain pH within normal limits; and shock index (SI), defined as the quotient between heart rate over systolic blood pressure,3 allowing to increase sensitivity in the identification of hypoperfusion states.4 Our objective was to assess the relative risk of each variable for morbidity and mortality.
Methods
Prospective analytical cohort study with a follow-up between April 2016 and July 2017 of patients diagnosed with hemorrhagic shock,5 defined as systemic arterial hypotension (SBP < 90 mm Hg or mean arterial pressure (MAP)<70mm Hg), associated with signs of tissue hypoperfusion and hyperlactatemia. Inclusion criteria were patients taken to emergency surgery who had the study variables: blood gases plus serum lactate, vital signs, use of blood products and vasopressors, and SI, identified on admission and after 6 hours. Exclusion criteria were patients who died intraoperatively or within the first 6 hours, and with no blood gases, electrolytes, or serum lactate measurements at 6hours. LC was calculated using the formula6 (serum lactate T0 - serum lactate T6)/serum lactate T0 x 100, where T0 was the initial lactate measurement and T6 lactate measurement at 6hours, and it was considered adequate when values were lower than 20% as compared with the baseline measurement. Excess BD (-ExBD) was considered severe if <-6mEq/L7; SI was calculated and classified as severe if the value was >18; lactate, SI, and BD values were recorded on admission and after 6 hours. Follow-up was conducted after 28 days to determine mortality and morbidity, including pneumonia, surgical site infection (SSI), acute renal injury (ARI), suture dehiscence (including evisceration), and reintervention. In addition, the use of blood products and vasopressors was also recorded.
Relative risk and 95% confidence interval (RR and 95% CI) were calculated for morbidity and mortality for each variable, and managed with dichotomically. Univariate and bivariate analyses were performed, together with a binomial logistic regression. Finally, modeling and goodness of fit were done to assess for correlation between data found and expected data. Data analysis was performed using the Stata 14 software package. (StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP.) A P value <0.05 was considered significant. The study was approved by the interinstitutional Universidad Industrial de Santander (UIS) -Hospital Universitario de Santander (HUS) ethics committee.
Results
Of a total of 380 patients in the target population, 196 met the inclusion criteria. Mean age was 30 years, 8.16% were female, 89.8% were classified as American Society of Anesthesiologists (ASA) 4, and 10.2% as ASA 5. The most frequent injury (40%) was penetrating chest injury (Table 1).
Table 1 General patient characteristics and type of trauma
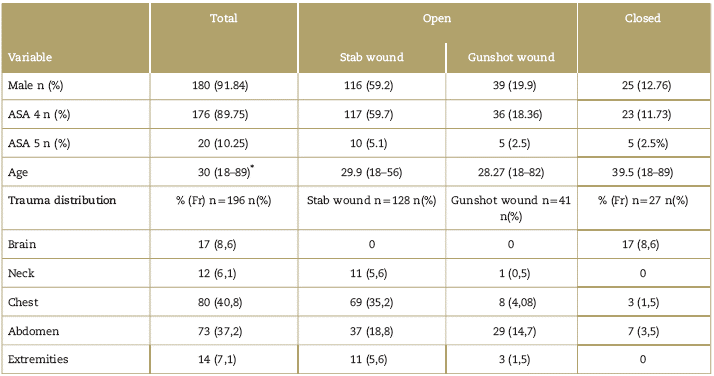
Age in average of years (minimum - maximum). ASA: American Society of Anesthesiologists physical status classification. Source: Authors.
Transfusion therapy was used in 45.4% of the patients, and vasopressor therapy was used in 32%. Although it was up to anesthetist to judge which therapy to use, it is important to highlight that the institutional protocol in this type of patient is to use the transfusion kit (5IU of red blood cells, 5IU of platelets and 5IU of plasma). The interquartile range for length of stay was 7 days, and 12 days in the intensive care unity (ICU). Morbidity at 28 days was 46.24%, with a predominance of surgical reintervention and ARI. Mortality was 9.69% (Table 2).
Table 2 Intraoperative, in-hospital, morbidity, and mortality variables

Vasopressors: norepinephrine equivalent dose >0.1mg/kg/minute and/or dopamine 5mg/kg/minute).
†Need for transfusion: trauma kit (5U of platelets, 5U of red blood cells, 5U of plasma).
Source: Authors.
Behavior of excess base, shock index, and lactate clearance on admission and at 6 hours
The behavior of -ExBD, SI, and aLC within the first 6hours was very variable. The drop in these values was greater for severe SI (sSI), and only 6.63% did not achieve normal values during that time period. -ExBD dropped by 45%, but only 59% showed non-critical values. After 6hours, 70% persisted with a lactate level of >2 mmol/L, lactacidemia was found in 20%, and aLC>20% was found in 84% of patients (Table 3).
Relative risk of morbidity according to sSI, aLC, and -ExBD
General morbidity was 46.24%, with predominance of reintervention and renal injury in 32%. In terms of associated variables, -ExBD on admission was not associated with morbidity, but its persistence at 6hours was associated with high and significant RR, except for suture dehiscence. sSI behavior on admission was a risk factor for needing transfusion therapy, and there was a significant association between the persistence of this score at 6 hours and morbidity, except for pneumonia, dehiscence, and SSI. Inadequate LC at 6 hours was associated with significantly high RR for all causes of morbidity studied. sSI and -ExBD at 6 hours were associated with the highest risk of ARI (Table 4).
Table 4 Relative risk of morbidity on admission and at 6 hours according to excess base deficit, lactate clearance, and shock index
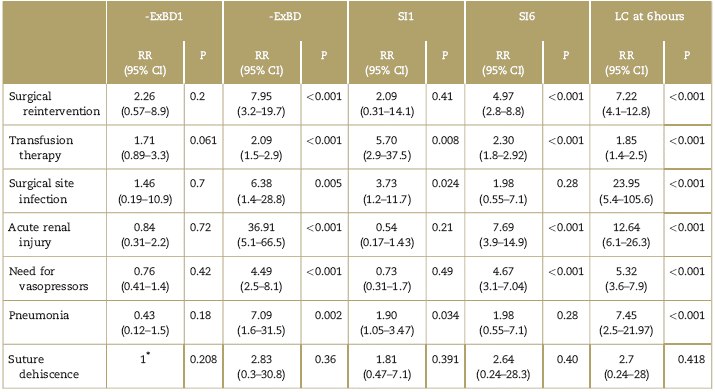
CI=confidence interval; -ExBD1=excess base deficit on admission; ExBD 6=excess base deficit at 6hours; LC=lactate clearance at 6hours; RR=relative risk; SI1=severe shock index on admission; SI6=severe shock index at 6hours.
∗ All patients with dehiscence showed severe EB.
Source: Authors.
Transfusion therapy and use of vasopressors
RR for the need of transfusion and use of vasopressors was significantly higher for sSI, LC, and -ExBD only at 6hours (Table 5).
Table 5 Relative risk of the need for transfusion and vasopressors according to severe shock index, severe base excess deficit, and lactate clearance

CI=confidence interval; RR=relative risk.
∗ > 2 units of blood products.
∗∗ norepinephrine dose >0.1 mcg/kg/min or dopamine mcg/kg/min.
Source: Authors
Relative risk for mortality: SI, LC, and -ExBD
At 6 hours, hyperlactatemia, LC<20%, and sSI were associated with an elevated and significant RR for mortality, but the same was not found for -ExBD. These findings will be subject for discussion (Table 6).
Binomial model for mortality
The group was evaluated as a whole and binomial regression and modeling were performed assessing those variables that could behave as risk factors. It was found that age >45 years, transfusion of blood products, renal failure, and clearance lower than 20% 6hours after admission were significant predictors of mortality with quite a high RR for acute renal failure (RR 49.19). Goodness of fitness (Hosmer-Lemeshow) showed perfect fit between observed and expected results (P = 0.86; deviance = 35.76266) (Table 7).
Discussion
One of the first authors to document the association between persistent and morbidity and mortality was Abramson, who in 1993 found that mortality was higher in patients with delayed drop in lactate levels down to baseline after 24 to 48 hours, and that survival was higher among those who achieved 100% LC within the first 24 hours.9 Our study found that mortality increases with persistence of lactacidemia over periods of time as short as 6 hours. In the 1990s, it was shown that not only high serum lactate levels upon admission but also clearance within the first 24 hours10,11 reduced morbidity and mortality, which was observed in our study as the highest rates of complications and mortality were found in patients with LC<20%. Research has emerged showing that initial monitoring is quite useful for predicting outcomes and that the trend toward serial monitoring is a valuable approach for in-hospital mortality.12 In our study, the measurement of hyperlactatemia on admission was only associated with the risk of transfusion, and no association was found with mortality or other morbidities, unlike the LC rate LC lactate level at 6hours, in which statistically significant associations were found. Among several studies, it is worth highlighting the systematic review by Kruse13 which found 8 retrospective studies of moderate quality, as well as a retrospective study by Odom et al,14 world authorities in perfusion and microcirculation, that present initial lactate and LC at 6 hours as independent predictors of mortality in trauma patients; the authors recommend conducting prospective studies.
In a systematic review, González et al15 conclude that the LC value in trauma has not been standardized and that there is heterogeneity in the different study populations and their management. We propose that a cutoff point of 20% for LC is adequate given that higher LC percentages might be related with more aggressive fluid therapies and potential adverse events.16 In a prospective observational cohort study,6 Regnier considers that early LC, defined as 2 and 4 hours, is found to be an important independent and prognostic variable, but with very close measurement periods. Given the dynamics of our services, patient volumes, and our teaching environment, we consider these periods to be very short and non-conducive to a cost-effective assessment of these patients.
More recently, Oliveros et al published a prospective cohort of multiple trauma patients admitted to the ICU in whom they measured lactate at 12 and 24hours. Their study showed lactate behavior similar to that found in other publications, with an association between mortality and persistently elevated lactate levels greater than 2.35 at 24 hours.17 The study has the drawback of not including an assessment of intraoperative behavior or intraoperative complications; it also has a selection bias as it only assesses the most critically ill patients transferred to the ICU and does not take into consideration patients who came in a state of shock but had a good therapeutic response and completed their course in the Post-Anesthesia Care Unit (PACU) and/or general wards. Our study has the advantage of assessing patients from the time of admission to the institution and following up on morbidity and mortality at 28 days, a period that is long enough to identify the various complications occurring in these patients.
In 2016, Dekker et al18 compared the different methods for LC calculation, and initial lactate measurement and concluded that there is no superiority of LC calculation over initial lactate measurement in terms of predicting morbidity and mortality. The author of this retrospective study mentions a potential selection bias as part of the limitations. In our study, we documented that LC is better able to predict morbidity and mortality as compared with initial lactate measurement.
As far as BD is concerned, Ibrahim et al,19 in a recently published systematic review of studies of the past 25 years, found that BD values >6 mmol/L are associated with severe injuries and complications such as acute respiratory distress syndrome (ARDS), acute lung injury, ARI, multiple organ failure, and increased mortality. In our study, we found an association with morbidities such as pneumonia, ARI, surgical reintervention, need for transfusion therapy, and vasopressors, although no correlation was found with the risk of mortality. Moreover, this review found that improvement of BD values within the first 48 hours was associated with a lower mortality rate, but we were unable to document that reduction in relation to BD values on admission or at 6hours.
Mutschler et al identified that BD -6 mmol/L on admission is an adequate cutoff point for mortality, in contrast with our study, which did not find that correlation. That same study established a new classification for hypovolemic shock based on the BD value, finding a better relationship between the degree of shock and the need for transfusion when compared with the classification proposed in the Advanced Trauma Life Support. This is supported by a retrospective review of 2954 patients12 which documented that, in 72% of patients with BD >-6 mmol/L, red blood cell transfusion was needed within the first 24hours; this is also consistent with our results that show that patients with severe persistent BD at 6 hours are at twice the risk of needing transfusion therapy.
Finally, we discuss the use of the sSI. In a systematic review, Olaussen8 concluded that the sSI is simple, reproducible, and useful for predicting the need for transfusion, and observed that the >1.0 threshold had a higher specificity, a reason why we also defined the value of >1.0 as the cutoff point. Our results also showed that an SI higher than 1 is predictive of the need for transfusion therapy.
In our setting, Charry3 published in 2015 a cohort study with 170 patients and found that an SI > 0.9 is predictive of worse prognosis at 24 hours after trauma. Another finding highlighted in that study as well as in ours is that there is a statistically significant correlation between serum lactate and an SI greater than 1 for mortality. However, our study has the additional advantage of not only predicting mortality with the SI but also predicting morbidity and the need for transfusion therapy and vasopressors.
In a retrospective cohort of 1419 patients, Mitra et al20 found that patients receiving a load of 1L of crystalloids who persisted with a high SI had a higher need for transfusion therapy, higher mortality, and worse outcomes than patients who responded initially to fluid therapy. Although we did not assess specific therapeutic effects, we documented that if the SI does not improve within 6 hours, there is a dramatic increase in mortality, the need for transfusion and vasopressors, and morbidity.
In another retrospective cohort of 16,269 patients, McNab et al studied the relationship between severe pre-hospital SI and the length of hospital stay, length of stay in the ICU, number of days on mechanical ventilation, and the use of blood products; they found that an SI > 0.9 indicates a higher probability of transfer to the ICU, emergency surgery, or death.21 In our study, we determined the initial SI which, extrapolating to this study, would be equivalent to the pre-hospital SI, and we were only able to find a greater need for blood products. In terms of mortality prediction, we found that a severe SI on admission is a protective factor, with statistical significance. We believe that when these patients arrive in these conditions, the trauma teams react faster and applies damage control principles, leading perhaps to a better impact on morbidity and mortality.
In the same cohort, McNab et al discuss their concern regarding the accuracy of the SI in the elderly. In a subgroup analysis, correlations for patients between 16 and 60 years of age were positive (P < 0.05). In patients over 80, none of the correlations with the outcome variables were statistically significant. In patients over 60 years of age, there was a correlation between a higher SI and an increase in mortality rates, and the authors concluded that the accuracy of pre-hospital SI declines in patients over 60.22 In our study, the mean age of the population was 30 years. Consequently, outcomes have to be interpreted with caution in geriatric ages as physiological compensatory mechanisms are diminished in this population group when exposed to trauma. Moreover, other interventions such as the use of beta blockers, cardiac devices such as pacemakers, implantable cardiac defibrillators, hip surgery, and heart transplant prevent compensation and will skew presentation toward a less compromised index.23 For this reason, lower cutoff points are proposed for this age group.
In terms of transfusion therapy, various studies have shown the association between transfusion of blood products and greater survival.24,25 Our finding that a severe SI on admission behaves as a protective factor may be secondary to the fact that patients arriving to our institution in such critical conditions trigger a protocol of massive transfusion, damage control surgery, and other resuscitation measures that impact mortality. If this index remains abnormal despite these measures, all compensatory mechanisms are overridden, and it becomes a statistically significant predictor or mortality. Other studies show that there is no reduction in mortality with the early use of transfusion therapy.26 In contrast, there are no studies in humans supporting the use of vasopressors in resuscitation of multiple trauma patients and, actually, their early use for hemodynamic support in patients with hemorrhagic shock may be deleterious and has been associated with higher mortality.27-29 A meta analysis of randomized clinical trials and observational studies comparing the different fluid administration strategies in trauma30 concludes that initial resuscitation strategies using liberal fluid administration may be associated with higher mortality. However, the authors of this review report that the available studies are subject to a high risk of selection bias and have a high clinical heterogeneity; consequently, this result must be interpreted with caution.
Because of its design, analysis, and follow-up, our study has validity and an adequate level of evidence. Therefore, the results are valid and applicable to our study population.
Limitations
Although the sample size in this prospective study, as compared with other international series, could be considered a limitation, there was an initial pilot study used to calculate the sample size. Consequently, the results obtained are statistically significant and not only totally applicable to our Colombian population and to our institution but also valid for extrapolation to different geographic settings. Although the mean age of the patients in our study was 30 years, it was not possible to conduct adequate subgroup assessments to determine behavior at different stages of life. Neither comorbidities that could affect LC (liver or kidney failure) nor renal or respiratory abnormalities that could affect acid-base balance before trauma were identified. Although we documented the risk of mortality for transfusion therapy and the use of vasopressors, we did not stratify groups based on the type of resuscitation. Therefore, these results must be interpreted with caution as close to 90% of our institutional staff members follow the protocol for trauma resuscitation and transfusion therapy concomitantly with the use of vasopressors such as noradrenaline and vasopressin.
Conclusion
LC < 20% at 6 hours is a risk factor for mortality and morbidity. No statistically significant association between morbidity and mortality and sever BD on admission, but severe BD at 6 hours is a risk factor for mortality and morbidity, except for suture dehiscence. Severe SI on admission acts like a protective factor for mortality, but persistence at 6 hours is associated with higher mortality and morbidity, except for pneumonia, suture dehiscence, and SSI. Given that the methods (biomarkers: lactate and base excess; scale CI) used in this study are independent predictors of mortality, they must be taken into consideration to guide resuscitation therapy and to use hemodynamic target-guided therapy guided in patients showing no improvement of control measures at 6hours.
Ethical responsibility
Human and animal protection. The authors declare that no human or animal experiments were performed for this research.
Data confidentiality. The authors declare that they followed the protocols of their institutions regarding patient data disclosure.
Privacy and informed consent. No patient data appear in this article.











 text in
text in 





