Introduction
Postoperative delirium is defined as an acute confusional state with altered levels of attention and consciousness.1,2 It has been observed mostly in extreme age groups, being the elderly the most affected group, with 10% to 60% incidence among patients receiving anesthesia.3 This pathology is considered of major interest in public health, as it may evolve toward dementia, increasing healthcare costs due to long-term treatment of patients.4
It is then necessary to identify the factors associated with the development of postoperative delirium. Studies at the international level report an association with the anesthetic technique, the type of surgery,5,6 fluid man-agement,7 genetic,8,9 and postoperative factors10; however, the bibliography available in our region is limited.
Therefore, the purpose of this study was to identify the pre-operative and postoperative predisposing factors to develop delirium in elderly patients receiving anesthesia, with a view to make an early diagnosis, administer timely treatment, and make an accurate diagnosis.
Material and methods
After receiving the authorization of the Local Committee on Research and Health Research Ethics 2601-registered in COFEPRIS under Number 13 CI 26 018 175 of August 24, 2016, an analytical cross-section study was conducted in a second-level hospital in the North East of Mexico.
A non-probabilistic sampling in elderly adults receiving anesthesia between November 2016 and November 2017 was conducted. The size of the sample was estimated for 2 proportions with a 95% confidence. Patients 60 years old and above, receiving general or neuraxial anesthesia and with a surgical time not exceeding 60 minutes were included. Patients previously diagnosed with cognitive impairment and patients undergoing an emergency procedure that precluded the evaluation of their prior condition were excluded.
At admission to the pre-anesthesia area, all patients gave their informed consent in writing and the research team asked a number of face-to-face questions related to sociodemographic variables (name, age, sex, marital status, and level of education). Age was classified into patients 70 years old and above, and patients under 70 years of age. The marital status was classified based on having a stable partner if they had been living together for more than 6 months uninterrupted. The level of education was classified into patients that received some education (from incomplete elementary school to professional education) and those who had no education at all.
Surgeries such as thyroidectomy, mastectomy, and cholecystectomy were conducted under general anesthesia, and procedures including hernioplasty (umbilical, ventral, and inguinal), hysterectomy, and lower urinary tract were conducted under regional anesthesia. The surgical procedures lasted between 60 and 120 minutes and the anesthetic agents used were Sevofluorane for general anesthesia and Ropivacaine for regional anesthesia. Fentanyl was also used at a dose of 3 to 5 mg/kg in patients operated under general anesthesia and at a dose of 3 mg/kg in patients operated under regional anesthesia. Dexamethasone at a dose of 0.1 to 0.15mg/kg, nonsteroidal anti-inflammatory agents such as lysine clonixinate at a dose of 100 to 200-mg intravenous (IV), and an ondansetron-type antiemetic agent at a dose of 0.1mg/kg were used as adjuvants.
Following the surgical procedure under anesthesia, patients were monitored at the Post-Anesthesia Care Unit (PACU), constantly asking for the level of pain using the visual analog scale (VAS) for pain. A VAS score >7 was classified as severe pain. Patients with hemodynamic instability with more than 5 minutes of hypotension- mean arterial blood pressure <60mmHg-were removed from the trial to avoid associating the cognitive impairment with cerebral hypoperfusion.
Subsequently, the information was recorded in the data sheet and the confusion assessment method (CAM) was used during the first 10 minutes following admission to the PACU. Such assessment is an internationally valid instrument to diagnose delirium in patients at high risk of presenting delirium,11 with 94% sensitivity and 89% specificity. CAM was administered by a non-psychiatric doctor and was based on direct observation and verbal communication with the patient. The instrument comprises 4 items: acute and fluctuating onset, attention alteration, disorganized thinking, and altered level of consciousness. A positive result in the first 2 items, and 1 positive result in any of the second 2 items was considered positive for delirium. Patients identified with postoperative delirium received Haloperidol at a dose of 2 to 5-mg IV.
The results obtained were uploaded to the Excel sheet and a database was subsequently developed, using the SPSS version 23.0 statistical software package to process the information.
The frequency of occurrence of delirium in the sample and its association with sex, age above 70 years, level of education, marital status, anesthetic technique, and severe postoperative pain was established using Pearson's Chi-square test, considering statistical significance at a P value <0.05. The odds ratio (OR was calculated with a 95% confidence interval (CI).
Results
A total of 100 patients with a minimum age of 60 years and maximum 93 years were included. The mean was 69.45 years (standard deviation = 7.95). There was a prevalence of females with 61%. 19% of the patients had no education and most (67%) had a stable partner.
With regard to the anesthetic technique used, 57% received neuraxial anesthesia and the rest received general anesthesia.
Severe postoperative pain was identified in 15% of all patients in the sample (Table 1).
Table 1 Overall description of the study population.
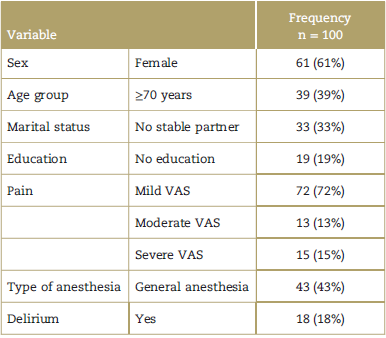
VAS=visual analog scale. Source: Authors.
Source: Authors.
A diagnosis of delirium was made in 18% of the patients; 61% of them received general anesthesia (P = 0.087), and 61% were females (P=0.91).
60% of the patients that experienced severe pain during the postoperative period experienced delirium (P = 0.000) and the OR was estimated at 12.66, with a 95% CI (3.6-43.8).
Delirium was identified in 44% of the patients with no education (P = 0.002), with an OR of 2.45, and a 95% CI (1.615.9). In terms of marital status, 66% of the patients with no stable partner experienced delirium, with an OR of 5.8, 95% CI (1.9-17.4) (Table 2).
Table 2 Probability of risk of developing delirium.

CI=confidence interval, OR=odds ratio, P=Chi square, VAS=visual analog scale.
Source: Authors.
In accordance with the age of the patients, delirium was identified in 72% (P = 0.001) of all patients over 70 years of age, with an OR of 5.6, and a 95% CI of 1.8 to 17.3 (Table 2).
In the multivariate analysis, the risk probability was significant among patients with severe pain (VAS above 7), with a B exponent of 5.49 (95% CI of 1.27-23.64) (Table 3).
Discussion
Proper management of the elderly patient contributes to reduce the number of complications that finally contribute to increase the cost of healthcare and the cost to society. Hence, this age group has increasingly been the focus of attention during the past few years.12
Benavides concluded in his study that elderly patients require a different approach, to understand the physiological, anatomical, social, and life differences that develop with age, with a view to providing optimal treatment of their pathologies.12
The results obtained show that a number of factors may be valuable to identify the populations at risk of developing postoperative delirium. Old age, not having a stable partner, and lack of formal education, are all sociodemographic factors that were associated with the occurrence of such condition. Similarly, experiencing severe postoperative pain is another associated factor.
According to the findings, the diagnosis of delirium increased among the older population. This is consistent with Carrillo,13 who advocates that the older the patient, particularly patients over 80 years old, the higher occurrence of delirium because of the vulnerability resulting from decreased brain plasticity and density. Monk further states that anesthesia plays a key role in the deleterious mechanism affecting these patients which induces neuro-apoptosis, which is accentuated among this age group.9 Winter et al14 also found this association between age over 70 and delirium in a trial published in Switzerland in 2015; while the incidence of delirium was low in this study, there was a prevalence among the group with an age similar to the population herein. Our study showed an almost 6-fold increased risk of experiencing delirium among patients aged 70 and above.
The anesthetic technique where delirium was more frequent was general anesthesia, but no statistically significant association was found. Hernández and Sánchez15 published a study in 2014 which found an association between the use of general anesthesia versus neuraxial with the development of delirium. There are however, several publications with results similar to our study. Wolters for instance in 2016 identified that the depth of general anesthesia and of sedation through neuraxial block had the same incidence of delirium, with no particular association to anyone of these techniques specifically. They concluded that the presence of delirium was due to the high level of brain activity suppression as measured with electroencephalography, regardless of the technique used.16 However, there is still a trend to attributing the cognitive deficit to the administration of certain drugs used in general anesthesia. In 1995, Bedford published the results of a review of 12,000 files of patients over 50 years old where he found that more than 10% of the patients undergoing surgery under general anesthesia experienced some mental decline and cognitive dysfunction, with a high incidence of delirium in elderly patients receiving general anesthesia. The recommendation was then to reserve such technique for emergency procedures.17
Monk et al described in 2008 an association between the years of formal education and the occurrence of delirium following non-cardiac surgery, and found that patients with a lower level of education exhibited a higher risk of developing delirium. Our study reported a 2-fold higher risk of experiencing delirium in patients with no formal education, which is consistent with the previous publication. No other series were found reporting such association.9
Poor pain management has often been reported as a factor associated with delirium.3,7,10 In the multivariate analysis of our results, severe pain (VAS over 7) was significant, with a 5-fold higher probability of risk. Some series report an association between poor postoperative pain control and the occurrence of delirium. This study showed an over 50% prevalence of delirium among patients with severe immediate postoperative pain. We reported a 12-fold higher risk of experiencing delirium among patients with severe pain based on the VAS score. Vaurio et al10 concluded that the presence and proper management of pain are important factors for the development of delirium.
Another sociodemographic variable considered in our study was the absence of a stable partner, which was associated with a 6-fold increased risk of experiencing postoperative delirium. Bekker refers to the involvement of the emotional status with the cognitive decline of patients; however, this variable was not identified as an associated or predisposing factor in previous studies.18
Thus, in accordance with our results, we report that there are sociodemographic factors identifiable in the patient's postoperative period that may be used as predictors of the risk to experience delirium, although these factors are not reported in the literature.
Of the few models available to predict the development of delirium in the elderly, E-PRE-DELIRIC is one of the small number of validated models that establishes the risk factors identified in postsurgical elderly patients to be admitted to an intensive care unit. The risk factors listed in this model are: age, a history of cognitive impairment, alcohol abuse, elevated blood urea nitrogen, admission category (surgery, trauma, internal medicine, inter alia), emergency admission, mean blood pressure, use of steroids, and respiratory failure.19 It is therefore necessary to conduct additional studies of the patient's pre-operative conditions, to be able to identify the population at risk and improve the detection of cases. The variables used in our study (severe pain, no schooling, general anesthesia, male gender, and unstable partner) may represent a valuable model to predict delirium in 88% of the cases.
We agree with Drews et al that highlight the importance of using a validated instrument for the detection of delirium signs and associated factors, such as those herein identified. Their study analyzed a sample of 1707 patients in the same age group as ours, with a 3-month follow-up after surgery. Their results indicated that 12% of the patients who experienced postoperative delirium developed posttraumatic stress disorder,20 leading to increased morbidity and mortality.
However, other series differ and challenge the association between anesthesia and long-term neurocognitive impairment in healthy elderly patients.
In a meta-analysis of 17 trials in postsurgical knee patients, Scott argues that in addition to not presenting any cognitive decline, the patients showed improved information processing speeds.21 So Bekker suggests that only individuals at high risk of delirium because of their history would be affected following surgery under anesthesia, presenting cognitive decline or signs of delirium.18
Consequently, it is imperative to continue with this line of research in the population identified as vulnerable, and to follow-up the results to assess the long-term impact that a high incidence of delirium actually has on the population. As suggested by Ramsay, it is not only a question of ensuring the survival of 1 individual, but ensuring his/her quality of life, particularly in terms of the patient's cognitive function.22
One weakness of our study is the potential bias resulting from using a non-probability sampling technique. However, one of the strengths is the use of a validated instrument with high sensitivity and specificity, in addition to the similarity between our results and those reported at the international level with larger sample sizes.
Conclusion
The frequency of occurrence of postoperative delirium in this series was 18%. Severe pain increases by 5.49 fold the risk of postoperative delirium.
Modifiable and non-modifiable variables must be further studied to improve the prognosis of patients undergoing an anesthetic procedure.
Finally, the recommendation is to preoperatively identify any subjects at risk of developing delirium; according to our results, these are patients with no formal education, absence of a stable partner, and older age. The intent is to provide postoperative follow-up using validated instruments for timely diagnosis and intervention.
Ethical responsibilities
Protection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics commit-tee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.











 text in
text in 



