Introduction
Closed reductions of fractures and/or dislocations are frequent in adult and pediatric patients coming to the emergency service. In the past, these procedures were performed with no standardized anesthetic or sedation techniques and, in the best of cases, attended by non-anesthetist practitioners with little training, or by the orthopedist who performed the procedure.
Patients undergoing these procedures tend to have a negative experience, associated with intense pain and anxiety, making it more difficult to manipulate the extremity and increasing the possibility of an unsuccessful reduction requiring intervention in the operating room under general anesthesia. This imposes a delay on timely intervention and increases costs for the health system.1
The use of sedation and analgesia for procedures (SAP) has become standard practice over the past decade because of the convenience, accessibility, and cost-effectiveness of performing orthopedic procedures in the emergency service instead of the operating room.2 SAP consists of administering sedative or dissociative agents with or without analgesia to induce an altered state of consciousness that will help the patient tolerate an unpleasant procedure while preserving cardiopulmonary function.3,4 SAP must be administered using a drug with a fast onset of action, short duration, safe, and easy to use, with minimal respiratory depression and an acceptable profile of adverse effects, and which can provide adequate amnesia and muscle relaxation.4
One of the more studied medications that meet all these requirements is ketamine, used for the first time in humans in 1965.5,6 It is a phencyclidine-related agent that produces functional and electrophysiological dissociation in the brain,7,8 creating a cataleptic state with amnesia and deep analgesia, but preservation of airway protective reflexes, spontaneous breathing, and cardiopulmonary stability. Its intramuscular (IM) or intravenous (IV) administration is quick and reliable, and its safety profile has been proven in several settings, taking the necessary precautions in terms of dose and route of administration. It is widely used around the world.9
Ketamine has a very good safety profile for sedation in the emergency room in the general population.10 The most frequent associated adverse effects are vomiting (16%), agitation (14%), and desaturation during the procedure (5%). However, major adverse events such as apnea, aspiration, need for intubation, laryngospasm, or permanent neurological damage due to hypoxia are rare, with a prevalence of 0.4% in the pediatric population11 and 0.005% for aspiration and need for intubation in adults.12
Despite the evidence of effectiveness and a favorable safety profile, ketamine is infrequently used, being the drug of choice only in 8% of cases according to a Dutch study13 and in 2.7% in a Canadian series.14
In 2017, the Colombian Society of Anaesthesia and Resuscitation (S.C.A.R.E.) published the clinical practice guideline for sedation outside the operating room,15 a paper of high scientific quality, containing a strong recommendation regarding the use of ketamine plus midazolam as the first choice for the performance of procedures under sedation in the emergency service, including fracture and dislocation reduction.
Given the paucity of data about the use of sedation with ketamine in the emergency service for orthopedic procedures in Colombia, the objective of this study is to describe the clinical and demographic characteristics and adverse events associated with the use of ketamine in these procedures in a high-complexity hospital.
Materials and methods
Design and study population
Retrospective, descriptive, observational case-control study in adult and pediatric patients coming to the emergency service of the Pablo Tobon Uribe Hospital (HPTU) in Medellin, Colombia, between January 2012 and July 2015, with displaced fractures of any extremity and/or dislocation of any joint, who required sedation with ketamine alone or in association with other medications for reduction and immobilization. These osteoarticular injuries are managed by an orthopedist most of the time, but because of human resource availability, sometimes they are managed by general practitioners or emergency medicine physicians. Multiple trauma patients were excluded.
Convenience, non-probabilistic sampling was used. The subjects were selected from the database of the HPTU Pharmacy Service, identifying patients for whom at least 1 ampoule of ketamine was delivered from the pharmacy to the emergency service during the study period.
Variables
The variables considered were age, gender, and outpatient profile (expected length of stay in the emergency service <6 hours). Trauma-related variables were also considered: localization of the injured segment, time between admission to the emergency service, and performance of the reduction procedure; total length of stay in the emergency service; consideration of fasting by the physician administering and monitoring sedation; application of additional drugs other than ketamine and their doses; position of the physician giving sedation; and reduction failure, defined as the need for a new reduction in the emergency service during the same admission, or the need for reduction under general anesthesia. Finally, clinically relevant outcomes related to the administration of sedation occurring during the procedure were identified, in accordance with adverse event definitions included in the work by Bhatt et al,16 and which were documented in the clinical records. Serious adverse events were defined as the presence of 1 of the following conditions: apnea, laryngospasm, hypotension, bradycardia, complete airway obstruction, aspiration, permanent central neurologic deficit, or death. In addition, significant interventions were defined as those interventions performed in response to any adverse event, including advanced maneuvers to maintain a patent airway, orotracheal intubation, vasopressor administration, or cardiopulmonary resuscitation maneuvers. Cases of desaturation requiring oxygenation with mask or cannula and/or airway manipulation, and vomiting during or after the sedation procedure were also recorded.
Data collection
The list of patients was obtained from the source mentioned previously and a review of the electronic clinical records (ECR) of the patients identified was conducted. The information on the variables described above was entered by 1 of the researchers (MIO-O) in an Excel spreadsheet previously designed for that purpose. The ECR at HPTU contains an editable pre-designed text note to document the sedation procedure, describing, among other things, fasting time before sedation and drugs used during the procedure, as well as the presence or absence of complications. A different researcher (COV-M) audited the recorded data and clinical records that did not contain sufficient information were excluded. Given the retrospective nature of the study, low-quality documentation was expected and, consequently, the nursing clinical record was included and clinically relevant outcome variables were measured in a yes/no dichotomic way, depending on whether they were present or absent in the ECR notes.
Statistical analysis
Qualitative variables were described as absolute and relative frequencies, and quantitative variables were described using the median and its respective interquartile range (IQR), given that the distribution was different from normal. All the statistical analyses were performed using the SPSS Statistics 17.0 software package (IBM, Chicago, IL).
The study was approved by the HPTU research ethics committee by approval document 19/2015 of September 24, 2015. Also, being a retrospective study, the committee give the exception of requesting informed consent.
Results
Overall, 354 patients were identified between January 2012 and July 2015 and included in the study. Of them, 74% were males, the median age was 21 years (IQR 12-32), and 68% were adults (>15 years). Of the muscle-skeletal injuries, 78% were localized to the upper limb. The median time between admission and the performance of the procedure was 98 minutes (IQR 56-159); the time of the last meal was documented in 8.5% of the cases. Sedation was assisted by a physician different from the one performing the reduction in 98% of the cases; sedation was most frequently provided by the general emergency physician (54%). Reduction failed in 7%, requiring new manipulation in the emergency room in 10 patients, and reduction under general anesthesia in 25 patients. In 98% of the cases, at least the combination of ketamine plus midazolam was used, and 3 or more drugs were used in 12% of the cases (ketamine, midazolam, and mainly morphine). The median length of stay in the emergency service was 261 minutes (IQR 173-710). The results for all the variables studied in the entire population and separated by pediatric and adult patients are shown in Table 1.
Table 1 General characteristics and by type of patient (adult/pediatric).
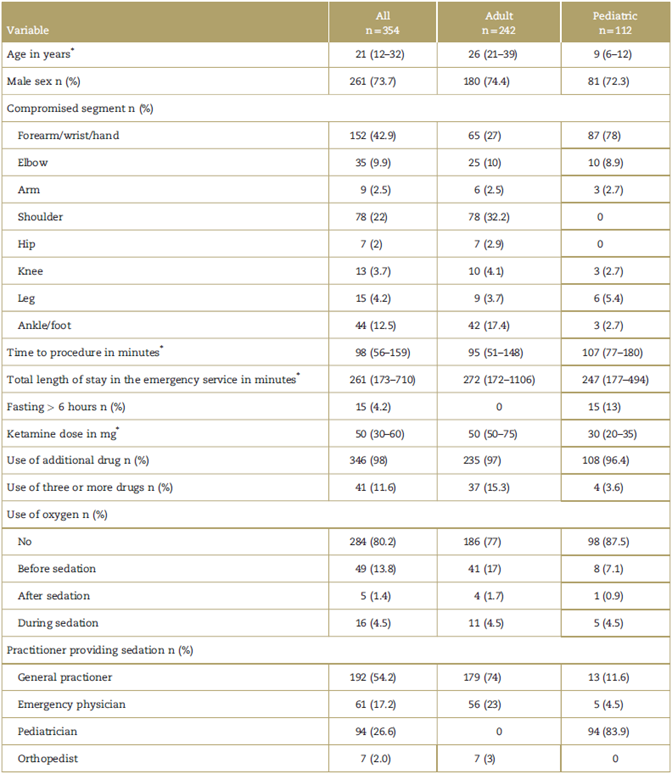
Source: Authors.
* Median and interquartile range.
Overall, 18 clinically relevant outcomes related to the use of ketamine were documented in 15 patients; the most frequently documented adverse event was desaturation in 11 cases (3.1%), followed by vomiting in 5 cases (1.4%). Table 2 shows the distribution of these outcomes according to the definitions established by Bhat et al.
Table 2 Clinically relevant outcomes (n=18) (absolute and relative frequency).
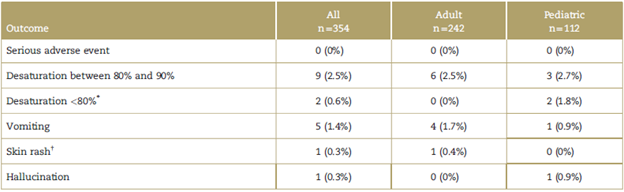
Source: Authors.
* The 2 cases of desaturation <80% were addressed with additional O2 through nasal prongs and maneuvers to maintain airway patency.
† The patient who developed a skin rash received sedation with ketamine plus midazolam and did not need any additional intervention.
Discussion
Care provided for young male adults predominated in the study. However, the use of ketamine sedation in orthopedic procedures varies in the world literature, and there are studies in all kinds of populations, evaluating the effectiveness, safety, and adverse events associated with its use in children and adults. Median age was 21 years. In 2015, a systematic review which included 6 studies assessed ketamine performance in the emergency service; in these studies, median age was 29 x 1.5 years, comparable with the 1 found in this study. The use of ketamine was highest in orthopedic procedures, higher than 90% in the majority of studies included.6 Regarding the segment, forearm, hand, and/or wrist involvement was found in 42.9% of patients, similar to the report by Messenger et al, in which 56.3% were upper limb procedures, and distribution by sex was similar to our population, which included 62.5% males.17 Sedation times were measured differently in various studies, making comparison difficult between those studies and this series.
Regarding procedure-related characteristics, the mean dose of ketamine was 50 mg (IQR 30), consistent with the reports included in the systematic review mentioned above (dose between 42 and 65 mg).6 When used for sedation in the emergency service, ketamine was usually associated with midazolam as recommended by the evidence, which has shown the safety and effectiveness of this combination. In 2010, a study examined the safety of IV and IM administration of this combination, studying adverse events, and found that agitation was less common in the group receiving midazolam (8% vs 25%, 95% confidence interval 6%-28%; number needed to treat (NNT): 6).18 Similar results regarding the safety profile have been reported in other studies.19,20 On the other hand, the most recent Colombian guidelines published on this topic contain a strong recommendation for the use of this combination.21
In this study, sedation was administered by the general practitioner 54.2% of the times, the emergency physician 17.2%, the pediatrician 26.6%, and the orthopedist 2%. The latter shows that sedation was administered by the same person performing the reduction, but this percentage corresponds to cases that were intervened before the implementation of Resolution 2003 of 2014 which requires the procedure to be performed by 2 different people.22 In 2011, O'Connor et al made a series of recommendations about sedation, including the practitioner giving sedation, and there were no differences in terms of safety and major complications, with the following rates and confidence intervals for every 10,000 sedations: anesthetists 7.6 (4.612.8), emergency medicine physicians 7.8 (5.5 to 11.2), intensive care physicians 9.6 (7.3-12.6), pediatricians 12.4 (6.9-20.4), and others 10.2 (5.1-18.3). There were no statistical differences (P < 0.05) between the rates of complications among practitioners before or after adjustment for potential confounding variables.23
In this study, complications were very low, with 95.8% of cases having no complications; the most frequent was minor desaturation in 9 patients (2.5%), with only 2 patients requiring maneuvers to secure the airway. Other complications such as major desaturation, vomiting, and skin rash were really negligible when compared with the existing evidence. A randomized clinical trial conducted in an urban pediatric hospital in children between 4 months and 18 years of age presenting to the emergency service with an orthopedic injury that compared the use of ketamine IV versus IM reported desaturation in 8.3% of the IV group versus 4% in the IM group, laryngospasm in only 1 case in the IV group, and vomiting in 11.9% in the IV group versus 26.3% in the IM group.24
A retrospective study conducted between January 1999 and April 2000 in pediatric patients between 1 and 12 years of age reported fasting of 1 hour or less in 12% of patients, between 1 and 2 hours in 39%, and 3hours or more in 49%. Vomiting occurred in 15.7% of the patients with fasting of more than 3 hours, 14% in cases with fasting of 2 to 3 hours, and in 6.6% of cases with fasting of 1hour. There was a linear increase in the vomiting rates with increasing age, and there was no relation between vomiting and the dose of ketamine.25 These results are different from the ones in our study in which 4.2% of the patients met the fasting requirement and vomiting was lower.
In 2007, a systematic review evaluated adverse events associated with the use of ketamine, including adult patients, with adverse events ranging between 0% and 76%. In the studies in which ketamine was used as monotherapy, psychiatric events ranged between 10% and 20%. Sedative agents were highly effective for preventing as well as controlling emergence reactions,5 which may explain the low rate of agitation among the patients included. Regarding the incidence of vomiting following emergence from the dissociation state, there was a wide range between 5% and 15% among the studies.6
Our study has some limitations pertaining to its retrospective nature and limited control over certain interventions such as oxygen administration through nasal cannula before sedation, which could potentially mask a higher prevalence of desaturation. Moreover, there is a selection bias considering the young population which intuitively points to the absence of comorbidities; consequently, the results cannot be generalized to all the patients coming to the emergency service. Likewise, there is no evidence of an active search for the identification of visual or auditory hallucinations that have been described as frequently associated with the use of ketamine.
Conclusion
In the studied population, there was a low prevalence of adverse events related to the use of ketamine for moderate sedation in patients requiring closed reduction in the emergency room; all of the events were minor and were solved leaving no sequelae in the patients.
The use of ketamine for orthopedic procedures in the emergency service is considered a very good therapeutic option, and findings are consistent with the guidelines of the S.C.A.R.E.











 text in
text in 


