Introduction
Cranioencephalic traumatism (CET) is considered one of the main causes of mortality and permanent disability in First World countries, especially in people with an active working life.1 In Colombia, the estimated incidence varies between 67 and 317 cases per 100,000 people.2 This is how the global frequency of the CET in emergency services in Colombia reaches 70%; the main cause is usually traffic accidents (51.2%).3
In3-5 this sense, the perioperative period is of importance in the course of CET patient management because, despite aggressive interventions in the emergency area, 1 or more of these factors may persist (or remain undetectable) upon admission to the operating room. For this reason, this period provides an opportunity to redirect resuscitation, with the primary goal of avoiding secondary lesions that overshadow the prognosis of CET patients.5 However, given the importance of such a scenario in the comprehensive management of the CET patient, perioperative management strategies, and clinical outcomes related to the care of the severe CET patient undergoing a decompressive craniotomy-type neuro-interventionism procedure have not been evaluated.
The objective of this study was precisely to describe perioperative management strategies and outcomes related to morbidity and mortality in patients with CET diagnosis taken to emergency neurosurgery at the Hospital Universitario San Vicente Fundación (HUSVF), in Medellín, Colombia.
Methods
A descriptive historical review study for patients with CET, was conducted at HUSVF, a fourth level of reference care hospital in the city of Medellín. The protocol was submitted for evaluation and approval by the institutional ethics committee of the HUSVF, with Deed 002 of February 2015, which exempted informed consent. Subsequently, researchers actively searched the process management system (System Administration Process) for the medical records of all patients over 13 years of age with a diagnosis of moderate or severe CET classified by the treating neurosurgeon and who underwent decompressive skull surgery between 2011 and 2014. There were no exclusion criteria. Information was collected from the time the patient was admitted to the emergency department to the time the patient was discharged from the institution.
Sociodemographic characteristics as well as the trauma mechanism of all patients were evaluated from the hospital database. The type of neurological injury and the patient's clinical status were then determined. Subsequently, intraoperative management was evaluated, as well as perioperative and clinical outcomes of patients who underwent decompressive craniotomy, such as: stay in intensive care unit (ICU), need for tracheostomy, neurological disability, hospital stay, and mortality. The definition of neurological disability is made according to the Glasgow outcome scale,6 where the result is dichotomized between good neurological recovery and neurological disability as a sequel upon discharge from the ICU.
Since the study was descriptive and included all patients who met the eligibility criteria during the period 2011 to 2014, it was not necessary to make the sample size calculation. However, the power of the study was calculated to estimate at least a difference of 10% in the outcome of perioperative neurological sequelae.
A univariate analysis was carried out as follows: for quantitative variables, means, and standard deviations (SD) were used if they had normal distribution, or alternatively, in medium and interquartile ranges; for qualitative variables, frequencies, and proportions were used. In addition, an exploratory bivariate analysis was performed between potential risk factors and perioperative mortality or neurological dysfunction. To this end, association tests were performed using odds ratio and Chi-square (x2) for qualitative variables. Estimators are presented with their respective confidence interval (CI) of 95%, and with a statistically significant P value when <0.05.
Results
During the period between April 2011 and April 2014, 258 patients were treated for CET in the emergency department of the HUSVF. Of these, 187 patients met the inclusion criteria (Fig. 1).
Table 1 describes the socio-demographic characteristics of the patients. The average age was 38 years (SD 17.56), the vast majority were male (89.3%) and without comorbidities (86.6%).
Table 1 Clinical and sociodemographic characteristics of patients.
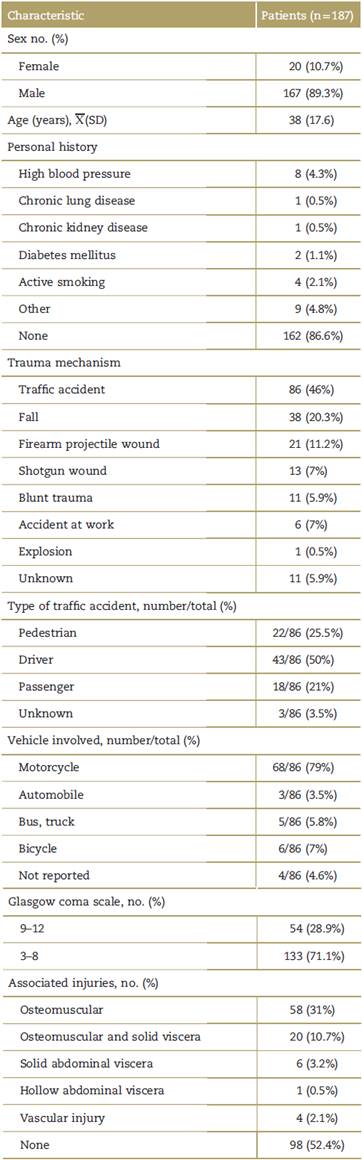
 =mean, SD = standard deviation.
=mean, SD = standard deviation.
Source: Authors.
The main cause of the CET was traffic accident (43%) and the most affected were the drivers (50%), followed by pedestrians (25.5%), while the type of vehicle involved was, in most cases, the motorcycle (79%).
The main neurological lesion found was a combination of extradural hematoma (EH) and subdural hematoma (SH) (33.7%), followed by EH (28,9%) and SH (24.1%) (Fig. 2).
Severe trauma, classified with a Glasgow coma scale (GCS) 3 to 8, was more frequent (71.1%) than moderate GCS 9 to 11 (28.9%). 52.4% of the patients had no associated lesions, and another 31% had associated musculoskeletal lesions.
100% of patients with surgical CET initiated protocol in the emergency room for this type of entity: elevated head, mannitol infusion, non-invasive monitoring of vital signs, and prophylactic antibiotic.
As for perioperative management, all patients were taken to surgery with balanced anesthetic techniques based on opioids and halogenated compounds. The use of hyperosmolar therapy during the intraoperative period was only recorded in 37% of patients. Tranexamic acid was used in 20.9% of patients; 21.4% of patients underwent transfusion therapy.
79.7% of patients presented episodes of perioperative hypotension with systolic blood pressure <90mm Hg. 41.7% of them required vasopressor support in continuous infusion; mainly, with noradrenaline, in 92.3% of the cases.
From the metabolic point of view, arterial gasometry and perioperative glycemia and lactate measurement were performed only in 47% of the patients. The main metabolic profile of the patients was hyperlactatemia metabolic acidosis, in 95% of the cases (Table 2).
Table 2 Perioperative hemodynamic and metabolic profile.

 = mean, IQR=interquartile range, Me=median, PaCO2=carbon dioxide blood pressure, PaO2=oxygen blood pressure, SD=standard deviation.
= mean, IQR=interquartile range, Me=median, PaCO2=carbon dioxide blood pressure, PaO2=oxygen blood pressure, SD=standard deviation.
Source: Authors.
In terms of clinical outcomes, no patient died during the surgical procedure; however, 30 of the 187 patients died during hospital stay, secondary to complications associated with the severity of the injury, that is a mortality of 16% (CI 95%: 10.7-21.3) (Table 3).
Table 3 Perioperative clinical outcomes.

Me=median, ICU=intensive care unit, IQR=interquartile range.
Source: Authors.
54% of patients who survived discharge had some degree of neurological disability. Assuming a difference of 10%, and based on the fact that this sequel is found among 45% to 70% of that reported in the literature,7,8 the study had a power of 79% to estimate the incidence of postoperative neurological injury in this care center.
29% of the patients were given a tracheostomy. The median stay in the ICU was 9 days, and the median hospital stay was 17 days.
The exploratory analysis found a positive association between the severity of injury and postoperative neurological mortality or dysfunction, as well as perioperative mortality and hypotension (Table 4).
Discussion
Trauma has become a high-impact event in the world, and head trauma has the highest morbidity and mortality. In addition, hospital stay times and expenses generate high pressure on the health system, with a great socioeconomic impact for the patient, the family and society.
The study found that most of the affected population were healthy men, which is consistent with previous studies showing how high-impact head trauma primarily affects the working-active male population.7-9
Congruently with other types of trauma, the largest portion of victims involved was due to traffic accidents; the motorcycle was the vehicle involved in more than half of the cases. This is consistent with the 2016 report of the National Institute of Legal Medicine and Forensic Sciences (Instituto Nacional de Medicina Legal y Ciencias Forenses), which recorded 50,574 cases treated for traffic accidents; that is, 80.5% of the total CET causes.10 These data differs from the HUSVF report during the 1990s, where the main cause of head trauma was gunshot injury. This difference can be explained by the social circumstances of the country during that period. In addition, the incidence of severe head injuries is increasing in direct relation to technological development and the introduction of high speed motor vehicles.
Among the pathophysiological types of trauma, the most common are extradural and SHs.5,4,11SHs are usually the result of acceleration-deceleration injuries; they occur more often in motor vehicle accidents and are more frequent than epidural hematomas.11 However, in the population studied, EH was more frequent than SH (28.9% vs. 24.1%), a phenomenon that could possibly be explained by a high impact of the event's energy, as occurs with traffic accidents on motorcycles.
Regarding perioperative management of the patient with severe CET, the main objectives should focus on early resuscitation, hemodynamic stabilization, emergent surgery, intracranial pressure control, cerebral perfusion pressure support, and multimodal monitoring.5,12,13 In accordance with these objectives, advances in neuro-monitoring and neurocritical care have changed the medical management of CET patients by improving their outcomes5; however, the study showed that hemodynamic and metabolic monitoring according to international recommendations for this type of lesion and surgical procedure was performed in only 47% of patients evaluated. It was not possible to identify a clear cause of this phenomenon through this study.
Despite the above, almost 80% of patients presented hemodynamic instability during the surgical procedure, which was managed, in most cases, with infusion of vasopressors; noradrenaline was the vasopressor of choice. Despite this management, exposure to an event of intraoperative hypotension was associated with a risk of mortality or postoperative neurological dysfunction 4.5 times more frequent than in patients in whom systolic blood pressure < 90 mmHg was not documented. Typically, cerebral perfusion pressure is determined by systemic blood pressure, which explains why this variable is the most critical for hemodynamic management of patients with severe CET.12,14 It is precisely because of this scenario that the recommendations warn of the need to maintain a systolic blood pressure > 90 mmHg throughout the perioperative management of the neurosurgical patient.1,4,12,13
As for the risk of development of endocranial hypertension in the perioperative period, it was not possible to objectively determine this complication, since no patient was monitored for postoperative intracranial pressure, despite being indicated for this type of event. However, 36.9% of patients were indicated hyperosmolar therapy as a management strategy for endocranial hypertension during the perioperative period.4,5
Coagulation disorders have been documented in literature to occur in approximately 1/3 of patients with traumatic brain injury, and are associated with increased mortality and worse outcomes.15 In this study, coagulopathy was documented in 0.5% of the patients. In addition, only 20.9% received tranexamic acid as part of intraoperative management. Although the CRASH-2 study showed that the drug decreases the risk of mortality in trauma patients,16 its use in this setting is still unclear.
Clinical factors associated with poor neurological outcomes in the CET patient include hyperglycemia or hypoglycemia,17 so their measurement is essential in the CET-critical patient. However, from the data obtained from this study blood glucose was measured only in 44% of patients admitted to the operating room, and at the end of the surgery only in 16%. This can be explained by the lack of records in the clinical history, rather than by a lack of request for such a measurement; however, the importance of measuring this variable allows for timely interventions in case of an abnormal result.
As for hydro electrolytic and acid base state disorders, these tend to be common in patients with CET, mainly associated with 2 variables: (1) the use of unbalanced or hyperosmolar crystalloids and (2) uncontrolled perioperative bleeding.4,18 In fact, in the analyzed data, although the electrolytic state was within the normal ranges, explained using crystalloid solutions-mainly balanced-a metabolic acidosis of hyperlactatemia type was presented, explained in the majority of the cases by perioperative bleeding. Most patients with acid-base disorder had another type of trauma associated with it, other than CET-primarily the musculoskeletal-which reinforces the concept that the high morbidity burden of the CET patient derives from the associated polytrauma.13
In evaluating mortality from this type of trauma, the study showed a mortality of 16% of all CET patients who were taken to surgery, an event that occurred during postoperative management, mainly due to complications related to polytrauma and the severity of the injury. Comparing these data with published national literature, mortality for moderate-severe CET is found to be between 18% and 48%.2 In this study, a great part of the patients with cranioencephalic trauma who required surgery (71.1%), presented GCS between 3 and 8 (severe), which can be explained by the condition of the study, as they were surgical patients. It is precisely in this group (Glasgow between 3 and 8) where a large association with in-hospital mortality was found, a finding that is, to a large extent, congruent with what has been reported worldwide. Although it is not possible to change the severity of the trauma, it is important in the perioperative period to identify that patients with a scale of greater severity deserve more timely action, and that all patients, without exception, who are very stable in the intraoperative period, should be taken to the neurosurgical ICU at the end of the procedure.
Finally, we highlight the high incidence of neurological dysfunction in this type of patient, which corresponds to 54% of all cases evaluated. These complications ranged from motor dysfunction to moderate-to-severe cognitive dysfunction, the latter being the most prevalent in our study. This finding explains 29% of patients who had to undergo definitive tracheostomies.
The greatest limitation of the study, in relation to its retrospective characteristic, was the lack of data in some of the clinical histories; furthermore, as it is a study carried out in a single hospital in the city, the possibility of generalizing the results is limited, despite the fact that this is a reference hospital in the city for such types of traumatic events. Bias control was not possible, nor was it foreseen within the methodological process, so any statistical association presented requires verification with analytical studies.
Conclusion
The study showed that CET is a critical event of high morbidity and mortality, despite the surgical management that is done, with a greater involvement in the young adult population, where the main mechanism involved is the traffic accident. Patients undergoing surgery had suboptimal hemodynamic and metabolic monitoring in almost 50% of cases, with the use of intraoperative hyperosmolar therapy in 36.9% and the absence of intracranial pressure monitoring. However, critical outcomes do not appear to be modified in patients with Glasgow <8, despite perioperative management. Severe neurological complications occurred in half of the cases of patients with moderate-to-severe CET.
Ethical responsibilities
Protection of people and animals. the authors declare that the procedures followed conformed to the ethical standards of the committee for responsible human experimentation and were in agreement with the World Medical Association and the Declaration of Helsinki.
Data confidentiality. the authors state that they have followed their workplace protocols on the publication of patient data.
Right to privacy and informed consent. the research was approved by the Institutional Ethics Committee with number 002 of 2015, in which the authors are exempted from informed consent, because the study is classified without risk according to the Ministry of Health Resolution 8430 of 1993. This document is held by the corresponding author.











 text in
text in 





