What do we know about this problem?
Clevidipine is a calcium antagonist with rapid onset, short half-life and no residual effect. It has been reported as a successful treatment for intraoperative hypertensive crisis secondary to pheochromocytoma, but we have just found three individual cases report about it .
What is the contribution of this study?
In a previous case of a patient undergoing pheochromocytoma exeresis in our hospital, we started the infusion of clevidipine during the first hypertensive peak. Now we report a series of three cases in which we started the infusion of clevidipine at low doses from the beginning of the surgery, before hypertensive crisis. We believe that initiating the clevidipine early and preventively could have helped to make the hypertensive peaks less pronounced.
INTRODUCTION
Pheochromocytoma is a tumor that produces catecholamine and is located in the adrenal medulla in 80-85% of cases. It can be associated with systemic diseases such as neurofibromatosis type 1.
Patients with pheochromocytoma can suffer symptoms as palpitations, arterial hypertension (AHT), diaphoresis or headache due to a high secretion of catecholamine.
Laparoscopic adrenalectomy is the treatment of choice, except in very large tumors or unresectable malignant tumors 1-3.
During surgery, there is a great risk of catecholamine release, especially during insufflation of the pneumoperitoneum and tumor manipulation 3. Severe hypertensive crises can occur even in patients who have never had hypertension. It is recommended to do a preoperative optimization with drugs that block the effect of catecholamine: alpha blockers, calcium channel blockers or angiotensin receptor inhibitors. For patients with tachyarrhythmia, the use of calcium channel blockers or beta-blockers (previous treatment with alpha) is recommended 4.
After tumor resection, the most common complication is severe arterial hypotension, due to an increased venous capacitance and the residual effects of hypotensive drugs used before5. To decrease it, it is recommended to do volume expansion during and after the surgery with fluid therapy guided by hemodynamic objectives 6, and the hypotensive drug used before tumor resection must have a short half-life.
Clevidipine is an intravenous calcium antagonist that has a rapid onset of action, short duration of effect, metabolism by plasma esterase and easy dose titration 7,8. It could be a good antihypertensive agent in these surgeries, but there are just a few publications about it 8-10. The following three cases describes its application in pheochromocytoma surgery.
METHODS: CASES REPORT
We present a series of three consecutive patients with pheochromocytoma that were treated with laparoscopic adrenalectomy in our hospital between 2017 and 2018. Patients are satisfied with the treatment received and we have obtained the signed consent of all of them to publish their clinical data.
They were a man and two women between 54 and 73 years old that were diagnosed by an increase of plasma or urinary levels of metanephrines and the results of an image test after they had presented clinical manifestations (table 1). They all received preoperative preparation an had normal BP and HR before surgery and on their arrival at the operating room (table 1). They were operated under general anesthesia: Anesthetic induction with propofol, rocuronium and remifentanil. Anesthetic maintenance: sevofluorane in patients 1 and 2, desfluorane in patient 3, remifentanil infusion and bolus of rocuronium in all of them. An epidural catheter was placed for postoperative analgesia and was used since the end of the surgery in all patients. They were monitored with Vigileo (company: Edwards Lifesciences)6.
TABLE 1 Patients' characteristics and diagnosis. Preoperative preparation and hemodynamic parameters.
| Characteristics | Patient 1 | Patient 2 | Patient 3 |
|---|---|---|---|
| Age (years) | 54 | 73 | 60 |
| Gender | Female | Male | Female |
| Chronic illnesses | Diabetes, dyslipidemia, hypothyroidism, glaucoma | Hypertension, dyslipidemia | Ex-smoker, dyslipidemia |
| Signs and symptoms | Recurrent hypertensive crises, tachycardia and sweating | Hypertensive crisis with palpitations, headache, tremors, paresthesias in the extremities and coughing with hemoptysis | Hypertensive crisis and sweating |
| Hormonal tests | Metanephrines in 24h urine: 5.210 μg/24 h (0,01-320 μg/24 h) Vanilmandelic acid in 24h urine: 19,9 mg/24 h (0,01-6,6 mg/24 h) |
Total metanephrines in plasma: 92,7 pg/mL (0-90 pg/mL). Noraderenaline in plasma: 3.856 pg/mL (0-420 pg/mL) Noradrenaline in 24h urine: 1.736 nmol/d (0-97 μg/24h). Normetanephrines in plasma: 4.424,4 pg/mL (0-196 pg/mL) |
Total metanephrines in 24h urine: 6.534 μg/24 h (0-302 μg/24 h). Normetanephrine in 24h urine: 4.916 μg/24 h (0,01-390 μg/24 h). Noradrenaline in 24h urine: 730 μg/24 h (0-97 μg/24 h). Adrenaline in 24h urine: 171µg/24h 0-20 μg/24 h. Dopamine in 24h urine: 171 μg/24 h (65-400 μg/24 h) |
| Image test | CT: Solid left adrenal 47 mm mass. Gammagraphy with 99m Tecneciosestamibi: Suprarenal left capture | CT: Left suprarenal 43X31X35 mm mass | MR: Right adrenal 77X74 mm mass which is globally hyperdense with acute adrenal hemorrhage |
| Pre-surgery treatment | Doxazosine retard 8 mg/24h Nifedipine retard 20mg/8h Propranolol 10mg/8h | Nifedipine 20 mg/8 h | Doxazosine 4mg/24h Propranolol 10mg/8h |
| Maxium BP during 48h pre surgery | 120/70 mmHg | 135/70 mmHg | 133/88 mmHg |
| Maxium HR during 48h pre surgery | 100 bpm | 75 bpm | 85 bpm |
CT= Computed tomography, MR= Magnetic resonance.
SOURCE: Authors.
In patients 1 and 2, the clevidipine infusion was started at low doses a few minutes after the anesthetic induction, despite the fact that they were normotensive, to try to avoid pronounced hypertensive peaks during the surgery. They had BP up to 169/77 -180/70 after the clevidipine infusion was started (figure 1). Patient 2 presented a significant depression of the ST segment in derivation II of the electrocardiogram. It was in the context of hypertensive peak up to 180/70 mmHg and sinus tachycardia up to 120 beats per minute. It normalized when the tachycardia and hypertension decreased. Patient 3 presented BP up to 217/107 during laryngoscopy. In that moment, the clevidipine infusion was started and BP was controlled in three minutes and remained stable (figure 1).
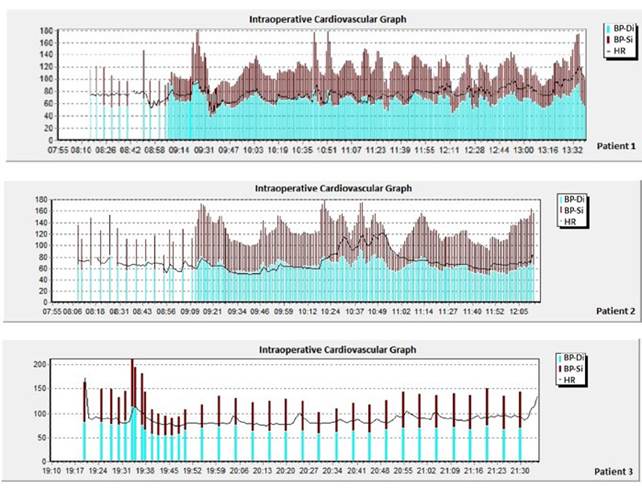
Patient 1: Blood pressure peaks up to 180/70 mmHg before and during tumor resection. Punctual episodes of arterial hypotension after the tumor resection and the clamping of the veins involved.
Patient 2: Blood pressure peaks up to 180/70 mmHg and sinus tachycardia up to 120 beats per minute before and during tumor resection. Punctual episodes of arterial hypotension after the tumor resection and the clamping of the veins involved.
Patient 3: Blood pressure up to 217/107 mmHg during laryngoscopy, before starting the infusion of Clevidipine.
BP-Di= Diastolic blood pressure in millimeters of mercury (mmHg), BP-Si= Systolic blood pressure in mmHg, HR= Heart rate in beats per minute.
SOURCE: Authors.
FIGURE 1 Blood pressure and heart rate during surgery.
After the clamping of all the veins involved, the clevidipine infusion was progressively reduced and could be removed in all of them. All patients presented episodes of arterial hypotension. In patients 1 and 2, hypotension was solved in less than 10 minutes just with fluid therapy guided by hemodynamic objectives. The hemodynamic objectives consisted of an increase of 10% or more in the cardiac index and the systolic volume index of the Vigileo monitoring system. The fluid therapy that was necessary to achieve this objectives was 1 liter of plasmalyte in patient 1 and 0.5 liters in patients 2 and 3. Patient number 3 also required a punctual 100 μg bolus of phenylephrine. They remained normotensive until the end of the surgery.
All patients were extubated in the operated room and transferred to recovery room.
Patients 1 and 3 were discharched to conventional hospital ward in six hours.
Patient 2 did not present symptoms or electrocardiogram of myocardial ischemia after surgery. Troponin curve was initially ascending, reaching a maximum of 83 ng/l. The cardiologist's diagnostic was myocardial damage in a hemodynamic context. The troponins normalized in 24h and the patient could be discharged from resuscitation area.
All of them remained with normal BP during the whole hospital admission, without the requirement of vasopressors or antihypertensive drugs. They were all discharged from hospital in less than four days.
DISCUSSION
The second surgical period of pheochromocytoma exeresis is associated with risk of hemodynamic instability, due to manipulation of the tumor and secondary relative hypovolemia 5.
Clevidipine is an intravenous calcium antagonist with rapid onset, short half-life, minimal effect on heart rate and myocardial oxygen consumption, dose-dependent and linear effect, metabolized by plasma esterase and with easy dose titration. It does not require dose adjustment by weight, renal or hepatic function 7,8.
The risk of arterial hypotension after tumor resection is lower if the hypotensive drugs used before have a short half-life. Clevidipine has not residual hypotensive effect 7,8 after tumor resection, so the risk of hypotension might be lower.
There are just a few publications about the use of clevidipine in this type of surgeries. Its use has been reported as a successful treatment for an intraoperative hypertensive crisis secondary to an undiagnosed pheochromocytoma9. It has been also described as a successful treatment of a patient with pheochromocytoma in the context of von Hippel Lindau disease10.
In a previous case in our hospital, we started clevidipine infusion during the first hypertensive peak, managing to control blood pressure quickly. However, even though the hypertensive peaks lasted just a few minutes, the patient had very high BP levels momentarily, even up to 279/122 mmHg8. In the three patients of this case series, we started the infusion of clevidipine at low doses from the beginning of the surgery, after anesthetic induction, despite the fact that they were normotensive. We believe that this could have helped to make the hypertensive peaks less pronounced (up to 180/70 mmHg after the clevidipine infusion was started). In future cases, if the patient does not present arterial hypotension, we will consider starting clevidipine infusion at low doses before the anesthetic induction, to try to minimize possible hypertensive peaks during laryngoscopy, as occurred in patient 3 that presented BP up to 217/107.
Clevidipine could be an antihypertensive agent of first choice in these interventions. We think that starting the infusion of clevidipine before the hypertensive peaks could help to make them less pronounced. However, more studies are needed to ensure its role in pheochromocytoma surgery.











 text in
text in 


