What do we know about this problem?
Information regarding the clinical behavior and the anesthetic and perioperative management of pregnant women with SARS-CoV-2 is starting to appear in the literature in the form of case reports and case series, although evidence and recommendations are still limited.
What does this study contribute that is new?
This study contributes to the knowledge of the clinical characteristics, results of anesthetic and perioperative management, complications and neonatal outcomes in seroprevalent pregnant women for SARS-CoV-2, delivered by cesarean section.
INTRODUCTION
The current COVID-19 pandemic declared by the World Health Organization on March 11, 2020, began in Wuhan, province of Hubei, China, in December 2019. The infection caused by the new SARS-CoV-2 coronavirus, spread quickly throughout China and the rest of the world, causing the disease and killing millions of people in its wake. Our country is among the most severely affected by this pandemic; as of the end of September 2020, official figures in Peru report more than 800,000 infected and more than 32,000 dead, the highest number of deaths for every one million people in Latin America, an among the highest in the world.
SARS-CoV-2 has affected all population groups - the obstetric population not being the exception - posing great challenges to the healthcare profession, compounded by scant knowledge about this new disease. One of those challenges is, no doubt, the perioperative management of obstetric patients.
Physiological changes occurring during pregnancy, both in the immune and cardiorespiratory systems, as well as atelectasis from the mechanical effect of the pregnant uterus, reduced lung capacity and high oxygen consumption are reasons to believe that obstetric patients will respond poorly to coronavirus pneumonia 1,2. In previous pandemics caused by other coronaviruses, adverse outcomes were higher in pregnant women than in non-pregnant women, with a higher number of orotracheal intubations, renal failure, disseminated intravascular coagulation, a larger number of patients admitted to intensive care units (ICU), and higher mortality 3.
It is encouraging to see that the initial reports about this disease in pregnant women describe a mild clinical picture, with a 1% mortality in the United Kingdom 4. As for anesthetic management, current recommendations guide to the selection of neuraxial anesthesia instead of general anesthesia, in order to avoid aerosolization and healthcare staff contagion. At this point, very little is known about the repercussion of COVID-19 on maternal and neonatal outcomes, or cesarean section-related complications.
The current literature on anesthetic management in this population is limited in terms of sample sizes and the quality of the studies. This work describes the clinical characteristics, the results of anesthetic and perioperative management, complications and eonatal outcomes in seroprevalent pregnant women for SARS-CoV-2 infection delivered by cesarean section.
METHODS
Patients and diagnosis
Observational, single-center study of pregnant women with serology of polymerase chain reaction (PCR) test for SARS-CoV-2, admitted to the National Maternal Perinatal Institute between April 1 and June 30, 2020. The protocol was submitted to the Research Methodology Evaluation Committee and the Ethics Committee of the National Maternal Perinatal Institute in Lima, Peru, for assessment and approval. The inclusion criteria were: pregnant women 18 years of age or older, with positive rapid or PCR test for SARS-CoV-2, undergoing cesarean section. The exclusion criteria were: pregnant women with a body mass index (BMI) of 40 or higher and/or fetal congenital malformations incompatible with life.
After approval of the protocol (Letter N.° 048-2020-DG-N°015-OEAIDE/INMP, July 8, 2020), the process of collecting the information was initiated using Google forms, with access restricted to the researchers only. The primary source for data collection were the clinical records of the individual patients. The epidemiological visualization window was 3 months and all patients who met the eligibility criteria were included in the analysis.
SARS-CoV-2 seroprevalence was determined by means of the qualitative rapid test in accordance with the reactivity criteria established by the Peruvian National Health Institute, and the interpretation was performed by the hospital clinical laboratory team. Samples of capillary blood were drawn using the SD BIOSENSOR Standard Q COVID-19 IgM/IgG Combo.
Perioperative management
The pregnant women were transferred from an isolation area to the operating theater, wearing surgical face masks. Two operating rooms were used exclusively for patients with reactive SARS-CoV-2. All the staff in contact with this group of patients in the operating room wore personal protective equipment against aerosols.
After obtaining the anesthesia informed consent, routine basic monitoring was established (non-invasive blood pressure, electrocardiography and pulse oximetry).
The technique of choice was neuraxial (spinal, combined spinal-epidural [CSE], epidural), provided maternal and fetal conditions allowed it.
Neuraxial anesthesia technique
L2-L3 or L3-L4 was selected as the intervertebral space for spinal, epidural or CSE puncture. A local infiltration with 2% lidocaine was used before insertion of the Tuohy N.° 18 epidural needle in the CSE and epidural techniques, while a trial dose was administered when the epidural technique was used. For CSE and spinal anesthesia, a 4 – and 3 ½" N.° 27 needle was used, respectively, with a dose of 6-10 mg of 0.5% hyperbaric bupivacaine; lidocaine with 2% epinephrine was used for the epidural technique. Additionally, neuraxial opioids (fentanyl and morphine) were used as adjuncts.
Postanesthetic recovery took place in the same operating room where the procedure was performed, with discharge criteria being Bromage = 0, Aldrete Scale 9 or higher, and absence of complications during the immediate postoperative period.
Maternal and neonatal outcomes
Data were extracted for all pregnant women with positive serology or PCR for SARS-CoV-2, including demographics, clinical characteristics (signs/symptoms, blood tests, ancillary tests such as rapid test or PCR for SARS-CoV-2), cesarean section categorization, vital signs at the beginning and the end of the surgery, type of anesthetic technique used, drugs used in anesthesia, use of vasopressors, Apgar score at 1 and 5 minutes, prophylaxis for nausea and vomiting, conversion to general anesthesia, operating time, estimated blood loss, use of uterotonics, use of blood products, use of tranexamic acid, intraoperative and postoperative complications, readmission to the operating room, and patient destination service.
Statistical analysis
Qualitative variables are presented as proportions or frequencies. The Shapiro Wilk test was used for quantitative variables in order to assess normal distribution. Results for variables with a normal distribution are expressed as means and standard deviations, while the results for variables without a normal distribution are expressed as medians and interquartile ranges. The STATA version 15 statistical software package was used for data and graph processing.
RESULTS
Clinical records of 107 pregnant women seroprevalent for SARS-CoV-2 (Figure 1) delivered by cesarean section were analyzed. Demographic, obstetrical and preoperative characteristics are shown in Table 1.
TABLE 1 Demographic and clinical characteristics of pregnant women with SARS-CoV-2.
| Characteristic or variable | Number (%) | Median or [Mean] |
|---|---|---|
| Age in years (D±SD)) | ||
| < 20 | 8(7.48) | [30.21 ± 6.89] |
| 20-34 | 67(62.62) | |
| > 35 | 32(29.91) | |
| BMI. Me(IQR) | ||
| Normal | 12(11.21) | 30.2 (26.8. 34.7) |
| Overweight | 39(36.45) | |
| Obesity I | 31(28.97) | |
| Obesity II | 14(13.08) | |
| Obesity III | 11(10.28) | |
| Gestational age in weeks Me(IQR) | ||
| Term | 85(79.44) | 39 (37.40) |
| Preterm | 22(20.56) | |
| Symptoms prior to hospitalization | ||
| Fever(n) | 4 | |
| Cough (n) | 1 | |
| Sore throat (n) | 1 | |
| Dyspnea (n) | 1 | |
| Gastrointestinal discomfort (n) | 1 | |
| Ancillary tests Rapid test | ||
| IgG+ e IgM+ | 96(89.72) | |
| IgG + | 6(5.61) | |
| IgM+ | 5(4.67) | |
| Molecular test (RT-PCR) | ||
| Positive | 1 | |
| Negative | 3 | |
| Platelet count Me(IQR) | 234.000 | |
| (191.000. 295.000) | ||
| Leukocyte count Me(IQR) | 9.700 | |
| (8.300. 11.500) |
Me: Median, IQR: Inter-quartile range, D: Mean, SD: Standard deviation n: number, BMI: body mass index
SOURCE: Authors.
Of the 107 patients, 99 (92.52%) were asymptomatic days before admission to the operating room and 8 (7.48%) were symptomatic. Fever was the most common symptom, followed equally by sore throat, cough, dyspnea and gastrointestinal discomfort.
Diagnosis was made in all cases by means of qualitative anti SARS-CoV-2 IgM and IgG antibody measurements in capillary blood. In 96 (89.72%) patients, tests were reactive for both antibodies, with only IgG reactivity in 6 (5.61%) and IgM reactivity in 5 (4.67%).
The anesthetic approach and indications for cesarean section in SARS-CoV-2 pregnant women are summarized in Table 2. The most frequent reasons for cesarean section were cephalo-pelvic disproportion (18.69%), previous cesarean section (18.69%), and non-reassuring fetal status (13.08%). SARS-CoV-2 pneumonia as a reason for cesarean section was found in only 1.87% of cases. Prophylaxis for postoperative nausea and vomiting in the operating room (dexamethasone alone in 28.97%, ondansentron alone in 22.43% and both medications in 44.86%) was used in 103 (96.26%) patients. As for oxygen therapy on admission to the operating room, only two patients required oxygen (binasal cannula in one case and bag mask in the other case).
TABLE 2 Anesthesia technique and indication for cesarean section in SARS-CoV-2 pregnant women.
| Characteristic or variable | Number(%) |
|---|---|
| Reason for cesarean section | |
| Cephalo-pelvic disproportion | 20 (18.69) |
| Previous cesarean section | 20 (18.69 |
| Non-reassuring fetal status | 14 (13.08) |
| Hypertensive disorder of pregnancy | 13 (12.15) |
| Pneumonia | 2 (1.87) |
| Other causes | 38 (35.52) |
| ASA physical condition | |
| II | 87 (81.31) |
| III | 20 (18.69) |
| Cesarean section classification according to the Lucas classification | |
| Category 1 | 6 (5.61) |
| Category 2 | 48(44.86) |
| Category 3 | 47 (43.93) |
| Category 4 | 6 (5.61) |
| Nausea and vomiting prophylaxis | |
| None | 4 (3.74) |
| Dexamethasone | 31 (28.97) |
| Ondansetron | 24 (22.43) |
| Dexamethasone+ondansetron | 48(44.86) |
| Oxygen therapy | |
| Binasal cannula | 1 |
| Non-rebreather mask | 1 |
| Anesthetic technique | |
| Neuraxial | 107 (100) |
| - Spinal | 100 (93.5) |
| - CSE | 4 (3.7) |
| - Epidural | 3(2.8) |
| Dose of 0.5% hyperbaric bupivacaine | |
| 6 mg | 1 (0.96) |
| 7 mg | 23 (22.12) |
| 7,5 mg | 5 (4.81) |
| 8 mg | 34 (32.69) |
| 9 mg | 24 (23.08) |
| 10 mg | 17 (16.35) |
| Use of neuraxial adjuncts | |
| Fentanyl | 92 (85.98) |
| Morphine | 101(94.39) |
| Use of vasopressors | |
| None | 91(85.05) |
| Prophylactic | 8(7.48) |
| Treatment | 8(7.48) |
| Anesthetic complications | |
| None | 102 (95.33) |
| Shivering | 4 (3.74) |
| Pruritus | 1(0.93) |
ASA: American Society of Anesthesiologist.
SOURCE: Authors.
The anesthetic technique at the start of the cesarean section was neuraxial in all cases; single-dose spinal anesthesia was used in 100 (93.5%) patients and the CSE and epidural techniques were used in a lower percentage of cases (Figure 2). Motor and sensory block was achieved from T4-T5 to S4-S5 with all the techniques.
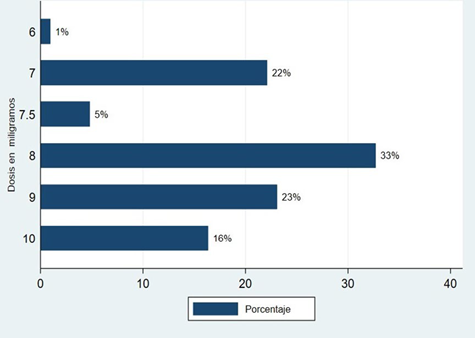
For the spinal block, the local anesthetic used was 0.5% hyperbaric bupivacaine at doses ranging between 6 and 10 mg. The most frequently used dose was 8 mg (32.69%), followed by the 9 mg dose (23.08%), as shown in Figure 3. Regarding neuraxial adjuvants, fentanyl was used in 92 patients (85.98%) and morphine was used in 101 (94.39%). Likewise, 91 (85.05%) patients did not receive vasopressors to prevent or treat the hypotension induced by the spinal block, 7.48% received prophylactic intravenous ethylephrine infusion, and rescue boluses were used in the same percentage of patients.
Medians as well as minimum and maximum vital sign values (heart rate, systolic blood pressure, oxygen saturation and respiratory rate) on arrival to, and exit from, the operating room are shown in Figure 4, highlighting minimum variation between values.
Table 3 shows the relationship with surgical and neonatal outcomes. Median surgical time was 42 minutes (IQR 3050 min). Median APGAR scores at 1 and 5 minutes after birth were 8 and 9, respectively.
TABLE 3 Surgical and neonatal outcomes in SARS-CoV-2 pregnant women.
| Characteristic or Variable | Number (%) | Median (IQR) |
|---|---|---|
| Surgical time in minutes Me (IQR) | 42 (30. 50) | |
| Blood loss | ||
| >1 000 ml | 2(2.8) | |
| < 1 000 ml | 104 (97.19) | |
| Use of uterutonic agents | ||
| Oxytocin | 37 (34.58) | |
| Oxytocin+ergometrine | 31 (28.97) | |
| Carbetocin+ergometrine | 13 (12.15) | |
| Oxytocin+ergometrine+misoprostol | 12 (11.21) | |
| Newborn Apgar score Me(IQR) | ||
| 1 minute | 8 (8.8) | |
| 5 minutes | 9 (9.9) | |
| Patient destination | ||
| Inpatient ward | 105 (98.13) | |
| Intensive care unit | 2 (1.77) | |
| Obstetric complications | ||
| Uterine hypotonia | 14 (13.08) | |
| Conversion to hysterectomy | 3 (2.80) | |
| Use of blood products | 3 (2.80) | |
| Use of tranexamic acid | 2 (1.87) |
M e : Median, IQR: Inter-quartile range.
SOURCE: Authors.
There was no intraoperative need to convert to general anesthesia; conversion to hysterectomy was required only in 3 patients and 2 of them needed blood product transfusions. Tranexamic acid was used in 5 patients (4.67%) and no thromboembolic events had been reported up until 72 hours after surgery. Only 1 patient received preoperative pharmacological thromboprophylaxis.
Two patients developed intraoperative pneumonia and one of them was transferred to the ICU after the surgery.
Moreover, 14 patients had hypotoniaatony and 3 of them underwent hysterectomy. One of these three patients was transferred to the ICU at the end of the surgical reintervention. The remaining 105 (98.13%) patients were transferred to hospitalization at the end of the post-anesthesia recovery period. No deaths had occurred up until the third postoperative day.
DISCUSSION
This work found that pregnant women were asymptomatic in 92.52% of cases, while 7.48% showed mild symptoms before hospitalization, with fever being present in the highest proportion. Gao et al. 5 report that symptoms such as fever (51%) and cough (31%) in pregnant women with COVID-19 were lower than in non-pregnant women (91% and 67%, respectively), which could we attributed to changes in the immune system of the pregnant women.
Symptoms prior to hospitalization and the rapid antibody test for SARS-CoV-2 were considered in the diagnosis of SARS-CoV-2 infection in this study. Oropharyngeal swab for RT-PCR was done in 4 of the 8 symptomatic patients with a positive rapid test, with 1 being reactive.
At the beginning of the pandemic, similar to several other countries in Latin America, the Ministry ofHealth in our country considered that the diagnosis should be based on the epidemiological background and individual patient characteristics, and that it should be confirmed with laboratory tests such as the rapid test for SARS-CoV-2 antibodies or RT-PCR.
In their study of SARS-CoV-2 prevalence carried out over a similar period of time, Flannery et al. 6 found in 1,293 pregnant women in Philadelphia that out of 72 seropositive women, only 46 were reactive on RT-PCR, while out of 1,037 seronegative women, only 18 were reactive on RT-PCR. Hence the need for further infection time studies between seropositivity and positive RT-PCR of SARS-CoV-2 infection in pregnant women. Likewise, Vidal et al. 7 report that both tests need to be complementary because of their diagnostic ability as a function of infection time.
Regarding the reason for cesarean section, it was found that the most frequent causes were cephalo-pelvic disproportion, previous cesarean section and non-reassuring fetal status. Similar results were described by Cao et al. 8, where 2 out of 8 patients (25%) required emergency cesarean section due to non-reassuring fetal status and the other 6 included diagnoses such as previous cesarean section, preeclampsia, among others. Unlike the case series by Chen et al.9 in which only 18% (3 pregnant women out of 17) required emergency cesarean section.
In this work, SARS-CoV-2 pneumonia was present in 1.87% of cases, resulting in an indication for cesarean section. This is in contrast with the study by Turan et al. 10, in which SARS-CoV-2 infection was the reason for cesarean section in 49.6% of preterm deliveries despite the absence of maternal or fetal risk. In 65.7% of term deliveries, COVID-29 was the indication for cesarean section. These figures show that the differences found were due to the fact that the SARS-CoV-2 infection was considered an indication for cesarean section, which was not the case in our study.
The anesthetic technique at the initiation of the cesarean section was neuraxial in all cases, with the single-dose technique used in the vast majority of patients. In a large case series, Zhong et al. 11 found that spinal anesthesia was used safely in 91.84% of their patients. In the study by Chen et al. 9, 18% of the pregnant women received general anesthesia, and 82% received anesthesia through epidural catheter, while in the study by Yue et al.12, the CSE technique was used in 30 patients, none of whom required general anesthesia. The difference with the study by Chen was that general anesthesia was selected due to fetal compromise that required immediate anesthetic approach. These results show that the neuraxial technique was safe in these patients.
Regarding the use of uterotonics, Bauer et al. 13 published in a review article the recommendation on the use of oxytocin or oxytocin derivatives (carbetocin) as first line drug and ergometrine as second line agent in these patients; in this study, oxytocin or carbetocin were used in 100% of patients as first-line drug, while misoprostol was used only in 7.5% of patients who needed a second line agent. As for costs, in a case report at the beginning of the pandemic, Landau et al. 14 described bronchospasm as a complication related to the use of prostaglandins (misoprostol), requiring airway management or orotracheal intubation and increasing the risk of infection for the attending staff.
Postpartum bleeding is one of the main causes of morbidity and mortality in pregnant women, and cannot be neglected when analyzing the impact of the pandemic. In relation to estimated bleeding during cesarean section, Yue et al. 12 published a study on the anesthetic management of 30 patients with confirmed or suspected COVID-19 infection in which they found greater blood loss among confirmed cases (334,7±63.3), than in suspected cases (293,8±25); although this difference in not clinically relevant, estimated bleeding in this study was very similar (500 mL [IQR 500, 600]).
Turan et al. 10 found 6 cases of postpartum bleeding with more than 1,000 mL of blood loss during cesarean section in 637 patients (0.9%). Three of them had severe COVID-19 infection, one of them developed coagulopathy, while the remaining two showed mild symptoms. This study found some degree of uterine hypotonia in 14 patients during surgery, but only 3 patients (2.8%) had bleeding of more than 1,000 mL. Of the three patients with postpartum bleeding, two were morbidly obese and were of advanced maternal age (44 years), while the third patient had dyspnea and required oxygen supplementation on arrival at the operating room. Blood products and tranexamic acid were used in two patients and total abdominal hysterectomy was performed in three patients.
The use of nausea and vomiting prophylaxis in these patients is crucial due to the risk of contamination during the intraoperative and immediate postoperative periods; this work found that 96.26% of the patients received some form of pharmacological prophylaxis for this end.
In various publications, one of the main controversies has to do with the relationship between SARS-CoV-2 infection in the pregnant woman and maternal death. Zaigham et al.15, in a systematic review of 18 articles including a total of 108 pregnant women (very similar number to that of this work), did not report any maternal deaths. In a more extensive review of 63 observational studies with a total of 637 patients, the reported incidence was 1.6% (10 maternal deaths), of which 2 patients were older than 40 years of age, while another 2 were obese and diabetic 10. A more extensive meta-analysis published in September described an even lower incidence of 0.1% (73 maternal deaths out of 11,580 pregnant women with COVID-19 infection) 16. This work did not find any cases of maternal death in the 72 hours following cesarean section, albeit with no follow-up beyond that time.
One of the signs of severity of the infection is the development of pneumonia requiring oxygen supplementation. In their review, Zaigham et al. 15 found that 2 out of 108 patients (1.85%) who developed acute respiratory distress syndrome required orotraheal intubation and mechanical ventilation. In this work, two patients developed pneumonia during the perioperative period and required oxygen supplementation, and one of them needed to be transferred to the intensive care unit postoperatively. Those two patients were under 35 years of age and were delivered pre-term, at 32 and 35 weeks of gestational age.
Although pregnancy is known to be a hypercoagulable state characterized by an elevation of prothrombotic factors, no increased risk of thromboembolic events has yet been shown in the current literature of pregnant patients admitted with COVID-19 when compared with non-pregnant patients infected by this same virus 17. No thromboembolic events were found in this work up until the third postoperative day. Nonetheless, risk stratification, especially in this group of patients, is of the utmost importance.
Outcomes for the newborns are a source of concern in this setting. In their review, Turan et al. 10 found low Apgar scores (below 7 at 1 and 5 minutes of life) in 6 out of 361 neonates (1.7%) reported across 29 studies. They were all preterm babies delivered because of loss of fetal wellbeing secondary to COVID-19 compromise in the mothers. In this review, we found 5 neonates (4.7%) with Apgar scores below 8 at 5 minutes of life, but two of them had a diagnosis of fetal malformations before admission to the operating room, while the reason for cesarean section in the remaining four cases were equally distributed between non-reassuring fetal status and cephalo-pelvic disproportion. They were are all term babies and only one of the mothers had respiratory distress requiring oxygen. The other mothers did not have any symptoms of the disease.
The main strength of this work is sample size when compared with other world studies on perioperative anesthetic management. Additional strengths include the analysis based on current evidence of clinical characteristics, perioperative anesthetic management and complications in pregnant women with serological identification of SARS-CoV-2 infection.
The main weaknesses include time, the use of convenience sampling and the small number or molecular RT-PCR tests available. As far as the latter is concerned, we are aware that the reference standard recommended by the WHO for the diagnosis of SARS-CoV-2 infection is real-time reverse transcription- polymerase chain reaction 18.
In April 2020, Vidal-Anzardo et al. published a research study comparing rapid serological tests with molecular tests, used in Peru in field conditions, in terms of diagnostic yield, sensitivity and specificity. For serological tests, sensitivity was 43.8% (95% CI [19.8-70.1]), which increased gradually over time, with 0% identification in the first week, 33.3% in the second week and 50% beyond that time, while specificity was 98.9% (95% CI [94.0-100]) 7. For the molecular RT-PCR test, sensitivity was 69.2% in the first week, but dropped to 25% by the second week and down to 13% beyond that time 5.
Consequently, the serological test becomes important as a complement to the molecular test after the second and third week of the infection.
Despite the challenges described above, it may be concluded from this study that the majority of pregnant women with SARS-CoV-2 infection are asymptomatic and that neuraxial anesthesia, including spinal, combined spinal-epidural and epidural, were found to be safe techniques for these patients and their newborn babies.
Ethics committee endorsement
This study was approved by the Ethics Committee of the National Maternal Perinatal Institute during a meeting held on July 8, 2020, as evidenced in Letter N.° 048-2020-DG-N°015-OEAIDE/INMP.
Human and animal protection
The authors declare that no human or animal experiments were carried out as part of this research.
Data confidentiality
The authors declare that they have followed the protocols of their institution on patient data disclosure.











 text in
text in