Introduction
The onset of pressure ulcers (PU) is consequential of ischemic necrosis at skin level and subcutaneous tissue, produced by pressure exerted upon over a bony prominence.(1) Pressure ulcers are considered adverse events that further complicate the critical state of patients hospitalized with high-complexity problems, causing deaths associated to infection and sepsis. Studies of PU prevalence in hospitals in Europe, Canada, and the United States indicate a variation between 8.3% and 23%, with nearly two in every three a product of prolonged hospitalizations.(2,3) Studies of PU prevalence in hospitals in Colombia reveal a variation between 2.2% and 10%.(3)
Data indicate that 60% of ulcers are developed in intensive and chronic care units during the first two weeks of hospitalization and their risk increases by 74% when combined with the presence of factors, like immobility, alteration of the immune system and loss of body mass.(3-5) Other determining factors of the risk are humidity, excoriation, and capillary lesion of the skin.(6) Pressure on bony protrusions is the condition to produce these ulcers and among the sites of highest prevalence there are the heels, malleolus, trochanters, elbows, gluteus, and sacrum.(5-7) Death has been described associated to pressure ulcers when these lead to problems, like important sepsis related to infection of the lesion.(5,7)
The impact of the onset of PU not only affects the quality of life of the individuals and their families, but also the health systems. Costs in preventing and treating PU constitute a high burden for health systems throughout the world, so that the general cost of treating a PU is approximately US$70 000, with an estimated annual cost between 2.2 and 3.6 billion US dollars.(4-7) Prevention of the onset of PU means a priority in national and international public health, in terms of the patient’s quality results.(8-10)
Recommendations based on evidence on interventions through conventional care and more specialized care, like using dressings in preventing PU, have been evaluated in the Clinical Practice Guides in Nursing by the Registered Nurses´ Association of Ontario (RNAO),(11) which are being implemented in our institution and show the best evidence available on all the interventions and care on PU prevention.(11) However, evidence on the effectiveness of other devices used in PU prevention is limited (low-moderate level of evidence), as is the case of using skin protectors, which have been the product of research aimed more toward healing PU, and have been progressively promoted for use in prevention.(12) Included among some of these products or devices, there are semipermeable skin protectors or dressings (polyurethane), padded dressings (hydrophobic, polyurethane), and hydrocolloid dressings (HD) (containing gelatin, pectin, carboxyl-methylcellulose).(13,14). A high degree of uncertainty exist on the preventive effectiveness of the dressings and their use associated to high costs per unit in health institutions for critical patients with prolonged hospital stay.(15)
Given that uncertainty prevails about the benefit of using skin dressings in preventing PU, the aim of our study was to estimate the association between exposure to using hydrocolloid dressings plus conventional care (HD+CC) compared to using only conventional care (CC) and PU incidence in adult patients, evaluated with high risk for pressure ulcer, included in the skin care program in a tier IV hospital through a retrospective study.
Methods
A retrospective cohort study was carried out. The study universe included adult patients with cardiovascular problems admitted to a private, high-complexity care foundation hospital in Bogotá D.C, Colombia. The population was comprised by 1461 clinical records from patients over 18 years of age admitted between June and December 2014; it was limited to patients admitted to hospitalization at risk of PU, but with intact skin, to any unit or care service during this period, and who had complete assessment record by the nursing staff from the Institutional Program on Prevention of Pressure Ulcers and Skin Care (PPCP, for the term in Spanish). This program seeks to administer preventive skin interventions on individuals at risk and conduct treatment in patients with wounds, ulcers, or other skin lesions. However, the preventive care strategies were begun within the program after the period of implementing the recommendations of a Clinical Practice Guide on the Prevention of Pressure Ulcers conducted between January and June 2014.(11)
The eligible population was made up of the clinical records from 170 patients over 18 years of age from both genders, who were hospitalized in any unit or intensive care service, with intact skin on admission to the PPCP, with a high or very high score of PU risk, according to the Braden scale (16) and who had been evaluated by the PPCP staff with a complete registry of the program variables, according to the clinical practice prevention guide.(11) These patients received the prescription of care prescribed in the clinical record based on the patient evaluation and according to the clinical decision made by the program’s nursing staff along with each patient’s treating physician. This prescription consisted in protecting at least one healthy area at risk with a) hydrocolloid dressing plus conventional care or b) only preventive conventional care (use of moisturizing lotion, changes of position, use of support surfaces or pressure regulating pillows, and anti-decubitus mattress).
The time during which the PU events stage I to stage IV (time to event) occurred was evaluated after admission to the PPCP. Both the confirmation of the ulcer and its degree of complication (Stage I to Stage IV, according to the National Pressure Ulcer Advisory Panel, NPUAP)1 were identified through the note on the clinical record made by the expert from the PPCP, who reported if the lesion appeared in a protected zone through any of both treatments studied. Discharge information was included by the PPCP group, given by the date of death or from the hospital discharge.
To conduct this study, information consigned in the clinical record was obtained, which included socio-demographic variables (age, gender, educational level, type of occupation, and place of origin); related to the prior health status (antecedents, comorbidities, prior PU development); related to hospital admission and evolution of the health status (admission diagnosis, hospitalization service, areas of the skin at risk of PU, score on the Braden scale, complications, date of PU onset, stage of the ulcer, its location, time of hospital stay).
Bivariate analysis was performed to compare las characteristics basales between the treatment groups, using Student’s t test for difference of means and the Chi squared test for difference of proportions. Incidence and behavior were estimated in function of the risk of PU onset in the study groups by using the Kaplan-Meier risk estimator. The association between the type of treatment and PU onset in the protected zones was estimated through Hazard Ratio with 95% confidence intervals, through raw estimation and a multivariate analysis with the Cox proportional risk model, adjusting for the co-variables identified as significant in the bivariate analysis (p<0.05), which were possible effect modifiers. This study was approved by the ethics committee in the participating hospital institution, as a preliminary phase included in the Pressure Ulcer Nursing Prevention study (PENFUP study).
Results
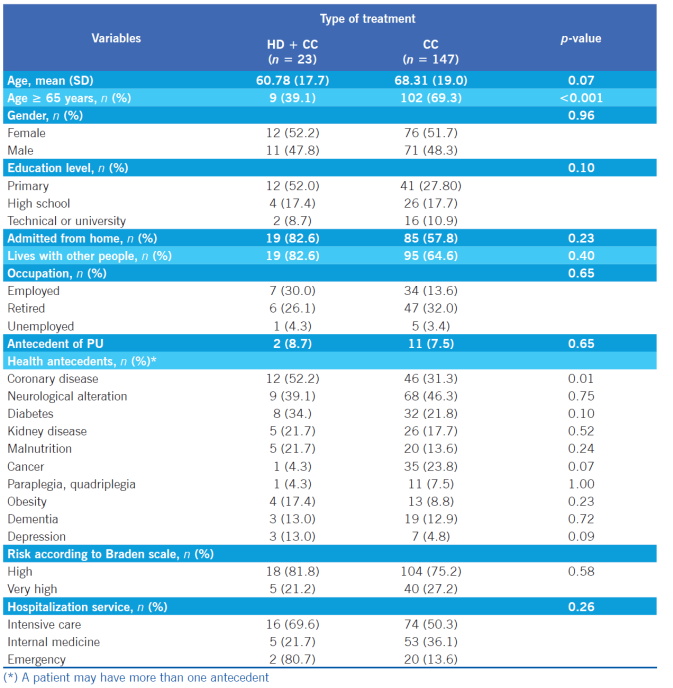
Of the total number of patients included (n=170), 23 received the HD+CC preventive treatment and 147 were administered only CC. The frequency of patients ≥ 65 years of age was significantly higher in the CC group compared to the HD+CC group (69.3 versus 39.1, p<0.001). It was generally observed that the groups were equal regarding the frequency distribution of participants in the variables for gender, educational level, place of origin, living with other people, and occupation between both groups. In relation to the evaluation of health antecedents, significant differences were also not observed related to prior PU presentation, or in terms of risk evaluated according to the Braden scale or according to the type of service to which the patients were admitted between both groups of care. Patients were hospitalized in a large proportion in an intensive care service in both groups without significant differences. Regarding health antecedents and comorbidities, a higher significant frequency was observed of patients with coronary disease in the group receiving care with HD+CC compared to the group with only CC, respectively (52.2% versus 31.3%, p=0.01) (Table 1).
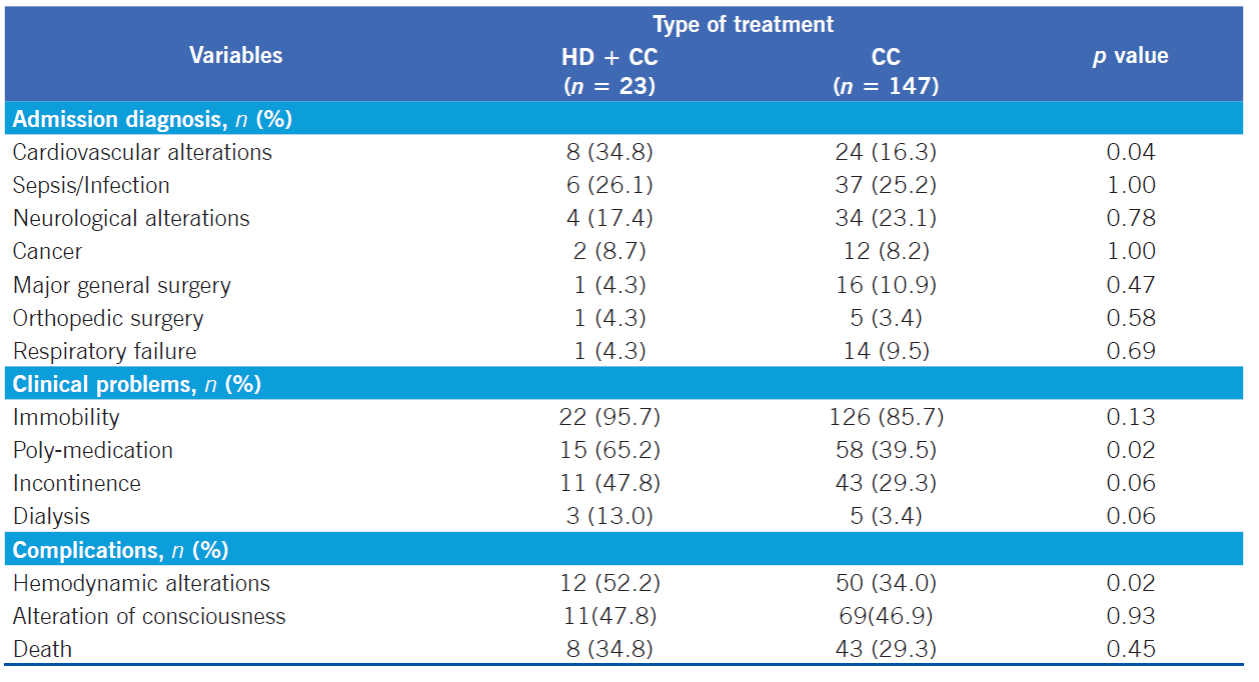
In relation to the admission diagnosis and clinical evolution of the patients during hospitalization, a higher frequency was noted of patients admitted due to cardiovascular causes or alterations in the group receiving HD+CC compared to the CC group (34.8% versus 16.3, p=0.04). Likewise, HD+CC patients had greater hemodynamic complications (52.2% versus 34.0%, p=0.02) and were exposed to greater poly-medication (65.2% versus 39.5%, p=0.02) than the CC patients. Although no significant differences were present, a higher frequency was observed in the HD+CC group compared to the CC group in the variables of immobility (95.7% versus 85.7%) and incontinence (47.8 versus 29.3) (Table 2).
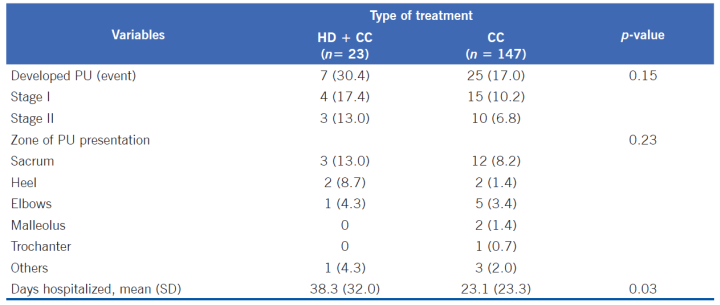
Although no statistical difference was found, the PU incidence was higher in the group receiving preventive treatment in the areas protected with HD+CC (30.4%) compared to the group with only CC (17%). In both groups, PU were evaluated as stage I or II, without difference in the proportion of contribution from each of them in each group. The average number of days of hospital stay was significantly higher in the group protected with HD+CC (38.2±32) versus the group protected with CC (23.1±23.3), with this difference being of 15.2 days. Although no significant differences were identified per zones of PU presentation, it was observed that PU incidence was higher in the sacrum, heels, and elbows in patients protected with HD+CC compared to those who received CC (Table 3).
Figure 1 shows the comparison of the Kaplan-Meier curves in function of time to the event due to PU, which are quite similar during the first 12 days in both treatment groups. This trend is reflected in the Kaplan-Meier survival analysis curves that are not statistically different through the Log-Rank test (p=0.482) (Figure 1).
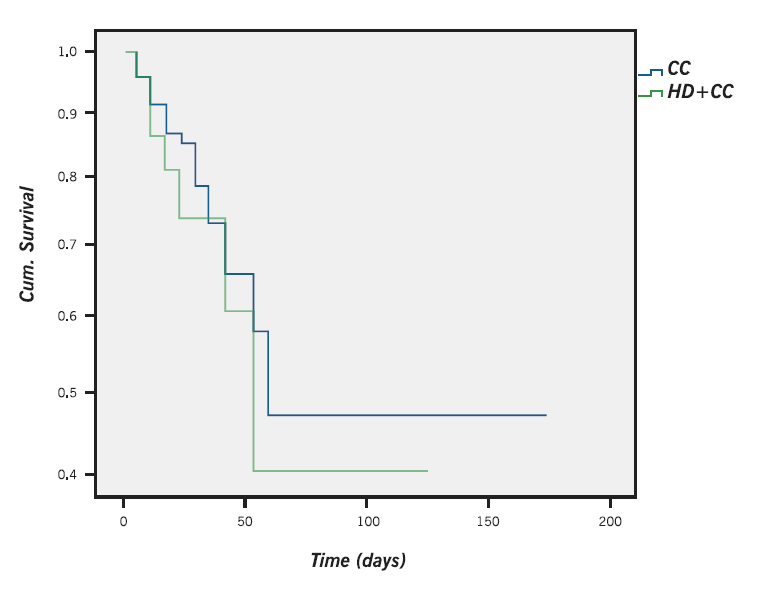
Figure 1 Kaplan-Meier estimations for the time in developing PU in patients, according to preventive treatment group
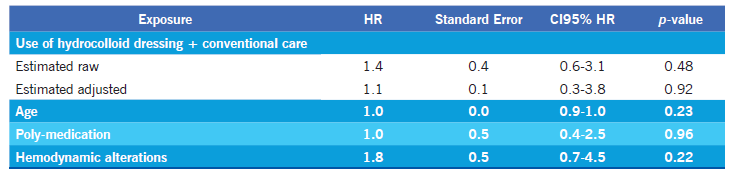
To examine the association between using the preventive treatments studied and development of PU, the raw HR was compared to the adjusted HR, showing no significant difference between both. Additionally, the Cox multivariate proportional-hazards model revealed that the variables of age, poly-medication, and hemodynamic alterations were not effect modifiers (Table 4).
Discussion
The findings from our study show no differences between using hydrocolloid dressings plus conventional care and using only conventional care in preventing the onset of pressure ulcers in adult patients hospitalized with high risk of developing these events. Given that no differences were observed in the benefit between one and the other preventive strategy, what the evidence shows is the promotion of higher-scale studies that permit evaluating their real impact in clinical care.
The presence of pressure ulcers can be explained by factors related to the patients’ age and their physiopathological condition.17 The results from our study are similar to the results described in other studies regarding the presence of factors related to PU, like age (elderly adults), coronary disease with possible alteration of consciousness associated to an alteration of the hemodynamic state, which also lead to immobility and limited tissue perfusion.18 Patients described in the group of preventive care with dressings had significant differences related to antecedents of coronary disease and also had greater hemodynamic alterations and poly-medication, accounting for the severity of the patients in this group, which could lead to greater complications and to a prolongation of their hospital stay. Cardiovascular problems with hemodynamic alterations are characterized for having low cardiac output and consequently have hypo-perfusion in all bodily organs, including the skin. Additionally, medications that improve cardiac output do so at the expense of tissue vasoconstriction to improve it, producing peripheral hypoxia with repercussions on the skin.17,19
Hemodynamic problems may lead to an altered state of consciousness, as was the case of patients hospitalized in the HD+CC group, which led to two important problems related with PU onset: incontinence and immobility. In general, incontinence is managed by the nursing staff by using diapers that, if not controlled adequately, produce lesions associated to chronic moisture that can be confused for pressure ulcers.12 Our study could not ensure existence of this confusion, given by the prevalence of stage I and stage II PU. The presence of pressure ulcers of a minor stage in our patients has been associated in our hospital to the implementation of the Clinical Practice Guide by the RNAO on PU prevention, which has permitted greater control of patients at risk through systemic evaluation by using the Braden scale, along with continuous evaluation of the record of events in all care services.20) Another factor identified in our study, which requires a wake-up call is obesity; although it did not show significant differences, it was observed with higher frequency in patients receiving HD+CC compared to the group receiving only CC. This factor is important, given that it has been evidenced in literature that it can lead to greater complications and prolongation of the hospital stay, while becoming a challenge in terms of mobilization for health caregivers.21
Although using dressings in caring for wounds or ulcers already formed has proven its healing benefit, limited valid and reliable evidence exists with respect to their effectiveness or the conventional care measures to prevent pressure ulcers. Published data available from other research present serious limitations in the design and methods, thus, limiting their results from being the base to implement these prevention strategies.14,22,23 Even so, some studies reveal results similar to ours, showing no differences between groups exposed to using HD compared to CC: Dutra et al.,24 found that PU incidence was higher in the group using HD (15%) compared to the group receiving preventive care with another type of protection (8.7%). The study by Walker et al.,15 reported no difference between using HD compared to CC (RR=0.73, CI95% =0.18-3.05).
Given the need to reduce adverse events because they are associated to increased care costs and to complications in the patient’s health,25 it is necessary for the use of PU preventive measures to be based on scientific evidence that proves the real benefit. In the specific case of the HD, the Consensus of Wound Healing Societies16 speaks of the uncertainty associated to the methodological limitations reported in studies with evidence in favor of hydrocolloid dressings, but - in turn - reflects the need to perform clinical trials to evaluate diverse preventive care strategies. Likewise, this Consensus recommends the continued use of conventional care strategies, like rotating patients per schedule and using support surfaces to reduce pressure on bony protuberances, friction and rubbing, and using moisturizing lotion without rubdowns.12 These recommendations coincide with those provided by the Pressure Ulcer Prevention Guide, implemented in our institution, which describes effective interventions with only using gel dressings in patients during prolonged surgeries, as well as using specific mattresses for each type of risk according to the Braden scale, which are very costly strategies for our country.11 The use of conventional care preventive measures was implemented in our hospital since 2014 and these are combined with the use of hydrocolloid dressings as deemed by the nursing staff, in spite of the uncertainty about their effectiveness.
The limitations in this cohort study are given by the use of retrospective information obtained directly from the patient’s clinical record, and although the group of nurses from the PPCP program is expert in skin wounds and lesions, it is not possible to establish the confirmation of the events investigated. Use of HD could have increased the confidence of the nursing staff in this intervention, keeping CC activities from being carried out, like mobilization and application of measure to reduce pressure with pillows. The conclusion in this study is that using HD+CC did not show superiority against CC in preventing PU in adult patients at high risk, according to the Braden scale. Our results show the need to perform well-designed clinical trials and of sufficient population size to evaluate the impact of using hydrocolloid dressings compared to conventional care in PU prevention.











 text in
text in