Introduction
Lower-limb ulcer of venous etiology (UVE) is a chronic disease evidenced by trophic lesions of the skin and the subcutaneous cell tissue, originated as consequence of the endogenous affection induced and maintained by high venous pressure. It is of frequent appearance, with preference for the elderly and occurs much more than that of ischemic or neuropathic type. It is defined as “a solution of cutaneous coverage continuity with loss of substance, which exposes the underlying tissues to a variable depth, related etiologically with a venous pathology determinant of ambulatory hypertension in the lower limbs, with scarce tendency to spontaneous cicatrization, chronic evolution, and high tendency to recurrence”.1 The UVE can be varicose, postphlebitic or post-thrombotic or through combination of these,2 localized generally below the knee, almost always perimalleolar. The lesion denotes histological and structural changes of the vascular and lymphatic wall. These modifications produce physiological alterations, like capillary leak, fibrin deposition, sequestration of leukocytes and erythrocytes, thrombocytosis, and inflammation, which harms oxygenation of the skin and nearby tissue, favoring tissue hypoxia.3
Care of patients suffering from UVE requires an evaluation and specialized treatment and, on occasion, interdisciplinary due to the multi-causal origin, manifestations on skin, cardiovascular compromise, magnitude and consequence of the damage. Besides the bodily affection, it compromises the quality of life of those who suffer it in the emotional, spiritual, social, and aesthetic dimensions,4 specifically due to issues associated to constant pain, deterioration of the bodily image, isolation, and difficulty in performing daily living activities. Furthermore, no care or deficient approach generate increased costs due to loss of working capacity, constant institutional readmissions, and high expenditures of health resources, in addition to the possible recurrence if efficient measures are not interposed.
Diverse risk factors have been described that favor the appearance of the wound; among them, those inherent to the physiopathology.5-7 Fukaya and Margolis8 consider, among others, immobility, obesity, rigidity of the ankle and deterioration of the calf muscle pump, which facilitate the appearance of varicose veins compromising blood irrigation systems. Some authors9 hold that the most common factors are advanced age, family background of venous disease, increased body mass index, smoking, antecedents of traumatism, and prior venous thrombosis; they have also considered the patient’s social history through characteristics of age, education, occupation, income, postural positions maintained, and access to care.10
Regarding its epidemiology, between 70% and 80% of lower-limb ulcers are of venous etiology.11,12 Pannier and Rabe13 found in the general population between 18 and 79 years of age a prevalence of 0.6% of healed UVE and 0.1% of active wounds. The National Conference on Consensus of lower-limb ulcers11 reports a population prevalence between 0.5% and 0.8% with an annual incidence between 2 and 5 cases for every 1000 people/year. With respect to its chronicity, it is estimated that between 40% and 50% of the wounds remain open or active for a period no less than 6 or 12 months; additionally, average times of recurrence of 42 weeks have been found, with an incidence of 22% of recurrence at three months, 39% at six months, 57% at 12 months, and 78% at three years.14 For the Latin American population no reliable data is available on its incidence or prevalence, but it is estimated that the latter can be between 3% and 6%.1 In Colombia, within a population prevalence of wounds of 5.2%, the UVE correspond to 14.6% of that value.15 Information is still scarce about UVE in the regional and national contexts, which is why we must advance on the description of the chronic process of these lesions.
The objective of this study was to establish the relationship between the sociodemographic and clinical factors with cicatrization success in patients with UVE. This study is important for the nursing profession because, in our context, nurses are responsible for providing care to patients who suffer it and knowledge of the factors related with the UVE cicatrization process will contribute to promoting interventions that lead to the decrease of its presentation and recurrence.
Methods
A cohort type, prospective observational study was conducted with the participation of 80 patients with UVE who were monitored for up to 13 months. The sampling was non-probabilistic, intentional. Selection of participants was conducted in three clinics in the city of Medellín (Colombia) with specialized nursing care in treating vascular wounds. The study included patients with controlled chronic pathologies, without neurological compromise, with diagnosis of varicose and traumatic UVE by a physician or by a nursing professional specialized in wounds. All the participants had at least one wound complying with the classification criteria of venous classification, according to ultrasound record or clinical diagnosis - in case the patient had more than one UVE, the decision was made to evaluate and monitor the bigger wound and its satellite wound. The study excluded patients with presence of mixed ulcer, those in which there was no certainty that their diagnosis corresponded to UVE, those who abandoned treatment, and those showed intolerance with the use of compression bandage (treatment received). Every patient identified as potential participant was invited to partake in the study and was explained the reasons and benefits; none denied participation.
Information was gathered between September 2014 and October 2015. It was possible to observe the evolution of the UVE, considering at least five observation times (T0 -basal-, T1, T2, T3, and T4), with a difference of no less than 25 days between one evaluation and the other. The wound nurse at the clinic performed all the evaluations and healing, and used different technological dressings according to the wound’s cicatrization stage; nevertheless, all the patients received compression bandages as part of the common treatment during follow up. To evaluate the stage and evolution of the UVE, the treating nurse along with the researcher applied the Resvech 2.0 instrument,16 a scale that measures improvement in the cicatrization process from 0 to 35, with the lowest scores indicating improvement. When tabulating the information from the instrument, infection and inflammation characteristics were recorded individually. To compare differences in cicatrization according to wound size, these were considered small when measuring ≤15.9 cm2, medium from 16 to 63.9 cm2, and large from 64 cm2 and above.
For the statistical management of the data, a univariate analysis was used to calculate the frequency distributions of qualitative-type variables and for data of quantitative nature, normality tests were conducted with the statistical distribution function through the Kolmogorov-Smirnov test with Lilliefors correction. The survival analysis considered as result variable the cicatrization success, which was defined as the complete cure of the wound in a time ≤90 days, evidenced by the presence of intact healed skin, absence of edges and absence of wound exudate. The model included those variables complying with statistical significance, biological plausibility or according to the Hosmer-Lemeshow criterion (p≤0.25). Censored data corresponded to five patients who quit the study, and four who - upon ending the study - did not achieve cicatrization.
To estimate cicatrization in function of time, the Kaplan-Meier method was used and the Logrank test was used for hypothesis contrast in comparison of two or more groups. The independent variables were dichotomized to define their input to the proportional risk model, thus: compromise of the wound Resvech score: slight = ≤15 points and high = >15; nurse experience in wound clinic: ≥5 years and <5 years; socioeconomic level: low = ≤2 and high = 3 and more; age of patient: ≤65 years and 66 and more years. The model also included the variables of gender and time in days since the appearance of the ulcer due to the clinical importance they represented. The Cox proportional risk model was carried out to study the multivariate effect on cicatrization over time. The statistical software used to process the information was Stata v.12.0. The research was approved by the Ethics and Research committees of the National Faculty of Public health at Universidad de Antioquia and of the three clinics where the data were collected. All participants signed the informed consent.
Results
The study evaluated 80 patients with UVE. All had at least one UVE, with a median of six months of antiquity. Table 1 shows the general characteristics of the participants. There was prevalence of female participants, married, low socioeconomic level, low schooling, and housekeeper as occupation. The mean age for this group was 65 years (minimum = 18 and maximum = 90). In life habits, there was higher frequency of tobacco consumption than alcohol, poor consumption of fruits and vegetables, high intake of beef and pork, as well as poor engagement in physical activity.
The 62.5% of the participants were treated by a nurse with experience of five and more years in wound clinic; 55% of the participants had a relative in charge of home care. It was evidenced that 73.8% had weight alterations; additionally, 77.5% suffered hypertension; 53.8% had a Yao index between 0.7 and 1.30. The most frequent antecedent was that of suffering from varicose veins (86.3%), followed by arterial hypertension (63.7%). Additionally, it was found that 66.3% of the participants had already had an episode of UVE; inclusively, 19 people had had more than three recurrences. In all, 39.6% manifested that these wounds had healed in ≤4 months. The most frequent location of the current wound was the internal malleolar (33.7%), with prevalence of the lower left limb (58.8%) (Table 2).
Table 2 Personal and family background, current clinical and wound characteristics of 80 patients diagnosed with ulcer of venous etiology

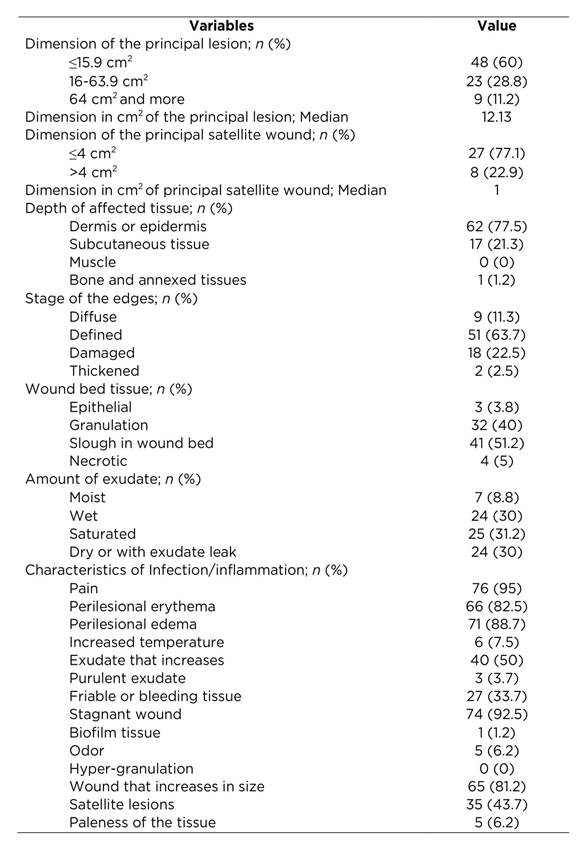
Table 3 shows information of the UVE during basal evaluation. It was found that 60% of these wounds measured less than 16 cm2; the greatest affection occurred in the epidermis (77.5%), defined edges were present in 63.7%, slough was found in the wound in 51.2%, and 31.2% had saturated exudate. Infection and inflammation characteristics showed that the wound caused pain (95%), with erythema and perilesional edema (82.5% and 88.7%, respectively). Likewise, other characteristics were found, like presence of wound that did not diminish in size in 92.5% and wound that increases in size in 81.2% of the patients.
Table 3 Basal evaluation of the wound in 80 patients diagnosed with ulcer of venous etiology according to the Resvech 2.0 instrument
The cicatrization process was analyzed during all the evaluation times. Graphic 1 shows that change in wound size was bigger between T0 and T1, noting a decrease of nine points in the median score of the Resvech scale, meaning a change of compromise from moderate to slight; in T2, 25% of the participants had healed and in T4, process stagnation was observed in patients with large wounds and with associated complications; at the same time, maintained inflammation of the affected lower limb and decompensation in their comorbidities were evidenced.

Graphic 1 Evolution of cicatrization of 80 patients diagnosed with ulcer of venous etiology, according to the moment of measurement and size of wound
Upon analyzing cicatrization in function of time, it was observed that 48.8% of the patients (52.5% of the women and 38.1% of the men, p ≤0.01) had cicatrization success of the wound in a maximum time of 90 days. Wounds located on the dorsal remained for a longer time (median of 113.5 days) and wounds located in the anterior median third of the limb healed faster (median of 48 days).
The Kaplan-Meier method was used to obtain the estimations of the cicatrization process from each of the evaluations of the 80 patients, of which 71 had cicatrization and nine were censored (due to loss and due to not presenting the event upon ending the follow up). The variable of follow up time had abnormal behavior of the data (Shapiro-Wilk test <0.0001). It was found that the median of the cicatrization time was 78 days (minimum = 14 days and maximum = 264 days, percentile 25 = 48 days and percentile 75 = 130 days). Graphic 2 shows the cicatrization in function of time, which exposes that the probability of an individual to healing increases over time.
To establish the variables that should be entered into the Cox proportional risk model, comparison was made of the cicatrization time with the variables dichotomized through the Logrank and Wilcoxon-Breslow tests. The first test was used when the graphics suggested differences in survival of the groups compared, the second test was used to find the statistic when it was not possible to establish that difference among groups. The variables shown in Table 4 were finally selected.
Table 4 Variables with potential to be included in the Cox proportional risk model of 80 patients diagnosed with ulcer of venous etiology.

Thereafter, the Cox proportional risk model was conducted to study the multivariate effect on cicatrization over time. Several models were run, according to the variables candidates for input into the model and the final risk model was constructed with the Breslow method. The statistical software showed that the model is adequate ((2 <0.0001). The Cox proportional risk model (Table 5) showed that cicatrization in all the evaluation moments is affected by the variables of the lesion’s degree of compromise, nurse’s experience, and socioeconomic level; age, wound antiquity, and gender were included, given the individual effect and prior knowledge of modification these variables exert on the cicatrization times. As noted in Table 5, the cicatrization rate of the individuals with slight compromise of the wound was 1.7 times faster with respect to those who had high compromise, throughout the study time and upon adjusting for the other variables. The cicatrization rate of those treated by a nurse with five years and more de experience was double (HR = 2.1) compared with those who were cared by a nurse with less experience. Likewise, those in socioeconomic levels one or two took twice the time to heal in relation to those from socioeconomic levels three and above.
Discussion
In this study, participants with UVE were mostly females and were between the sixth and seventh decade of life, which has been described in literature.5,17 Marques18 stated that female prevalence is due to gestational disorder that lead to post-thrombotic syndrome, besides the high prevalence of varicose veins, although some studies (10,19 described among their participants a proportion of UVE in men above 50%.
This study found a cicatrization rate of 48.8% in 90 days or less. In light of this, Finlayson20) compared the effectiveness of some methods in treating ulcers of venous etiology and found a 10-week cicatrization median for participants using compression bandages and 14 weeks for those using compression stockings; also, Lozano21 proposed cicatrization times of 12 weeks when using multilayered compression bandage. In a systematic review, Borges22 describes better cicatrization times with the use of compression bandage with 30% healing of the wound in the first two weeks of treatment. The author also proposes that cicatrization times are dependent on the treatment used and characteristics of the wound. Regarding the stage of wound compromise, this study found prolonged cicatrization times when wound size was large and compromise was high. With relation to this, Finlayson20) also described more delay in cicatrization in wounds larger than 10 cm2, as in other studies23,24 referring to differences in cicatrization and prognosis when the wounds were bigger and had greater compromise on the tissue.
This study found that the experience of treating nurses determines the time and cicatrization success. Studies, like that by Adderley,25 have compared general nurses with specialists in treating wounds and have shown that the latter are more precise in identifying the lesion, diagnostic judgment, and suitability for treatment. In this regard, Ylonen26 described in a literature review that the treating nurses have knowledge gaps concerning the evaluation, physiology, and healing process, hence, the author cites the need to increase knowledge and nursing care, as well as continuous education to the patient.. With relation to the aforementioned, Zarchi27 warns on the treatment that the compression event should also be taught and perfected. Likewise, this author identified substantial variation in the pressure made by elastic and inelastic bandages when measuring the pressure exerted by different professionals who placed the bandages, finding that they had variable underestimations and overestimations in the pressure exerted. The author added that, because of its efficacy, well-established compressive therapy is the essential intervention to treat ulcers of venous etiology.
This research found better cicatrization times in participants from higher socioeconomic levels. With respect to this, Selvaraj10 exposed that patients belonging to low and middle socioeconomic levels, with non-professional occupations and who remained on their feet for extended periods or seated because of household work, agricultural work, and informal work, favored development of venous disease that in time could be complicated with UVE. Similarly, Marques18 found more prevalence of UVE in individuals from low socioeconomic levels, low income, and low educational level; some of these findings were also present in this research. To end, other risks exist associated to poor cicatrization, among them high body mass indices, poor nutrition, dietary intake low in fruits and vegetables and poor practice of physical activity.28 In fact, our findings also showed high prevalence of these risk factors in the participants.
This study concludes that cicatrization of UVE in a time ≤90 days was associated to slight compromise of the wound, which involves its size and stage of tissue affectation, the expertise of the treating nurse, and the socioeconomic level ≥3. According to these factors, and considering that UVE are a multi-causal manifestation, we need to promote the relationship between knowing and doing in caring for individuals with ulcer of venous etiology, and it is recommended to emphasize during the formation of future nurses and during continuous education of those who are already professionals the theoretical and practical settings of prevention and treatment of UVE, which will contribute to improving the quality of care for the person with this health problem.29)
Limitations
Some of the data of the evaluations was obtained from the clinical history or comments by the treating nurse, which can offer variation in the results. Although various confounding factors were considered and multivariate analyses were performed with adjustments by the risk factors established, the possibility exists that using different technological dressings to favor the wound bed affects the results.











 text in
text in 





