Introduction
Since March 11, 2020, the World Health Organization (WHO) initially declared the COVID-19 as an epidemic; a public health emergency of international concern that later turned into a pandemic. This pandemic, with a viral origin, has a lethality of 3.4% according to the WHO 1. COVID-19 had an impact on the global population that may lead to physical and mental health consequences, including insomnia, anger, fear of getting infected, social isolation, development of increase of pre-existing disorders such as post-traumatic stress, anxiety, or depression 2.
In Colombia, the main measures to reduce transmission and avoid a collapse in the health system were social isolation, limited mobility, and quarantine. These measures are the most effective as well as the ones with a higher impact on the population. To determine the psychological consequences of the pandemic, individual characteristics such as tendency to anxiety, intolerance to uncertainty, perceived vulnerability to illness, lack or an excess of information, which may increase worries and frustration, must be evaluated 3. People were forced to adopt new customs and habits, leaving aside others, and generating changes in the family, work, social, and academic context to adapt to the new conditions. Similarly, new virtual tools were introduced to promote a return to the daily routine under biosecurity conditions 3.
Older adults were part of the COVID-19 risk group, given that they present a higher chance of death due to prevalence of fragility, disability, and dependency, in addition to pre-existing comorbidities and geriatric syndromes 4-5. Therefore, the Colombian Ministry of Health and Social Protection 6 recommended preventive isolation, with limitation of visits and contact with friends, family members, and/or caregivers. Prieto et al. 7 carried out an investigation four months after the beginning of the pandemic and found that one of the populations most affected by the restrictions in the access to the health system, physical therapies and continuity of medical treatments are those with chronic diseases, since they require of a routine of hospital visits for evaluations and drug dose adjustments 8. Changes in these caused an additional stress, as well as the fear of possible transmission during access to health services 7.
Parkinson's disease (PD) is the second most common neurodegenerative disorder after Alzheimer's 9. Its incidence increases with age and leads to physical and cognitive disability in the most advanced stages of the disease 10-11. It's estimated that the prevalence in Colombia is between 60 and 70 per 100.000 inhabitants 11. This increase is due to factors such as the aging of the population, exposure to environmental risk factors, as well as improvement in the diagnosis and report of the disease. The situation of the COVID-19 pandemic presented big challenges for patients with PD, leading to changes in the access to the health system, the practice of exercise or leisure activities, relationship with peers, and mental health care.
Furthermore, Navarta-Sánchez et al. 12 identified three aspects that affect how patients and their families confront with the disease. These include medical attention, family environment, and acceptance of the disease, which can be influenced by religious beliefs or optimistic and positive personalities. Additionally, factors such as the severity of the disease 13 and the age of the patient are also predictors of disease adaptation.
Cilia et al. 14 suggest that patients with PD are more vulnerable than the general population due to factors related to the disease, such as its long duration and comorbidities associated with age. Moreover, Prasad et al. 7 indicate there is no evidence that patients with PD are more vulnerable to COVID-19 contagion or have worse results, although them and their caretakers have different opinions about it.
Quality of life (QoL), as defined by the WHO, refers to how the individuals perceive their position in life and the value systems they adhere to 13. Regarding PD patients, there is evidence of deterioration in their QoL attributed to factors such as disease stage and duration, disability, cognitive impairment, motor disorders 15, postural instability, and difficulty in multitasking 16. These characteristics contribute to dependency, preventing patients from performing daily activities independently, affecting their QoL 6.
Depression and anxiety are the main psychological conditions associated with the COVID-19 pandemic in these patients. Rodriguez-Carrillo and Ibarra 15 reported that 40% of patients with PD experience anxiety disorders exacerbated by the pandemic. The se conditions contribute to increase difficulties and freezing of gait, causing a negative impact on their quality of life. Additionally, they noted that between 20-35% of patients may present depressive symptoms, which are among the factors most detrimental to their overall well-being.
The management of the disease was limited by public health recommendations during the COVID-19 pandemic, which is why patients had to seek tele-consultation to continue their treatment. Many also faced interruptions in care from specialized centers and experienced a considerable reduction in physical activity 17. For the QoL assessment in these patients, it's necessary to explore the perception of the patient on their physical and mental status, as well as their ability to evaluate the impact of the symptoms on their functionality. These patient-reported insights serve as crucial indicators of their health status, distinct from the medical interpretation of symptoms 14.
The caregiver figure plays a crucial role in managing PD when patients experience loss of functionality and autonomy. Typically assumed by a family member, this role involves direct participation in providing instrumental support for the patient's recovery and well-being. In Colombia, however, there is a recognized deficiency in the ability to care for these patients, as there are no public health policies that guarantee rehabilitation and adding the high costs, most patients cannot have a follow-up with a neurologist or assist to educational programs. Additionally, the shortage of neurologists further complicates the situation 16.
To address these gaps, the establishment of clinical communities is proposed as a strategy. These communities consist of multidisciplinary teams organized around the patient, aiming to provide comprehensive care including medical management, education, support, follow-up, hospitalization, outpatient care, rehabilitation, and support services 16.
Given the chronic nature of PD and its impact on both motor and non-motor domains, it's crucial to encourage physical activity, leisure activities and regular disease monitoring among these patients. Physical activity is particularly significant as it helps reduce stress 17 and supports the maintenance and improvement of mobility, balance, posture, motor performance and reduce fall risk 18.
However, the COVID-19 restrictive measures implemented by the Colombian government limited outdoor physical activity, attendance to therapies, and regular medical check-ups for patients with PD. Therefore, our goal was to assess the emotional status and quality of life of patients with PD that belong to the program Saturday in Motion, as well as to explore what was the patient's perception of quality of life related to the COVID-19 pandemic.
Materials and methods
Participants
The sample included 12 participants aged between 65 and 78 years, who were conveniently selected from the Saturday in Motion program 16 between July and August 2021. The inclusion criteria were a) clinical diagnose of PD; b) receiving medical treatment; c) classified between the stages 1 and 3 on the Hoehn and Yahr scale; and d) not using mobility aid.
All participants completed the Beck Anxiety Inventory (BAI), Patient Health Questionnaire (PHQ-9), and the Parkinson's Disease Questionnaire (PDQ-39), to assess mood disorders and quality of life. Recruitment took place during a regular virtual session of the Saturday in Motion program, where the project was introduced and the participants were invited to join the research voluntarily. Self-reporting questionnaires and semi-structured interviews were conducted via Zoom, with each sessions lasting no longer than 2 hours and facilitated by two researchers. All patients provided consent for session recordings.
The participants who agreed to take part in this study did so voluntarily and without financial remuneration. They digitally signed the informed consent form, which was approved by the Institutional Ethics Committee of the Faculty of Social Sciences of the Pontificia Universidad Javeriana Cali. The study adhered to international ethical recommendations, including the Helsinki Agreement, and complied with Resolution 8430 of 1993 from the Colombian Ministry of Health and Social Protection.
Data analysis
A mixed methodology was employed, comprising a non-experimental design for the quantitative component and a phenomenological design for the qualitative component. Data for the qualitative component were collected through semi-structured interviews (Appendix 3), which explored five 5 categories related to the COVID-19 pandemic: social domain, caregivers, adaptation strategies, disease management, and leisure activities of the participants. The description of these categories is provided in table 1.
Table 1 Definition of the analysis categories
| Category | Definition |
|---|---|
| COVID-19 pandemic | A pandemic is defined as the global spread of a new disease 19. The WHO declared COVID-19 a pandemic once cases were reported on all continents. |
| Caregivers | Is the person directly involved in the care, recovery, and well-being of the patient, often assumed by a family member. Their responsibilities include providing support, delivering care at home, and making decisions about patient care. |
| Adaptation strategies | Process by which a group or individual modifies their behavioral patterns to adjust to the rules established in the social context they are in. |
| Management of the disease | The management of Parkinson's disease involves different aspects, including pharmacological and non-pharmacological treatments, which depend on the patient's clinical characteristics, lifestyle, access to resources and the will of the patient. |
| Leisure activities | They are defined as the activities or tasks people perform in their free time. Among which are physical activities such as walking, functional exercises or dancing. |
Source: Own elaboration.
In the quantitative component, descriptive analyses (mean, standard deviation, median and interquartile range) were used for the sociodemographic and clinical variables, according to normal or non normal distribution. Data analysis was conducted using IBM SPSS v28 software.
For the qualitative component, discourse analysis was performed using the categories previously defined with the ATLAS.Ti Cloud Software. All of information was analyzed and data triangulation was conducted to enhance the comprehensiveness of the findings.
Results
The total sample comprised 12 patients, with 75% being men and 25% women, with a median ages of 75 years (SD = 2.9) and 71 years (SD=6), respectively. The mean years since diagnosis for men and women were 9 (SD=4.6 and 3.6, respectively). 89% of men lived with their wives, while 67% of women lived with one of their children (table 2).
Table 2 Description of the sample sociodemographic data
| N=12 | ||
|---|---|---|
| Men | Women | |
| 9(75%) | 3(25%) | |
| Age | 75(±2,9) | 71(± 6) |
| Years of diagnosis | 9(± 4,6) | 9(± 3,6) |
| Level of education | ||
| High School | 3(33%) | 1(33%) |
| University | 4(44%) | 1(33%) |
| Postgraduate | 3(33%) | 1(33%) |
| Who they live with | ||
| Partner | 8(89%) | 1(33%) |
| Siblings | 1(11%) | 0(0%) |
| Children | 0(0%) | 2(67%) |
Source: Own elaboration.
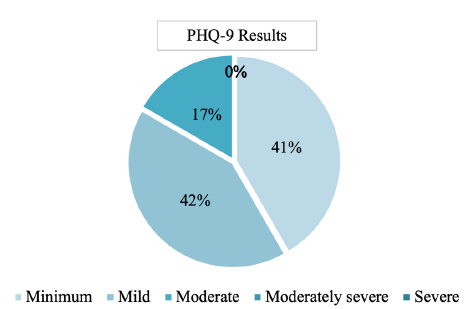
Regarding the emotional state scales, Figure 1 shows that 50% of patients presented mild levels of anxiety, while 5% showed minimal levels of anxiety.
Source: Own elaboration.
Figure 1 Description of the anxiety level based on Beck Anxiety Inventory (BAI) scale
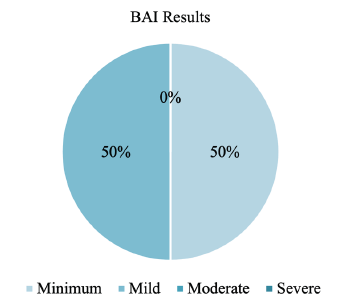
Similarly, Figure 2 illustrates that 41% of patients presented mild depressive symptoms; 41%, had severe depressive symptoms, and 17% showed moderate symptoms.
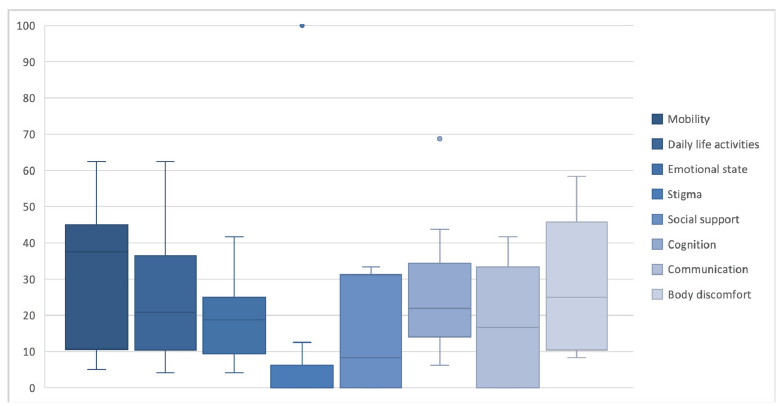
Moreover, Figure 3 shows the distribution of the dimensions of PD Questionnaire (PDQ-39). According to the table, the greatest compromise in QoL is due to mobility, which imposes the most limitations, with a median of 37.5 (IQR 10.6-45), followed by body discomfort with a median of 25 (IQR 10.445.8) and cognition, with a median of 21.87 (IQR 14-34.3).
Source: Own elaboration.
Figure 3 Distribution of each of the dimensions of quality of life in the PDQ-39 according to the sample of patients
Source: Own elaboration.
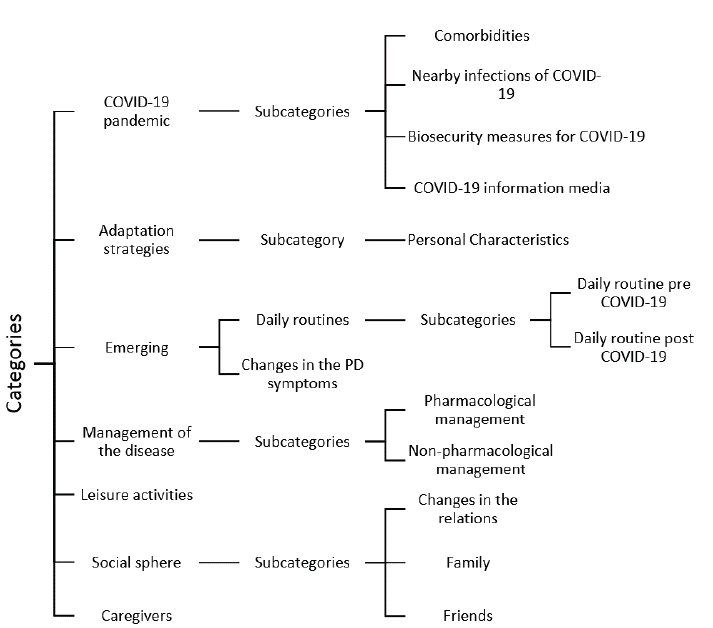
Figure 4 Categories, subcategories, and emergent categories of analysis of the qualitative phase
On the other hand, the dimensions of stigma with a median of 0.00 (IQR 0-6.2) and social support with a median of 8.3 (IQR 8.3-31.2), have the least impact in patients regarding their symptomatology and quality of life. However, there was an outlier in the stigma dimension where one patient scored 100. Despite being diagnosed 14 years ago, this patient was affected by the tendency to hide the disease by avoiding going out to public places and being seen, which causes a feeling of shame and concern about others' reactions.
The analysis categories initially proposed for the semi-structured interviews in the research method are shown in table 1. However, during the interviews, additional subcategories and emerging categories emerged.
Subsequently, table 3 delineates the analysis categories, subcategories, and excerpts that, following data analysis, depict and encapsulate the patients' perspective on each category.
Table 3 Results obtained by interviews
| Category | Subcategory | Fragment |
|---|---|---|
| COVID-19 pandemic | - "It was a total restriction of life" (S3) | |
| Adaptation strategies | Personal characteristics | - "Feeling locked in a room without communication or in the house itself was exasperating" (S11). |
| Daily routines | Daily routine post COVID-19 | - "Well, my life changed since the moment of Parkinson's; I started not to go out, to be calmer and the pandemic finished me off" (S10) |
| Changes in the PD symptoms | - "I have worsened mainly in motor symptoms, I have difficulty to stand up, I walk with difficulty as well, before I did not" (S7). | |
| Disease management | Non-pharmacological management | - "It was discontinued completely, because at the beginning with the restrictions there was no way to mobilize, and when we started to have more freedom, it was recommended not to go to the hospital, as it is a place with saturation of patients, agglomeration and in that sense, it is better not to seek therapy there" (S5). |
| Pharmacological treatment | - "There was no in-site follow-up, it was all by phone and my husband always told the doctor he was okay, they would give him the formula and that was it" (S12). | |
| Leisure activities | - "Logically, the stay at home meant a decrease of mobility; I hardly exercised, not because I could not do it, but because I felt lazy, the habit of staying in bed changed, you no longer wanted to get up to exercise" (S11). | |
| Social sphere | Family | - "I needed to go out, but my kids wanted to protect me, (...) and they would say "I will do this for you, so you do not have to go out", I don't like that, I like going out, the same can happen to her and to me" (S4). |
| Friends | - "We used to go for walks, but that's over now, we have to stay here alone" (S6). | |
| Caregivers | - "My caregiver, my wife, she has been my right hand, she's always attentive and knows when to pick the medicines, she schedules medical appointments, as well with the physiotherapist and was aware of the exercises and would repeat them for me" (S2). |
Source: Own elaboration.
Discussion
The purpose of this research was to characterize the emotional state and quality of life of patients with PD participating in the Saturday in Motion program 16, as well as explore their perception of quality of life during the COVID-19 pandemic. This research revealed anxiety levels ranging from minimal to mild, despite what was described in different studies, where it is indicated that the additional stress produced by the changes was caused by the pandemic situation, and could have been a trigger of their symptoms 15,20. Interviews supported these findings, indicating that most patients did not struggle with adopting preventive measures against contagion due to existing coping strategies and adjustments related to aging, their diagnosis and comorbidities. These findings align with the observations of Navarta-Sánchez et al. 12, regarding changes in the activities and daily routines among patients with PD.
Most patients exhibited minimal and mild levels of depression, with 17% experiencing moderate symptoms, which could potentially affect quality of life negatively. This observation aligns with findings by Pezoa-Jares 21, who identified depression as one of the most frequent neuropsychiatric alterations in patients with PD, that additionally, may worsen over time. Similarly, Rodríguez-Carrillo and Ibarra 15 suggest that depression is one of the factors that most affects the quality of life of these patients.
In our patient sample, we identified that the duration of the disease was not a decisive factor in the perception of QoL, which contrasts with the results obtained by Martínez-Jurado et al. 22, who reported that QoL deterioration was influenced by disease duration. Specifically, the observed that patients with less than five years since diagnosis experienced a major compromise of the QoL compared to those diagnosed for more than ten years. These differences may be associated with clinical variables such as age of onset, disease subtypes, progression and pharmacological treatment.
According to our results, the three dimensions that had the greatest impact on QoL were mobility, wihich aligns with findings from Arango et al. 23 and Palacios et al. 10; body discomfort; and cognition, although the latter contrast with the findings of Saavedra et al. 11. This discrepancy may be linked to the negative perception of cognition, which can be worsened by depressive and anxious symptoms, the CO-VID-19 pandemic situation, or even by the advanced age of the patients and progression of the disease. These dimensions significantly impair life activities, thereby contributing to a deterioration of QoL 10.
According to Avendaño-Avendaño et al. 24 and Palacios et al. 10, our results showed that the social support dimension affected the overall QoL score. For example, during the interviews, patients often indicated having a primary caregiver, in most cases the spouse or a Haga clic o pulse aquí para escribir texto.support system of friends and family, who provided companionship, recreational spaces and management for the development of activities related to the control of their disease.
Amid the COVID-19 pandemic, families supported patients by procuring medication and food, offering emotional support, facilitating technology for family meetings, and assisting with teleconsultations. This proved to be a useful and efficient tool in maintaining continuity in medical management 25.
Similarly, pharmacological management in most cases was uninterrupted, attributed to the involvement of caregivers and/or family members who assisted in procuring medication and accessing teleconsultation, providing both emotional and practical support 26. Some patients reported that their physicians adjusted their medication doses in response to the increased symptoms.
Regarding the assessment of the QoL perception during COVID-19 pandemic through semi-structured interviews, two important aspects were identified: firstly, patients presented a wide knowledge of the SARS-CoV-2 virus, which allowed them to identify the symptoms and adhere to biosafety measures to prevent infection. Secondly, patients identified themselves as being at risk for COVID-19, not solely due to the PD diagnosis, but also because of their age and preexisting comorbidities, which could increase complications if they were to contract the virus 1.
Likewise, it was observed that the perception of QoL did not significantly changed during the COVID-19 pandemic, possibly because patients had a median of 9 years of diagnosis since diagnosis, allowing them to regularly assess and adapt to the impact of symptoms on their QoL. Thus, patients' perception of their QoL could be considered indicative of their mental state 27.
During interviews, patients did not directly attribute changes in symptomatology or increases in motor and/or cognitive symptoms to the COVID-19 pandemic. They acknowledge PD as a neurodegenerative and progressive condition with multiple motor and non-motor symptoms. This awareness enable them to differentiate between symptoms inherent to the disease and those exacerbated by external factors such as the pandemic. Consequently, patients described an enhanced awareness of their disease, increased knowledge about it, and a sense of empowerment assuming an active role in managing their condition.
Empowered patients demonstrated greater adherence to treatment, emphasizing the importance of non-pharmacological strategies in symptom management, and incorporating various activities into their daily routines. Additionally, patients highlighted the importance of music as complementary therapy, finding it beneficial for initiating gait, improving motor symptoms, balance, and posture 18. Moreover, they noted that music decreased stress and provided entertainment, making it a valuable leisure activity.
Patients largely attribute the increase in their symptoms to administrative and logistical difficulties. Initially, government restrictions and later self-care measures during the reactivation process led to reduced availability of physical therapies and/or activities. This situation also resulted in interruptions to specialists follow-ups due to the difficulty to adapt to technology, as well as difficulties accessing the healthcare system. These challenges included transportation to hospitals, in-person appointments, and restrictions on facility access due to the pandemic 8,28.
Although preventive measures slowly allowed going back to the activities, many patients delayed reintroducing recreational activities into their daily routines. Among the identified causes of increased symptoms were disruptions to routines, fear of contagion, and prohibitions made by family members and/or caregivers. However, patients identified that once they resumed their leisure activities, symptoms that had exacerbated during their inactivity improved or decrease, consistent with findings by Feeney et al. 29.
The return to on-site appointments allowed treating physicians to perform more thorough evaluations, conduct physical examinations, and make informed decisions regarding treatment based on changes in symptoms.
Additionally, regarding perceptions of isolation, it was found that the circumstances of the pandemic and changes in personal relationships were mediated by adaptation strategies. Patients utilized acceptance of the situation, resilience, and flexibility to recognize the COVID-19 pandemic as a stressful event. This encouraged modifications in their daily life activities with the goal to prevent and mitigate possible contagion, causing changes both in the familiar and social context 3, also in the medical settings and adaptation to biosafety measures.
To summarize, the pandemic presented a challenge for patients with PD. Nevertheless, they found ways to adapt with support from their families, caregivers, and physicians, as well as through participation in patients groups. These spaces, even in virtual formats, promoted recreation and continuity through educational talks, conferences and activities with different specialists, allowing support in the adaptation process both in patients and caregivers to the pandemic context.
In conclusion, QoL comprises eight dynamic dimensions that are influenced by individual characteristics and environmental changes. Hence, it is challenging to fit in a single aspect of what is determined as QoL. The subjective perspective holds a high value in comprehending the impact of the COVID-19 pandemic on patients with chronic and disabling conditions like PD. Through interviews, insights were gained into patient's perception of QoL during the pandemic. In addition, emerging categories and subcategories provided deeper insights into the personal experiences of each individual with PD during this challenging period.
Lastly, the limitations of this study were mainly centered on the size of the sample, underscoring the need to carry out a study with a larger number of patients to obtain more information on the QoL concerning the experience of COVID-19. While socioeconomic variables were not within the scope of this research, they are crucial considerations, as patients mentioned challenges such as accessing the healthcare system, medication, and transportation, which initially generated expectations upon the change in medical attention given due to the pandemic situation.
Moving forward, it is essential to carry out a follow-up studies to assess how external variables impact PD and its effects on QoL, particularly in managing these patients in the post-pandemic period.